Main complaints in the presence of venous insufficiency
- a state of stupor and lethargy (compared to the state of being hit on the head with a pillow);
- decreased vision;
- swelling and numbness in the facial area;
- heaviness in the back of the head (due to the fact that it is there that the venous pathways converge and then flow into the internal jugular vein system);
- tinnitus (associated with venous stagnation in the inner ear, the pressure created irritates the auditory nerve, as a result of which a person experiences this symptom). Neurologists most often deal with this problem by prescribing medications, but treatment turns out to be ineffective, because the cause is not eliminated and the effect of the drugs is temporary.
Disease severity
Disruption of the outflow of venous blood from the brain is a very dangerous condition, therefore, to fully study and treat it, it is divided into several types of severity:
- In the first degree, there are almost no symptoms, and the disease is diagnosed as part of a routine study of the brain or if it has been examined for tumors and neoplasms. This type of disease is a consequence of hypertension, solar activity or light blows to the head.
- In the second degree of the disease, the symptoms are not clearly expressed; moreover, they are usually attributed to fatigue and poor sleep. Headache occurs rarely, and a person does not attach any importance to it. This type of pathology occurs as a result of severe trauma and is chronic in nature.
- With venous encephalopathy or the third degree of severity of the disease, the symptoms appear completely, the person’s condition is assessed as serious. The change in blood circulation in this case affects all areas of the brain. If this form of the disease is left untreated, then in addition to the failure of arms, legs, vision and hearing, a person may experience dementia and other serious consequences.
Treatment of cerebral venous outflow disorders
In a situation where a patient is diagnosed with a violation of venous outflow, he is prescribed venotonics and other vascular drugs. But this measure is temporary, as mentioned above. As soon as the medication is stopped, the complaints return. The answer to the question: “How can this be?” is very simple: “Because the cause of the disease has not been eliminated.”
In this situation, osteopathic treatment is, literally, salvation, because the doctor works with the root cause of the disease. First of all, the osteopath eliminates the disorders visible to him:
- normalizes muscle tone, because Hypertonicity can cause compression of the veins and disrupt the outflow.
- eliminates the slightest displacement of skull structures;
- restores the correct position of the vertebrae.
Most patients, after starting treatment, note increased strength, improved sleep and memory, and a feeling of lightness in the body. But there are situations when after the first session the condition may worsen. But, we hasten to reassure you, this is temporary. Let's explain why this happens. When any problem arises, our body tries to independently adapt to new circumstances, i.e. compensation processes are launched. If a person turns to an osteopath at the beginning of a problem, then most likely he will not experience any discomfort after the session, because The body has not yet had time to rebuild. If the problem has been developing for years, then there is a high probability that after the first visit to an osteopath the condition may worsen somewhat, because the body must get used to the “rearrangement”. Malaise, as a rule, lasts a couple of days, then the condition improves and the body heals itself.
Dear patients, remember that you do not have to endure and wait for the body to cope with the disease on its own. Take action and help your body. And there will be health and harmony in your life. It’s not for nothing that they say that in a healthy body there is a healthy mind
Algorithm for diagnosis and treatment of chronic forms of venous circulation disorders
In the Russian Federation, 35–38 million people suffer from chronic venous insufficiency. Unfortunately, the stereotype according to which venous pathology is considered only a surgical pathology has led to the fact that a huge number of patients do not receive adequate medical care [1]. At the same time, changes in venous circulation are one of the important pathogenetic mechanisms for the development of vascular diseases of the brain.
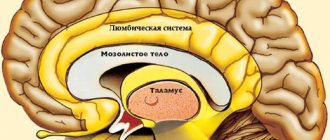
Regional changes in the tone of intracranial veins lead to venous congestion and impaired cerebral circulation in atherosclerotic lesions of cerebral vessels, arterial hypertension (AH) and hypotension, chronic lung diseases, and cardiac pathology. It has been recorded that in 15% of patients with hypertension, compression of the jugular, brachiocephalic and vertebral veins is recorded, signs of impaired venous outflow of the brain occur in 91% of cases of hypertension, and in patients with stage 1-2 hypertension - in 55% of cases [2, 3] . At the same time, the compensatory capabilities of the brain and its circulatory system are so great that even serious difficulties in the outflow of venous blood may not cause clinical manifestations of increased intracranial pressure and impaired brain function for a long time [4], so early diagnosis of this pathology causes certain difficulties.
To simplify the doctor’s work, the following algorithm for diagnosing and treating chronic forms of venous circulation disorders can be used.
Algorithm for diagnosis and treatment of chronic forms of venous circulation disorders
Step 1. Identify risk factors
The doctor should always remember that venous congestion in the vast majority of cases is secondary in nature, that is, it occurs as a symptom of an underlying disease that impedes the outflow of venous blood from the cranial cavity. Therefore, diagnosis first of all involves identifying the underlying disease (Table 1).
Obstruction of venous outflow from the cranial cavity is observed in a number of diseases [5]:
- cardiac and cardiopulmonary failure;
- common pulmonary tuberculosis, pulmonary emphysema, bronchiectasis, bronchial asthma, pneumothorax;
- compression of extracranial veins - internal jugular, innominate, superior cava - by a neoplasm in the neck, aneurysm; hypertrophied neck muscles in reflex-muscular-tonic syndromes of cervical osteochondrosis;
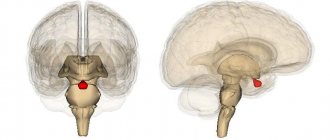
- tumors of the brain, its membranes, and skull;
- thrombosis of veins and sinuses, infectious-toxic lesions of veins, cerebral thrombophlebitis;
- compression of the veins during craniostenosis (premature fusion of the sutures between the bones of the skull with compression, in particular, of the jugular veins), in these conditions the venous collectors dilate compensatoryly;
- asphyxia of newborns and adults;
- venous and arteriovenous hypertension;
- when nasal breathing stops;
- infectious and toxic lesions of the brain;
- with the consequences of traumatic brain injuries;
- epilepsy.
Diseases that cause disruption of venous outflow are given in Table. 1.
In addition, the development of venous encephalopathy may also be due to the classical causes of cerebrovascular pathology: hypertension, atherosclerosis, smoking, diabetes, use of hormonal drugs (estrogens), alcohol and drug abuse, use of nitrates and some vasodilators (nicotinic acid, papaverine). Venous outflow can also be impaired under physiological conditions, for example, when straining, during a prolonged cough, during physical stress, singing, playing wind instruments, childbirth, screaming, bending the head (for example, during physical exercise), in a lying position without pillows under the head, when the neck is compressed by a tight collar.
Step 2. Analysis of complaints and medical history
Disturbances of venous circulation, as a rule, are genetically determined. Currently, the role of the initial tone of the veins in the formation of venous discirculation is undeniable. Constitutional and hereditary factors are key for the development of venous dysgemia [6]. Patients with a family “venous” history usually have several typical manifestations of constitutional venous insufficiency - varicose veins or phlebothrombosis of the lower extremities, hemorrhoids, varicocele, impaired venous outflow from the cranial cavity, esophageal varicose veins. Pregnancy is often the trigger.
Typical complaints:
- morning or afternoon headache of varying intensity;
- dizziness, depending on changes in body position;
- noise in the head or ears;
- visual disturbances (decreased visual acuity, photopsia);
- “tight collar” symptom - increased symptoms when wearing tight collars or ties;
- “high pillow” symptom - increased symptoms when sleeping with a low headboard;
- sleep disorders;
- feeling of discomfort, “fatigue” in the eyes in the morning (symptom of “sand in the eyes”);
- pastiness of the face and eyelids in the morning (with a pale, purple-cyanotic tint);
- mild nasal congestion (outside the symptoms of acute respiratory infections);
- darkening of the eyes, fainting;
- numbness of the limbs.
The course of the disease has chronic, episodic and remitting variants.
Step 3. Examination of the patient
When examining the patient, a “venous triad” is detected:
1) swelling of the face in the morning after a night's sleep, which decreases significantly in the evening with sufficient physical activity; 2) cyanosis of the facial skin; 3) expansion of the saphenous veins of the neck and face.
With severe venous stagnation, patients are unable to lower their heads and remain in a horizontal position for a long time. Blood pressure (BP) in such patients is usually within normal limits, venous pressure ranges from 55 to 80 mmH2O. Art. A low difference between systolic and diastolic pressure is characteristic, in contrast to hypertension. In severe cases, epileptic seizures and mental disorders are possible [7]. Venous discirculation is characterized by a decrease in corneal reflexes. On palpation, pain is detected at the exit points of the first, less often the second, branches of the trigeminal nerve (“transverse sinus syndrome”) with the formation of hypoesthesia in the innervation zone of the first branch of the trigeminal nerve, which is probably associated with the development of neuropathy caused by venous stagnation and impaired microcirculation in the vaza system nervorum [8].
According to the type of prevailing symptom, the following variants of chronic venous insufficiency (encephalopathy) are distinguished: cephalgic, hypertensive (pseudotumorous), bettolepsy, polymorphic (scattered small-focal brain damage), sleep apnea syndrome, psychopathological/asthenovegetative [9].
Cephalgic syndrome is the most common clinical manifestation of the pathology of the venous system. As a rule, headaches increase when moving the head to the sides, changes in atmospheric pressure, changes in ambient temperature, after excitement, drinking alcohol, etc. This syndrome has a number of characteristic signs (Table 2).
Hypertension (pseudotumor syndrome) is characterized by clinical signs of increased intracranial pressure (ICP) in the absence of focal neurological symptoms and the presence of congestive optic discs [10]. Develops acutely. Patients, as a rule, complain of intense paroxysmal headaches, are euphoric, irritable, and often angry. Bradypsychism appears with slowness of movements. When examining the cerebrospinal fluid, increased pressure attracts attention. The protein content is slightly increased or normal, cytosis is not increased, serological reactions are negative. Pseudotumor syndrome in chronic venous pathology must be carefully differentiated from brain tumors.
Bettolepsy (cough syncope) is the development of short-term fainting with convulsive twitching during a coughing attack. Cases of “cough” fainting (bettolepsy) are quite rare and account for no more than 2% of patients with venous pathology. This form of venous blood flow disorder develops when:
- chronic bronchitis;
- emphysema;
- pneumosclerosis;
- bronchial asthma;
- cardiopulmonary failure.
In the pathogenesis, the main role is played by brain hypoxia, which occurs during a prolonged cough, caused by an increase in intrapleural pressure, disruption of venous blood flow in the superior vena cava system, a slowdown in pulmonary blood flow with an increase in intrapleural pressure, with a decrease in the filling of the left ventricle with blood, a slowdown in cardiac activity, and a decrease in cardiac output. . In most cases, paroxysms during coughing are not related to epilepsy, since they develop according to pathogenetic mechanisms characteristic of fainting conditions. Coughing attacks occur in patients while sitting or standing, often during or shortly after eating. Provoking factors: cold air, pungent odor, tobacco smoke, excessive laughter, etc. Simultaneously with the cough, facial hyperemia develops, followed by cyanosis with pronounced swelling of the neck veins. Usually there are no warning signs, there may only be slight dizziness. Loss of consciousness occurs within the first minute from the onset of coughing. The duration of syncope varies from several seconds to a minute. Cyanosis appears, patients often fall, often hurt themselves, the cough stops, the color of the face changes from cyanotic to marble-pale. Seizures are usually not observed (sometimes tonic seizures are possible). There is no tongue biting or involuntary urination.
Bettolepsy is observed mainly in older people with chronic diseases of the respiratory tract and lungs (pharyngitis, laryngitis, emphysema, bronchial asthma, etc.). At a younger age, the appearance of fainting when coughing is observed quite rarely, mainly in individuals with increased sensitivity of the carotid sinus, or with functional insufficiency of the mechanisms that support postural tone.
The syndrome of scattered small-focal brain lesions is clinically manifested by individual symptoms, such as asymmetry of the nasolabial folds, mild nystagmus, and slight staggering when walking. Motor, sensory, and coordination disorders are less common. Parkinson-like syndrome may develop [11].
Psychopathological and asthenovegetative syndromes are the earliest signs of venous insufficiency. They are characterized by increased fatigue, irritability, unstable or bad mood, sleep disorders in the form of constant drowsiness or persistent insomnia, autonomic disorders (unpleasant sensations from the heart, shortness of breath, hyperhidrosis of the extremities). It is possible to develop hyperesthesia (intolerance to bright light, loud sounds, strong odors), intellectual disorders (disorders of attention and memory, ability to concentrate). Headaches are often observed. Patients experience a change in mental state depending on atmospheric pressure: when it falls, fatigue increases, irritable weakness, and hyperesthesia (Pirogov's symptom) increase. In rare cases, psychosis develops with delusions and visual and auditory hallucinations [12]. Determinants of asthenia are constant complaints of increased fatigue, weakness, exhaustion after minimal effort in combination with at least two of the following complaints:
- muscle pain;
- dizziness;
- tension headache;
- sleep disorders;
- inability to relax;
- irritability;
- dyspepsia.
The most characteristic signs of asthenic disorders can be divided into several groups depending on the dominant complaints [13].
1. Physical disorders:
- muscle weakness;
- decreased endurance.
2. Intellectual disorders:
- disorders of attention, ability to concentrate;
- Impaired memory and vigilance.
3. Psychological disorders:
- lack of self-confidence;
- decreased motivation.
4. Sexual disorders:
- lack of libido;
- decreased erection.
Psychopathological and asthenovegetative syndromes predominantly develop in young and middle-aged patients.
Sleep apnea syndrome. In patients with sleep apnea, the absence of a physiological nocturnal decrease in blood pressure and impaired cerebral venous hemodynamics have been established.
Step 4. Additional research methods
For more accurate diagnosis, instrumental research methods are used: ophthalmoscopy, skull radiography (craniography), ultrasound (US) methods for studying the venous system of the brain, computed tomography or magnetic resonance imaging, cerebral angiography. When conducting any diagnostic study, it is necessary to take into account that venous circulation is extremely labile, and this is associated with the state of central hemodynamics, the respiratory cycle, muscle activity, and posture. It is advisable to conduct the examination on days with a favorable geomagnetic situation, provided that the patient does not have an increase in blood pressure at the time of examination, or complaints of headache or a feeling of “heaviness” in the head during the last week. Patients should not drink alcohol for several days. In women of reproductive age, it is advisable to assess cerebral hemodynamics in the first half of the menstrual period.
Craniograms can reveal an increase in the vascular pattern, expansion of diploic veins, and venous outlets. Ophthalmological methods allow already in the early stages of vascular diseases of the brain, along with changes in the arteries, to detect the dilation of veins, their tortuosity, uneven caliber, and with a pronounced increase in intracranial pressure - congestion in the fundus. The methods of biomicroscopy of the conjunctiva of the eyeball and venous ophthalmodynamometry are quite informative. To clarify the causes and extent of impairment of venous outflow at the neck level, duplex ultrasound scanning (USDS), selective contrast venography, scintigraphy and computed tomography are used. Each of these methods has advantages and disadvantages. Ultrasound scanning makes it possible to reliably assess the speed of blood flow and the relationship of blood vessels with surrounding tissues, but has limitations since a relatively small area of the brachiocephalic veins is available for study. Selective contrast venography is associated with a certain risk when administering a contrast agent, which is often unjustified for this pathology [15]. Scintigraphy does not provide information about the structures surrounding the veins. Standard computed tomography allows assessing the diameter of the veins and their relationship with surrounding structures only in cross sections, but does not display the characteristics of blood flow, and in addition, is accompanied by radiation exposure. Magnetic resonance venography of the brain is characterized by a decrease in the intensity of the blood flow signal, up to its loss, in the superior sagittal sinus, great cerebral vein and straight sinus. It is also possible that there is a decrease in size or a complete absence of the signal from the blood flow along the transverse and sigmoid sinuses, the internal jugular vein of one of the hemispheres of the brain, combined with the expansion of these venous structures on the opposite side; expansion of emissary and superficial cerebral veins [16].
Step 5. Choice of therapy
Unfortunately, the issues of pharmacotherapy of cerebral venous circulation disorders still remain controversial and insufficiently studied; there is no doubt that, first of all, it is necessary to treat the underlying disease. The earliest possible energy correction can additionally affect the survival of neurons, reduce damage to brain tissue caused by chronic ischemia and hypoxia, and primarily affect the core of the asthenic syndrome - hypoergosis with increased exhaustion of mental functions [17]. Taking into account modern ideas about the pathogenesis of venous encephalopathy, the main efforts should be aimed at eliminating the following pathological factors:
1) normalization of the tone of the venous bed; 2) leukocyte aggression and inflammation; 3) correction of microcirculatory disorders; 4) increasing the capacity of the venous bed.
In the treatment of chronic disorders of venous blood flow at various stages, pharmaceutical drugs belonging to various groups (anticoagulants, agents that improve microcirculation, venotonics) are most often used. The spectrum of action of most drugs is quite narrow (dextrans affect blood rheology, antiplatelet agents reduce platelet aggregation activity, venotonics improve the tone of the venous wall, vasodilators enhance the hypotonic effect, etc.), therefore, to achieve an optimal therapeutic effect, it is necessary to use several drugs of different groups [ 2]. In recent years, there has been a search for an ideal drug for the treatment of disorders of cerebral venous circulation, which should affect as many pathogenetic links as possible, have a minimum number of side effects and high bioavailability. Naturally, the greatest interest is in drugs that have energy-correcting and microcirculatory mechanisms of action in the spectrum of their pharmacological activity with the maximum possibility of combination with venotonic drugs.
Treatment of venous circulation disorders
Clinical symptoms of brain damage in the initial stages of venous circulation disorders are minimal, but the microvasculature is already damaged, which leads to further progression of the pathological process, thus, the basic therapy is the prescription of drugs that have an angioprotective effect.
Angioprotectors
The first group of basic therapy is angioprotectors - drugs whose main effect is to restore vascular tone and their permeability. As a rule, they also have a multimodal mechanism of action.
One of these pharmacological agents is Actovegin, a drug that activates metabolism in tissues, improves trophism and stimulates regeneration processes. Of particular importance in its mechanism of action is the activating effect on the energy metabolism of cells of various organs [18]. This is due primarily to the ability to increase the uptake and utilization of glucose and oxygen, leading to improved aerobic energy production in the cell and oxygenation in the microcirculatory system. At the same time, anaerobic energy exchange in the vascular endothelium improves, accompanied by the release of endogenous substances with powerful vasodilating properties - prostacyclin and nitric oxide. As a result, organ perfusion improves and peripheral resistance decreases [19]. This mechanism ensures stabilization of the functional metabolism of tissues under conditions of temporarily induced stress and hypoxia in peripheral arterial disorders. Improvement in the processes of tissue utilization of oxygen and glucose is not isolated, but is associated with changes in the functional state of both the blood inflow pathways to the capillaries (arterioles) and the blood outflow pathways (postcapillary venules), as well as with changes in hemodynamic parameters at the capillary level [20].
A structural feature of precapillary arterioles is that there are no elastic elements in their wall, the number of smooth muscle elements is minimal, and neighboring muscle cells spiraling around the endothelial tube are located at a considerable distance from each other [21]. As a result, along the precapillary arterioles there are areas in which the vascular wall consists only of endothelial cells, outside of which there is a basement membrane, which allows them to be compared with venous vessels. Changes in the functional state of the microvascular bed, as an integral part of the cardiovascular system, affect the parameters of central hemodynamics, and, in particular, the venous system. There are probably also correlations between the functional state of the tone-forming links of microblood flow modulation and the level of blood pressure; a slight but significant decrease in diastolic (p < 0.03) and mean blood pressure (p < 0.04) is associated with a decrease in the tone of precapillary arterioles [22]. Considering the close relationship of metabolic and hemodynamic processes at the level of the microcirculatory bed, changes in the functional activity of all three tone-forming mechanisms of blood flow modulation, recent studies have proven the role of Actovegin as a corrector of microcirculation disorders [18–22]. The use of the drug resulted in a unidirectional change in the functional activity of all three tone-forming mechanisms of blood flow modulation, a significant increase in the amplitude (decrease in tone) of the myogenic rhythm on average for the group by 54% (p < 0.03) and the amplitude of the neurogenic rhythm by 50% (p < 0.003) ), and therefore Actovegin has a pronounced vasomotor component. An indicator of the metabolic activity of the microvascular endothelium is a decrease in the size of the pericapillary zone, which reflects the degree of hydration of the interstitial space. A significant decrease in the size of this zone against the background of the drug’s action confirmed that reabsorption processes predominate in the filtration-reabsorption metabolic mechanism. The filtration-reabsorption mechanism of exchange is directly related to the hemodynamic parameters of the blood flow, since it is based on the difference between the hydrostatic and colloid-osmotic pressure of the blood. Filtration processes are associated directly with the amplitude of pulse oscillations, which reflects the hemodynamic parameters of arterial blood flowing into the microcirculatory bed, and reabsorption processes with the amplitude of the venular rhythm. The results obtained during the study demonstrated the close relationship between metabolic processes and microhemodynamics and, as a final result, the possibility of using Actovegin as a means of basic therapy in patients with chronic forms of venous circulation disorders. The advantages of Actovegin include its low toxicity and good tolerability. The only contraindication to the use of the drug is hypersensitivity. Recommended regimen: 200 mg 2-3 times a day orally for a long period of 3-6 months. Courses can be held twice a year, preferably in spring and autumn.
In hospital settings, it is possible to prescribe the drug parenterally. The clinical effect is usually achieved gradually (within 3–4 weeks), and therefore the average duration of use is 1 to 3 months. Repeated courses of treatment are recommended.
Venotonics
The second group of basic therapy drugs are venotonics. Venotonics can be divided by origin into preparations from herbal raw materials and synthetic preparations.
Derivatives of ergot alkaloids (dihydroergotamine mesylate, ditamine, clavigrenin, ergotamine) are preparations from plant materials that have pronounced α1- and α2-adrenergic blocking activity, dilate peripheral vessels, increase venous tone.
Venoruton stimulates the release of endothelin from endothelial cells, which, by activating the endothelium-A receptors of the myocyte membrane, stimulates the contractile apparatus of the smooth muscles of the veins and increases the tone of the vascular wall.
Troxevasin increases the production of endothelin by endothelial cells, which, by activating endothelium-A receptors of the SMC membrane, stimulates the contractile reactions of venous myocytes and causes an increase in the tension of the vascular wall.
Detralex is a synthetic drug that reduces the distensibility of veins and venous stasis and reduces capillary permeability and increases resistance. In the presence of chronic venous circulation disorders, the maximum effect of treatment is ensured in combination with a certain, well-balanced lifestyle, in which it is recommended to avoid long exposure to the sun, reduce body weight, go for walks and, in some cases, wear special stockings that improve blood circulation.
Unfractionated and low molecular weight heparins increase the production of nitric oxide by endothelial cells, which leads to dilatation of the saphenous vein. In the portal vein, which has spontaneous phasic activity, heparins stimulate endothelial nitric oxide synthase, as a result of which the tone decreases and the frequency of phasic contractions decreases and, according to the mechanism of chronoinotropic dependence, the amplitude of phasic contractions of smooth muscles increases.
However, these drugs are used primarily for the treatment of varicose veins of the extremities or as a complement to the main treatment for venous encephalopathy.
Drugs for symptomatic treatment
Therapy for cephalgic syndrome, which often occurs in the form of tension headaches, consists of normalizing venous outflow by eliminating the increased tone of the pericranial muscles and benign intracranial hypertension. The drugs of choice in this case are muscle relaxants and diuretics.
The main diuretic drug is acetazolamide (Diacarb), used in a dosage of 250 mg 3 times a day. According to recent studies, the use of Diacarb can reduce the frequency and duration of sleep apnea by 6 months after taking it for 1 month [23]. Precautions must be taken when using acetazolamide.
- Use with caution in patients with a history of thromboembolic syndrome and in persons with pulmonary emphysema.
- The simultaneous use of Diacarb and acetisalicylic acid is not recommended.
- With long-term use, it is necessary to monitor the level of blood electrolytes, the number of platelets and leukocytes, as well as the acid-base status.
In conclusion, I would like to emphasize that chronic forms of venous circulation disorders are a common pathology in clinical practice today. It should be noted that making a diagnosis at the initial stages may not even require expensive diagnostic methods; it is sufficient to carry out a thorough analysis of complaints and the clinical picture at the stage of the patient’s first treatment. Identification of characteristic “venous complaints” allows for timely complex therapy including drugs that have a venotonic effect with an adequate treatment period (at least three months), which will minimize pathological changes in the venous bed and eliminate the phenomena of cerebral ischemia and hypoxia.
Literature
- Belova L. A. Venous cerebral discirculation in chronic cerebral ischemia: clinical picture, diagnosis, treatment // Neurological Bulletin. 2010. T. XLII, issue. 2, p. 62–67.
- Mishchenko T. S., Zdesenko I. V., Mishchenko V. N. Therapeutic possibilities for the treatment of cerebral venous disorders // International Neurological Journal. 2011, 1, p. 39.
- Savelyeva L. A., Tulupov A. A. Features of venous outflow from the brain, according to magnetic resonance angiography // Bulletin of the Novosibirsk State University. Series: Biology, clinical medicine. 2009. T. 7, issue. 1, p. 36–40.
- Svistov D.V. Pathology of the sinuses and veins of the dura mater // Health of Ukraine. K., 2004, No. 9, p. 3.
- Manvelov L. S., Kadykov A. V. Venous insufficiency of cerebral circulation // Atmosphere. Nervous diseases. 2007, no. 2, p. 18–21.
- Putilina M.V., Ermoshkina N.Yu. Venous encephalopathy // Journal of Neurology and Psychiatry named after. S. S. Korsakova. 2013, v. 113, no. 4, p. 26–34.
- Chukanova E. I., Chukanova A. S., Daniyalova N. D. Cerebral venous disorders: diagnosis, clinical features // Neurology. Neuropsychiatry. Neurosomatics. 2014, no. 1, p. 26–34.
- Berdichevsky M. Ya. Venous discirculatory pathology of the brain. M.: Medicine. 1989. 224 p.
- Caso V., Agnelli G., Paciaroni M. Frontiers of Neurology and Neuroscience. Handbook on Cerebral Venous Thrombosis. 2008. V. 23.
- Kholodenko M.I. Disorders of venous circulation in the brain. M.: Publishing house of medical literature, 1963. 226 p.
- Neimark E. Z. Thrombosis of intracranial sinuses and veins. M.: Medicine, 1975.
- Shemagonov A.V. Chronic cerebral venous discirculation syndrome. www.medicusamicus.com.
- Skorobogatykh K.V. State of the intracranial venous system in patients with chronic tension-type headache. Author's abstract. ...cand. honey. Sci. M., 2009. 27 p.
- Putilina M.V. Asthenic disorders in general medical practice // Nervous diseases. 2014, no. 4, p. 26–34.
- Savelyeva L. A., Tulupov A. A. Features of venous outflow from the brain, according to magnetic resonance angiography // Bulletin of the Novosibirsk State University. Series: Biology, clinical medicine. 2009, vol. 7, issue. 1, p. 36–40.
- Skorobogatykh K.V. State of the intracranial venous system in patients with chronic tension-type headache. Author's abstract. ...cand. honey. Sci. M., 2009. 27 p.
- Putilina M.V. The role of arterial hypertension in the development of chronic cerebrovascular accident // Journal. neurology and psychiatry named after. S. S. Korsakova. 2014, no. 9, p. 119–123.
- Nordvik B. Mechanism of action and clinical use of the drug Actovegin. Actovegin. New aspects of clinical application. M., 2002. pp. 18–24.
- Fedorovich A. A., Rogoza A. N., Kanishcheva E. M., Boytsov S. A. The effect of the drug Actovegin on the metabolic and vasomotor functions of the microvascular endothelium in human skin // Rational pharmacotherapy in cardiology. 2010, No. 1, vol. 6, p. 119–123.
- Fedorovich A. A. Non-invasive assessment of vasomotor and metabolic function of microvascular endothelium in human skin // Regional blood circulation and microcirculation. 2013, No. 2 (46), p. 15–25.
- Hayward CS et al. Assessment of endothelial function using peripheral waveform analysis // J. Am. Coll. Cardiol. 2002, No. 40, p. 521–528.
- Fedorovich A. A. Disturbances of microcirculation processes in the skin in diseases of the peripheral vascular bed // Farmateka. 2013, No. 12.
- DeBacker WA et al. // Am J Respir Crit Care Med. 1995; 151(1).
M. V. Putilina, Doctor of Medical Sciences, Professor
GBOU VPO RNIMU im. N. I. Pirogova Ministry of Health of the Russian Federation, Moscow
Contact Information
Cerebral vasospasm
Elderly people, middle-aged and brain-aged people are often bothered by headaches, noise and dizziness, increased fatigue, memory impairment, and decreased performance. Often patients do not take such complaints very seriously. Meanwhile, these may be signs of vasospasm in the left cerebral arteries, MCA (middle cerebral artery) and ACA (anterior cerebral artery). Cerebral vasospasm (narrowing of the lumen of the arteries at the base of the brain after subarachnoid hemorrhage due to rupture of a saccular aneurysm) can secondary cause cerebral ischemia.
After an aneurysm ruptures, the patient experiences a temporary period of improvement or stabilization until symptomatic vasospasm occurs. Neurological symptoms of cerebral spasm from the fourth to the fourteenth day after the first rupture of the aneurysm. The resulting neurological symptoms correspond to cerebral ischemia in specific arterial territories. The severity of cerebral vasospasm determines the likelihood of developing cerebral ischemia and infarction.
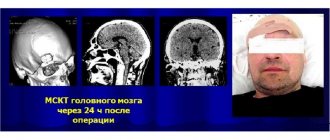
Signs of vasospasm in the left arteries of the brain, MCA and ACA often occur in those patients in whom early magnetic resonance or computed tomography of the brain showed layers of coagulated blood 1 mm thick or more in the sulci of the brain or spherical blood clots larger than 5 mm3 in the basal cisterns.
Doctors at the Yusupov Hospital determine the localization and severity of vasospasm in the ACA and MCA using magnetic resonance or computed tomography. To ensure an accurate prognosis, a CT scan of the brain is performed between 24 and 96 hours after subarachnoid hemorrhage.
Clinically pronounced cerebral vasospasm is manifested by symptoms that relate to one or another pool of blood supply to the brain of a certain artery. When the trunk or main branches of the middle cerebral artery (MCA) are involved, the patient develops the following symptoms:
- Contralateral hemiparesis - weakness of the muscles of half the body on the side opposite to the intracerebral hemorrhage;
- Dysphasia is a speech disorder due to spasm of the arteries of the dominant hemisphere of the brain;
- Anosognosia, apraktoagnosia - a recognition disorder due to spasm of the arteries of the non-dominant hemisphere of the brain.
Signs of vasospasm in the left cerebral arteries, MCA and ACA may not be pronounced due to the fact that collateral blood flow is formed in the brain through fusion of areas of adjacent cerebral blood supply.
Ischemia due to vasospasm of the ACA is manifested by abulia. The patient is awake, lies with his eyes closed or open, and responds to instructions with a delay. He cannot actively conduct a conversation, but answers questions with short phrases that he pronounces in a whisper, chews food for a long time and often holds it between his gums and cheek. All focal neurological symptoms resulting from cerebral vasospasm in patients may occur suddenly, reaching maximum severity within a few minutes, or develop over several days.
If the entire brain area in the MCA basin (middle cerebral artery) is subject to ischemia or infarction, its edema develops, which can lead to increased intracranial pressure. Early magnetic resonance or computed tomography of the brain can predict an unfavorable outcome if a large blood clot is detected in the Sylvian cistern or in the lumen of the Sylvian fissure and a second significant clot in the basal frontal fissure, located between the cerebral hemispheres. The simultaneous presence of clotted blood in these areas is combined with severe symptomatic spasm of the MCA and ACA. In such a situation, superficial collaterals in the cerebral cortex from the ACA are not able to compensate for ischemia in the MCA territory.
If spasm of the cerebral arteries occurs against the background of subarachnoid hemorrhage, drug prevention and treatment are ineffective.
Because patients with cerebral vasospasm have increased blood volume and swelling of the brain parenchyma, even the small increase in intracranial volume that occurs with vasodilator exposure can aggravate neurological disorders. If a patient has severe symptomatic cerebral vasospasm, neurologists do not prescribe vasodilators.
All efforts of doctors are aimed at increasing cerebral perfusion pressure by increasing mean arterial pressure. This is achieved by increasing plasma volume and prescribing vasopressor drugs (phenylephrine, dopamine). Since treatment aimed at increasing perfusion pressure leads to an improvement in the picture of the neurological status in some patients, but high blood pressure is associated with the risk of recurrent hemorrhage, when using this method of treatment, neurologists at the Yusupov Hospital determine cerebral perfusion pressure and cardiac output, and conduct a direct study of the central venous pressure. In severe cases, the patient's intracranial pressure and pulmonary artery wedge pressure are measured.
Administration of the osmotic diuretic mannitol, while maintaining adequate intravascular volume and mean arterial pressure, increases the patient's serum osmolarity. In severe cases, barbiturate coma is used to reduce intracranial pressure.
Hypoplasia of the ACA
The cause of sudden blockage of a cerebral vessel is often an abnormal decrease in its lumen. The reason for this is not cholesterol plaques, but hypoplasia of the cerebral artery - a pathological narrowing of the vessel. The disease is observed in 80% of older people. In addition to their congenital defect, age-related changes in blood vessels are added.
PMA hypoplasia – what is it and how does it manifest? ACA hypoplasia manifests itself in insufficient development of the right cerebral artery. The vessel has an abnormal shape. With this pathology, the structure of the blood vessels supplying intracranial structures may be disrupted. ACA hypoplasia is a congenital pathology that occurs in utero. With hypoplasia of the ACA, the nutrition of the cerebellum, brainstem and occipital lobes is disrupted. As a result of the pathology, the risk of aneurysm formation or stroke increases. Hypoplasia of the ACA is a dangerous condition, to which neurologists at the Yusupov Hospital and neurosurgeons at partner clinics pay special attention.