How does the disease develop and what are the consequences?
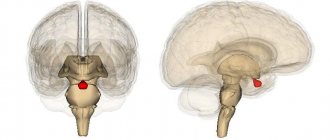
The activity of the endocrine glands, which produce cerebrospinal fluid, is disrupted. As a result, there is too much cerebrospinal fluid, and the small body is unable to ensure its normal outflow. On the left of the diagram is a normal brain, and on the right is one affected by hydrocephalus.
Hydrocephalic babies are easily recognized by their disproportionately large heads. Water cannot compress and increases the volume of the skull, and since in children under one year old rigid connections between the cranial bones have not yet formed, the increase in volume of the head occurs unhindered.
When hydrocephalus of the brain develops in an older child, excess fluid manifests itself exclusively as damage to the central nervous system.
The disease is quite dangerous: the cerebrospinal fluid does not leave the head and begins to put pressure on the nervous tissue, destroying neural connections. Without proper treatment, this usually leads to swelling of the brain and ultimately the death of the child.
Classification of the disease
In children, there are four main types of hydrocephalus of the brain:
- External - fluid accumulates in the subarachnoid space - the cavity between the pia mater and the arachnoid mater.
- Internal - cerebrospinal fluid remains in the cerebral ventricles. The substance of the brain begins to thin out.
- Open (communicating) - all ventricular systems of the brain expand, but there are no obstacles to the movement of fluid through the cerebrospinal fluid system.
- Closed (occlusive) - disruption of the liquor flow is caused by pathologies of the ventricles: their adhesions, neoplasms.
The open form of childhood hydrocephalus can be either external or internal. But occlusal in 99% of cases is internal.
In addition, dropsy is also divided according to the form of its flow:
- Acute – a rapid increase in intracranial pressure, the baby’s condition worsens in the period from one to three days.
- Subacute - normal circulation of cerebrospinal fluid is disrupted for three to six months, after which severe brain damage occurs.
- Chronic – the development of the disease also lasts up to six months, but there is no such serious damage to the brain. Characteristic of open hydrocephalus.
Causes of pathology
As a rule, this is a congenital disease. There are also acquired forms, but they are quite rare.
The causes of cerebral hydrocephalus in children are intrauterine infections, birth injuries, genetic disorders, and central nervous system defects.
Depending on the stage at which the disease developed, its causes vary:
- Fetal hydrocephalus in the vast majority of cases develops due to defects of the central nervous system. Infectious infections are to blame for the pathology of every fifth intrauterine hydrocephalus. Only a small proportion is due to genetic disorders.
- When the disease begins to develop immediately after birth, it is most likely due to infections in the womb. Such situations account for 75%. In 15% of cases, a newly born baby begins to suffer from dropsy due to a birth injury that led to meningitis or intracranial hemorrhage. The remaining 10% are malformations of either the spinal cord or brain, as well as disturbances in the functioning of blood vessels.
- In children aged one year and older, hydrocephalus is almost equally formed as a result of one of the following reasons: hemorrhage; brain tumor (spinal or brain); consequences of TBI; consequences of brain inflammation; genetic problems; malformations of cerebral vessels.
These generalized reasons also have their own classification.
So, among the infections that cause the disease, the following are common:
- rubella;
- cytomegalovirus;
- neurosyphilis;
- herpes virus type 1 or 2;
- toxoplasmosis;
- bacteria and viruses that cause meningitis;
- parotitis.
Defects responsible for the formation of dropsy:
- Narrowing of the canals connecting the cerebral ventricles.
- Arnold-Chiari syndrome (underdevelopment of the posterior fossa of the skull, due to which the brain structures located there do not fit into it).
- Anomalies of the cerebral venous system.
- Underdevelopment of the openings through which cerebrospinal fluid drains into the subarachnoid space.
- Dandy-Walker syndrome (anomaly of the development of the cerebellar spaces and cerebellum).
Also, among oncological diseases, hydrocephalus can be caused by:
- brain cancer;
- papilloma;
- tumor of the skull bones;
- brain ventricle tumor;
- vascular plexus meningioma;
- various forms of spinal cord oncology that impair fluid circulation.
Diagnosis of internal hydrocephalus
The clinical symptoms of internal hydrocephalus are usually so characteristic that they allow the neurologist at the Yusupov Hospital to suspect its presence during the first examination of the patient. To determine the type and degree of hydrocephalus, as well as to identify the pathological process that caused the disease, doctors conduct a comprehensive examination of the patient, which includes radiography of the skull, ultrasound, computed tomography or magnetic resonance imaging.
X-ray signs of hydrocephalus are thinning of the skull bones and divergence of the sutures between them; a symptom of “finger impressions” is observed on the inner surface of the cranial vault. With hydrocephalus caused by stenosis of the cerebral aqueduct, a decrease in the volume of the posterior cranial fossa is determined on radiographs of the skull. An increase in the volume of the posterior cranial fossa on craniograms is a sign of hydrocephalus in Dandy-Walker syndrome. If one of the interventricular communications is closed, the asymmetry of the skull is visible on the craniogram.
Echoencephalography (ultrasound) allows you to determine the degree of increase in intracranial pressure. In children of the first year of life, an ultrasound scan of the brain is performed through an open fontanel using ultrasonography. The most informative are tomographic diagnostic methods. They make it possible to determine the nature of hydrocephalus, identify the location of blockage of the cerebrospinal fluid tract or an existing congenital anomaly, and diagnose a neoplasm, cyst or hematoma. Monoventricular internal hydrocephalus is characterized by an increase in the volume of one ventricle of the brain.
If vascular disorders are suspected, magnetic resonance angiography is performed. For congenital hydrocephalus of infectious origin, PCR diagnostics are performed to determine the type of pathogen that caused it. Visual disturbances and the condition of the optic discs are assessed by an ophthalmologist at the Yusupov Hospital. Neurosurgeons at partner clinics decide on the need or advisability of surgical intervention.
Risk factors
There are accompanying conditions that contribute to the development of hydrocephalus of the brain in a child:
- Early birth (gestation period did not exceed 34 weeks).
- A narrow maternal pelvis and, as a result, a difficult birth process.
- The newborn's light weight is less than one and a half kilograms.
- During childbirth, hypoxia or asphyxia was observed in the fetus.
- Active methods of obstetrics: manual techniques, vacuum, forceps.
- The mother suffered viral infections during pregnancy: herpes, influenza, ARVI, toxoplasmosis.
- Bad habits of the mother that manifested themselves during pregnancy.
- Untreated sexually transmitted diseases in the mother during pregnancy.
Most risk factors for hydrops are related to maternal health.
Even indirect reasons, such as a premature baby with low weight, indicate an abnormal pregnancy. Every problem with a woman’s health during pregnancy weakens the embryo’s body.
How does hydrocephalus manifest?
Depending on the form of development of the pathology and the age of the child, the external signs of the disease change.
For children under two years of age, in which in 95% of cases hydrocephalus is a congenital pathology, the following symptoms are characteristic:
- Severe course of the disease. A rapidly deteriorating condition caused by damage to brain structures.
- The main symptom is a rapid increase in head volume. Growth of 1.5 cm or more every month is typical, for at least three months in a row. Starting from the ninth month of life, growth drops to 8-9 mm.
- A child is born with a head whose girth is larger than the girth of the chest. If by six months the ratio does not change, and the head is still larger than the chest, there is reason to suspect hydrocephalus.
- The veins on the occipital, temporal and frontal parts of the head are clearly visible.
- At three months the child does not yet hold his head up and begins to sit up late, crawl, and walk.
- The fontanel on the top of the head is convex.
- The accumulation of cerebrospinal fluid primarily occurs in the frontal lobes of the brain. Head enlargement starts from the forehead.
- While fixating the baby's gaze, the baby's pupil twitches chaotically.
- The scalp becomes thin and has a painful shine.
- Overhang of the brow ridges over the facial bone - the eyes appear to be very deep-set.
A number of less characteristic signs can confuse the initial diagnosis of hydrocephalus in children and complicate treatment. For example, tearfulness, poor appetite, slow weight gain, frequent regurgitation, drowsiness, legs constantly bent at the knees, head tilting - all these symptoms are characteristic of hydrocephalus. But at the same time, they can be observed in dozens of other childhood diagnoses.
In the acute form of dropsy, when the disease progresses rapidly, other signs can be observed:
- convulsions;
- long cry on one note;
- loss of acquired physical skills (sitting, following other people's movements, vocal functions);
- vomit.
For children aged two years and older, other manifestations of hydrocephalus of the brain are typical:
- Headaches that begin in the morning (after sleep) and gradually subside in the evening. Nausea and vomiting often begin at the same time.
- Migraines that appear after stress, mental or physical work. Often accompanied by nosebleeds.
- A feeling of a rush to the head when bending over and bursting headaches.
- Pain in the fundus of the eye.
- Visual impairment: loss of sharpness, double vision.
- Urinary incontinence.
- Decreased muscle strength, accompanied by rapid fatigue.
- Cramps and fainting.
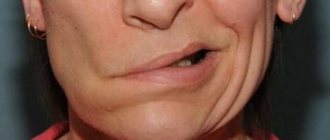
- Loss of coordination and uncontrolled movements of the limbs.
Symptoms of internal non-occlusive hydrocephalus
The main symptom of hydrocephalus in children is an increase in the size of the head. In young children, the bones of the skull are thinned, soft, and the sutures between them diverge. A convex fontanelle stands out, which does not close for a long time. The skin on the skull is thin, shiny, and venous vessels are visible under it. Babies are lagging behind in physical and mental development, they are capricious, and cry constantly. The eyes are deep-set, looking down. Visual acuity decreases. With high intracranial pressure, nausea, vomiting occurs, and convulsions develop.
In older children, the signs of the disease worsen: irritability with attacks of aggression, lethargy, headaches, impaired memory, attention and consciousness. Coordination of movements and intelligence are impaired, learning problems appear, and mental retardation develops.
The characteristic signs of internal hydrocephalus in adults are:
- shaky, unsteady gait;
- loss of urinary control;
- memory impairment;
- headaches that are not always relieved by painkillers;
- blurred vision;
- vision deteriorates, pressure is felt on the eyes;
- nausea and vomiting.
Patients experience scattered attention and decreased concentration, and loss of thinking skills. Signs of mental disorders appear:
- emotional instability;
- attacks of aggression;
- neurasthenia;
- replacement of apathy with emotional upsurge.
Impaired motor functions appear. Impaired walking, contracture in the joints or paresis of the lower extremities develops. Patients often do not attach importance to these symptoms, mistaking them for signs of normal aging and do not consult a doctor.
Treatment of hydrocephalus in children
Due to the complexity of the disease and its danger, treatment for a child with hydrocephalus is prescribed not only by a neurosurgeon, but also by a neurologist.
Treatment can be conservative (that is, without surgery, only with the help of medications) or surgical.
During drug treatment, the first step is to reduce intracranial pressure using the drug Diacarb. It reduces the production of cerebrospinal fluid and promotes the removal of potassium from the body.
In the hospital, strong osmotic diuretics are prescribed - oral Glycerin and Mannitol. Salt diuretics, for example Furosemide, are also prescribed. It, like Diacarb, should be taken in conjunction with drugs that maintain normal potassium levels - Panangin or Asparkam.
Doctor's advice
Hydrocephalus - this conclusion can often be found after an ultrasound scan of infants. However, in most cases it is compensatory in nature, everything returns to normal by the first year of life. In addition to birth injuries, protracted labor, structural features, the cause of such dropsy is the immaturity of the nervous system. True hydrocephalus is characterized by the entire clinical picture of increased intracranial pressure - an increase in the size of the head, monotonous crying, and the presence of neurological symptoms. Conclusion Ultrasound is not a diagnosis, it is the result of an examination; the diagnosis is made based on a combination of complaints, anamnesis, examination, and research data.
Victoria Druzhikina Neurologist, Therapist
Any medicinal forms of treatment for acute hydrocephalus must be carried out under the strict supervision of doctors, and intermediate results must be checked using computed tomography and neurosonography.
Along with diuretic enzyme blockers, medications are prescribed that stimulate the functioning of brain neurons. For example, "Encephabol".
As for surgical intervention, the most effective method of surgical treatment of the brain in children is bypass surgery. Often this is the only way to save a child's life.
Shunting is the creation of a flow path (shunt) for cerebrospinal fluid to bypass an existing blockage. For closed hydrocephalus, it is used when tumors have already grown into the brain.
In the open form of the disease, three types of bypass surgery are provided:
- Ventriculoatrial.
- Ventriculo-peritoneal.
- Lumbo-peritoneal.
In addition to shunting, another type of surgical intervention is possible for closed forms of hydrops - dissection of arachnoid adhesions. This method involves the absorption of cerebrospinal fluid.
Watch the video about the causes and treatment of hydrocephalus:
The life span and quality of life of a child with hydrocephalus, his chances of recovery depend on many factors: the reasons that caused the development of the disease, the speed of diagnosis, the quality of treatment. But even a healthy baby can become a victim of the disease.
Don't forget about prevention. Protect your child from head injuries in every possible way; be sure to use protective equipment during active recreation. If the baby was born premature, be sure to undergo routine examinations with a neurologist, do an ultrasound and an MRI.
Women who are about to become mothers or planning to conceive a child should be aware of their health. Get rid of bad habits a few months before pregnancy. Get screened for infections. If you happen to get sick while pregnant, consult a geneticist and undergo an additional ultrasound.
Your unborn baby is sensitive to literally everything, so take care of him even before birth.
This article has been verified by a current qualified physician, Victoria Druzhikina, and can be considered a reliable source of information for site users.
Bibliography
1. https://docs.cntd.ru/document/499002598
Rate how useful this article was
3.5 4 people voted, average rating 3.5
Did you like the article? Save it to your wall so you don’t lose it!
Is it possible to cure the disease and treatment?
There are medications that can reduce the volume of accumulated transudate and reduce intracranial pressure.
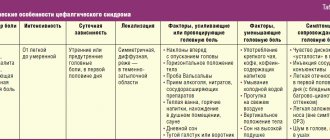
Drug therapy is prescribed for compensated types of pathology. Effective medications for improving the condition of a baby with hydrocephalus are presented in the table.
| Name of the drug | Description | Mode of application |
| Diakarb | The product has diuretic properties, removes excess fluid from the body, and releases potassium. | Used to treat children from 4 months of age at a dose of 50 mg twice a day. |
| Furosemide | Powerful diuretic. Thanks to this property, it is possible to reduce intracranial pressure and normalize the general condition of the patient. | Prescribed from 1 to 3 mg. The dosage is calculated individually based on the body weight of the newborn. In the form of injections from 1 to 1.5 mg per kilogram of body. |
| Mannitol | Diuretic drug. The action of which is to increase the osmotic pressure in the renal tubules. | The product is available in powder form. Before use, it is dissolved in sterile water and administered intravenously |
The information provided in the table is for informational purposes only, so you should consult your doctor before using medications.
Surgical methods of treatment in children
Today it is practiced to use intrauterine treatment of hydrocephalus.
Thanks to a puncture of the anterior abdominal wall of the expectant mother's abdomen, doctors remove fluid from the peri-cerebral space. The procedure is done once. Another effective way to pump fluid out of a baby’s head before birth is bypass surgery. The entire system will remain inside the baby's head until the moment of birth.
Neuroendoscopic operations
A new effective, but at the same time expensive method of surgical treatment of internal hydrocephalus of the fetus. The duration of the operation is no more than 20 minutes.
A special medical device, a neuroendoscope with a built-in small camera, shows the place where the catheter is inserted. It is necessary to quickly remove accumulated cerebrospinal fluid. The doctor makes an additional hole to effectively remove transudate from the enlarged areas of the ventricles of the brain.
Bypass operations
The most effective way to treat true hydrops, but it is carried out only after birth. During the operation, shunts - silicone tubes - are inserted.
They drain excess fluid from the ventricles of the brain into the abdominal region. A special valve regulates the flow volume. The ICP stabilizes and the cerebrospinal fluid does not flow back into the brain cavity.
Several similar procedures are performed throughout the child's life. The tubes can become clogged and break, which leads to mechanical damage and disruption of their operation. Planned surgical interventions are prescribed due to age-related changes in the baby’s body.