Each person, to the best of his ability (and, let's be honest, desire) takes care of his health: a balanced diet, giving up bad habits, playing sports, walking in the fresh air, and getting proper rest. Many people visit a doctor at least once a year, even without any complaints or deterioration in health - this is a routine check-up, clinical tests, completely safe studies (ultrasound, fluorography, ECG, etc.). But sometimes concern about the state of one’s health takes on a clearly exaggerated, pathological character. A person constantly looks for (and finds!) symptoms of various diseases (as a rule, we are talking about severe, incurable pathologies), and turns to doctors in search of confirmation of a self-made diagnosis. Gradually, this anxiety takes on an obsessive nature - hypochondriacal depression , which requires, first of all, the help of a psychotherapist. This disorder is quite common, but only a few decide to turn to a specialist; most patients try to cope with this problem on their own. Doctors at the Leto mental health center will help overcome constant fear and anxiety and return the patient to a full life, full of pleasant events.
Etiology
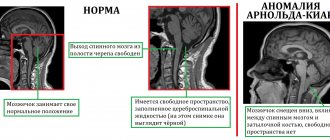
To date, a hereditary predisposition to the development of depressive disorders . It is assumed that genetically determined disorders in the production of neurotransmitters, a decrease in the sensitivity of cells to their influence, lead to characteristic symptoms. Similar changes can occur as a result of organic brain damage as a result of:
- stroke;
- intoxication;
- chronic hypoxia due to alcohol and drug use;
- cerebrovascular pathologies.
However, the “impetus” for the progression of manifestations of hypochondriacal depression is usually external circumstances:
- past illness;
- diagnosed severe pathology in a relative or close friend;
- news in the media (for example, articles describing a serious disease, reports about the spread of viral and bacterial infections, etc.).
people who are self-centered and are more susceptible to depression of a hypochondriacal nature . In addition, such a disease also occurs in cases where a person cannot accept himself and his body, suffers from low self-esteem, a feeling of his own low value and worthlessness, feels guilty about something and wants to subconsciously suffer a well-deserved (as he believes) punishment . An indifferent attitude on the part of relatives plays an important role, and constant complaints about health are nothing more than an attempt to attract attention to oneself.
general information
Hypochondriacal neurosis is a person’s inadequate attitude towards his body and is a psychological disorder.
The disease can develop against the background of any somatic pathologies and emerging negative thoughts. This is the type of neurosis when a person begins to especially attribute non-existent diseases to himself and is anxious about his well-being. The group includes teenage children and the elderly. Women suffer from this disease much more often than men, so you need to urgently contact a specialist to get the necessary help.
Clinical picture
The main symptom of hypochondriacal depression is worries about one’s own health. The patient constantly listens to internal sensations; the slightest discomfort, and even more so, pain, causes a deterioration in mood, even leading to a panic attack. A person temporarily completely loses interest in work/study/everyday activities and “switches” to searching for information about what this or that symptom means.
In this case, minor diseases are immediately “swept aside”. The patient does not think that, for example, discomfort in the abdomen can only be a consequence of overeating, poor diet, or digestive disorders. Immediately thoughts come to mind about oncology, perforated ulcers , and other similar serious diseases. Complaints of pain in the heart area are also typical.
A person consults a doctor if there is any slight deterioration in health. A monotonous, emotionally unexpressed presentation of complaints is typical, but the patient only expects confirmation from the doctor of the alleged diagnosis. If this does not happen, he easily becomes emotional, tries to prove that he is right, and demands various, often technically complex, expensive and unnecessary, from the point of view of a specialist, examinations.
But even negative results of a comprehensive comprehensive diagnosis either do not bring relief or provide only a short-term effect. After a certain time everything starts again.
In addition to complaints about well-being, hypochondriacal depression is characterized by:
- apathy;
- sad, depressed state;
- monosyllabic quiet speech;
- disinterest in the results of their work;
- neglect of household duties;
- indifference to appearance, sloppiness;
- decrease in social activity, desire for solitude, and attempts to “stir up” a person, “pull” him out for a walk, etc. can cause an outburst of anger and irritation.
With hypochondriacal depression, attempts at self-medication are extremely dangerous. For example, fearing a heart attack, a patient may start taking antithrombotic, antiarrhythmic or antihypertensive drugs, fearing a bacterial infection - antibiotics. Uncontrolled use of any drugs, and especially potent drugs, is fraught with severe complications and side effects.
In addition, we should not forget about developing concomitant diseases. Due to growing tension and anxiety, sleep deteriorates, and a constant feeling of weakness and weakness appears. Against the background of permanent stress, various cardiovascular disorders develop and periodic headaches occur. Doctors often encounter hyperthermia of a neurological nature. If you do not consult a specialist in a timely manner, exaggerated somatic symptoms can develop into real diseases.
Hypochondriacal syndromes
Hypochondria, as mentioned, is manifested by pathologically exaggerated fears for health, searches for or confidence in the presence of any disease in the absence of objective signs of the latter. The structure of hypochondriacal syndrome includes a variety of disorders.
Hypochondriacal fixation of attention. Focusing on pathological sensations, dysfunctions of the body, and possible causes of their occurrence. “Somatization of the psyche” is observed in the form of dominance of various painful sensations in the self-perception of patients. Patients strive to take into account and identify any, including the most minor, deviations from what, in their opinion, corresponds to a normal state of health. Absolutization of ideas about health is characteristic - the latter is considered as a kind of ideal state, the utmost perfection of the functions and structure of the body, excluding any anomalies.
| | We will help you cope with hypochondria! |
This maximalism clearly indicates the juvenileism (resemblance to the personality of adolescence) of the psyche of hypochondriacal patients. With neurotic hypochondria, the focus on the bodily self is involuntary, obsessive. Patients try to distract themselves with something else, to think less about their well-being, although they are not entirely successful: “Thoughts only about the disease. I’m chasing them away, trying to think about something else... The world has narrowed, there’s only one disease on my mind...”
With the worsening of hypochondria, the absorption of attention in the somatic sphere becomes, as it were, intentional, appropriated and reflects the motives of the individual who have become conscious, descending to a different, lower level of motivation. Hypochondriacal narrowing of the sphere of consciousness and the associated limitation of external contacts, their transfer to another plane is sometimes called hypochondriacal autism. The psychic self may also become the object of patient attention. This is defined as a pathological reflection and is usually observed with depersonalization, fear of madness, especially in adolescence and young adulthood.
Affective disorders. Anxiety, fears, panic reactions associated with general health disorders, individual manifestations or ideas about the nature of the alleged disease. Hypochondriacal emotions, according to patients, are of a local nature, but, most importantly, they are entirely determined by the state of health and its assessment as if other things no longer exist.
“I’m in a bad mood because it hurts. If it doesn’t hurt, your mood is normal.” This somatization of emotions apparently reflects the predominance of the hypochondriacal attitude and determines the content of the cognitive component of affective reactions. Acute hypochondriacal crises with fear of death, confusion, and agitation may occur. The mentioned affective disorders most often occur against the background of an anxious mood.
If melancholic depression also occurs, then fears for one’s health are joined by concerns for others, especially close people; fear of infecting them, self-blame for the unrest they cause; Sometimes patients are alarmed to discover signs of their illness, despite the precautions taken. The presence in the structure of a depressed mood of suspicion and paranoid alertness can be expressed by fears of retaliatory revenge from others for damage to their health allegedly caused by the patients.
Hypochondriacal detailing of thinking. The complaints of a significant part of the patients are carefully developed, all the circumstances of the disease are reported with an extreme abundance of detail. Often complaints are systematized in accordance with the existing concept of the disease and are filled with medical terminology. Patients identify the main and secondary symptoms, group them, establish cause-and-effect relationships between them, and sometimes combine them into very intricate structures.
There is a tendency towards fruitless reasoning to understand and explain to the doctor the reasons for the appearance of the disease or individual symptoms, which for some reason are given the greatest importance - hypochondriacal reasoning. Sometimes such a feature is revealed: the more pronounced the affective radical of hypochondria (fears, anxiety), the less represented is the tendency to intellectualize, and vice versa.
The structuring of hypochondriacal constructs may be preceded by a search for a suitable model for explaining one’s well-being. Reading, say, medical literature, the patient finds manifestations of one or another disease, in fear discovering similarities with the most serious of them. He does the same, listening with bated breath to stories about other people’s illnesses. This period of hypochondriacal identification is often accompanied by confusion. The identification of one’s condition with information about one’s supposed illness is sometimes so complete that the patient clearly experiences the same painful sensations: “the illnesses are passing on to me.” This can be seen as the action of the mechanisms of appropriation that underlie some forms of pathology of self-consciousness - hypochondriacal depersonalization. On the other hand, the patient can find signs of his disease in other people, that is, project his ideas about it outward - hypochondriacal transitivism.
A shift in interests is taking place towards an active, albeit selective, study of medical information. The imaginary confidence in one's own medical knowledge gradually grows. Sometimes an undisguised distrust of doctors and conventional methods of treatment appears; patients strive to see the most authoritative specialists, in their opinion, and seek the latest methods of examination and treatment.
The tendency to consider one’s illness as something unusual or even exceptional with full confidence that others should share this opinion, we would call hypochondriacal egocentrism. Another manifestation of it is to consider everything that happens around through the prism of hypochondriacal ideas. For example, the patient is told about completely unrelated things, but he reduces this to the topic of illness.
Having learned that his son is skipping classes, the patient concludes: “He doesn’t think about his father, he doesn’t care that I’m sick.” My wife stayed late after work, and here’s the reaction: “She apparently doesn’t care whether I’m alive or not.” Someone had a resounding success, but the patient thinks: “With my health, I could not stand this.” This envy and discontent sometimes turns against doctors, especially those who do not follow the lead of their patients. The aggression of the latter then spills out in complaints and litigious harassment, to which a lot of time and energy are devoted, which even a healthy person could envy.
Some patients save all the documentation received from the medical institutions where they were, requests, copies of complaints and responses to them, clippings from newspapers, magazines, and create their own “archive” of the disease. Hypochondriacal patients often become regular subscribers to specialized literature, faithful readers of the Health magazine, and collectors of apocryphal publications on the treatment of various diseases, so that some acquire decent home medical libraries. Considerable sums are sometimes spent on consultations, treatment by celebrities and fashionable healers, and the purchase of literature from the more than modest family budget of many patients.
Activity and behavior disorders. Reflect the one-sided orientation of activities in terms of maintaining and restoring health. Behavior can be different, which reflects the depth and severity of hypochondriacal disorders: from frequent requests for medical help, including emergency, to the development of their own self-medication systems or the use of healer recommendations and paramedicine methods.
The lifestyle undergoes radical changes: contacts, social activity are limited, nutrition, daily routine, sleep, etc. are carefully regulated. Patients can also do this in order to prevent possible disorders - health hypochondria. This, in particular, was I. Kant - the “great hypochondriac.” If they manage to “cure” using their own methods, they strive to replicate these methods and stubbornly seek public recognition - an expansive hypochondria of health, which is actually a delusional, hypochondriacal paranoia of health.
Productive psychopathological phenomena. They include various disorders of co-anesthesia (senesthesia, senestopathy, other disorders of elementary sensitivity), obsessive-phobic phenomena, reactive and autochthonous affective shifts, overvalued ideas, overvalued delusions, delusional ideas of hypochondriacal content, poisoning, obsession, influence, paraphrenic delusions. Taking into account the nature of productive disorders, the following clinical variants of hypochondriacal syndrome are distinguished.
Neurotic (phobic, obsessive) hypochondriacal syndrome. Observed in neuroses. Determines the clinical picture of hypochondriacal neurosis. It is characterized by constantly disturbing thoughts, doubts, fears, fears of a serious illness, and sometimes a mental disorder. Obsessive-phobic phenomena are of psychogenic origin (with onset similar to a reaction to an illness) and are amenable to psychotherapeutic correction.
Many patients understand that their fears are unfounded and painful. Similar disorders can occur in the structure of neurosis-like states of various origins. Such hypochondria is an illustration of a split personality. One Self identifies itself with a sick person who finds various health abnormalities in himself and is afraid of this; the other Self identifies itself with a healthy person who is alarmed that something wrong is happening to his psyche. Depressive hypochondriacal syndrome. Identified in the depressive phases of circular psychosis.
Against the background of a depressed mood, persistent, difficult or completely uncorrectable, frightening ideas arise about the presence of some incurable disease, related in content to malaise, depression of vital tone, or painful algia in various parts of the body. This is more typical for states of anxious depression in individuals of an egocentric nature. A critical attitude towards the disease is often lost or superficial. Suicidal thoughts and actions are possible.
Senestopathic-hypochondriacal syndrome. Obsessive, overvalued and delusional formations of hypochondriacal content, associated with varied and numerous senestopathic sensations. Most often observed in the extended pre-delirium period of a sluggish endogenous disease. It can occur in organic diseases of the central nervous system of various origins, consequences of traumatic brain injury, vascular diseases of the brain, and symptomatic psychoses.
Delusional hypochondriacal syndrome. A distinction is made between paranoid, paranoid and paraphrenic variants of delusional hypochondriacal syndrome. Paranoid hypochondriacal syndrome is a systematized interpretive delusion of a serious illness, often existing for many years. Long-term persistence of overvalued hypochondriacal ideas, often combined with litigious and paranoid tendencies, is observed within the framework of hypochondriacal personality development.
Patients spend many years in the heroic role of a sick person, “squeezing” out of this various possible advantages, and they do this skillfully, even skillfully, without experiencing moral torment. The ethical formula of such hypochondriacs is simple: “I’m sick, and I can do anything.” Paranoid hypochondriacal syndrome is formed in the structure of the syndrome of mental automatism and is combined with delusional ideas of physical influence, phenomena of mental automatism, primarily senestopathic.
Paraphrenic hypochondriacal syndrome is a hypochondriacal delusion of fantastic content: patients “have their bones changed, their brains are sucked out, their internal organs are burned,” they are “acted on from space, from other planets.” A nihilistic hypochondriacal syndrome is also distinguished - patients are convinced that their insides have rotted and their vital physiological functions have been disrupted. Within the framework of neurotic hypochondria, hypochondriacal reactions observed in somatic patients should be considered.
They can occur with a predominance of fear and anxiety, obsessive phenomena or overvalued formations. Hypochondriacal reactions occur preferentially in individuals of an asthenic, anxious-suspicious and hypothymic type. The presence of affective viscosity, rigidity, and intellectual deficiency may cause delayed reactions. It is impossible not to note the important role in the genesis of hypochondriacal reactions played by violation of the rules of “mental asepsis” on the part of the doctor (iatrogeny), nursing staff (sorrorrhagenia) - careless statements, inattention, and sometimes rude straightforwardness. Communication between patients (egrotogeny) greatly contributes to the appearance of hypochondriacal reactions.
A particular danger in terms of the development of psychogenic hypochondria is the activity of all kinds of healers from “traditional” and occult medicine. Many healers work according to this scheme: first they show the patient that he has so many different diseases that it is surprising how he lived to see this day, and then they heal him in a few minutes. Convincing a person that he is sick is much easier than eliminating the consequences of mental shock or assuring him that there is no longer any danger. We should also not forget that the cultivated belief in healing is far from a safe form of manipulation of consciousness; it inevitably leads to personality regression and encouragement of the patient’s dependent role in the healing process, which is completely unacceptable from the doctor’s position.
Back to contents
Diagnostic methods
Unfortunately, people usually come to our clinic in the later stages of the disease after endless and fruitless consultations with highly specialized specialists. For diagnosis, special questionnaires and questionnaires are used. The psychotherapist’s task is to exclude other forms of depressive disorders, psychoses, and age-related neuropsychiatric disorders.
Immediately after confirmation of the diagnosis, we recommend starting a course of psychotherapy. However, if the patient's symptoms persist after 2–3 weeks, it is better to undergo a repeat diagnostic examination to rule out concomitant diseases.
Cost of services
| CONSULTATIONS OF SPECIALISTS | |
| Initial consultation with a psychiatrist (60 min.) | 6,000 rub. |
| Repeated consultation | 5,000 rub. |
| Consultation with a psychiatrist-narcologist (60 min.) | 5,000 rub. |
| Consultation with a psychologist | 3,500 rub. |
| Consultation with Gromova E.V. (50 minutes) | 12,000 rub. |
| PSYCHOTHERAPY | |
| Psychotherapy (session) | 7,000 rub. |
| Psychotherapy (5 sessions) | 30,000 rub. |
| Psychotherapy (10 sessions) | 60,000 rub. |
| Group psychotherapy (3-7 people) | 3,500 rub. |
| Psychotherapy session with E.V. Gromova (50 minutes) | 12,000 rub. |
| TREATMENT IN A HOSPITAL | |
| Ward for 4 persons | 10,000 rub./day |
| Ward for 3 persons | 13,000 rub./day |
| Ward 1 bed VIP | 23,000 rub./day |
| Individual post | 5,000 rub. |
| PETE | 15,000 rub./day |
This list does not contain all prices for services provided by our clinic. The full price list can be found on the “Prices” , or by calling: 8(969)060-93-93. Initial consultation is FREE!
Treatment
Psychotherapy sessions are conducted both individually and in groups. Therapeutic effects are aimed at:
- reduction of anxiety;
- behavior correction;
- increased self-control;
- training in relaxation techniques;
- improvement of psychological well-being;
- increasing self-esteem.
Rational psychotherapy,
, has a good effect . The doctor tells the patient in detail what hypochondriacal depression is and explains the need for treatment.
But in severe cases of the disease, psychotherapy alone is not enough. Doctors at our clinic prescribe (necessarily with individual dose selection):
- antidepressants;
- benzodiazepine tranquilizers;
- mood stabilizers and anxiolytics;
- neuroprotectors, etc.
You can get more detailed information about the treatment of hypochondriacal depression at the Leto clinic from our operators by calling 24 hours a day 8(969)060-93-93.
Symptoms of hypochondriacal neurosis
The hypochondriacal type of neurosis is characterized by patients' confidence that they have a fatal disease. Among the symptoms described are weakness, malaise and other signs of various pathologies. As a rule, patients consult medical reference books, after which their confidence in the presence of the disease becomes stronger.
A typical sign is that patients claim that their test results are inaccurate and that their treating physicians are inattentive and incompetent. The state of extreme dissatisfaction extends to all areas of life, and in general the patient's character becomes irritable and hot-tempered.