Mechanism of development of liquorodynamic disorders
There are several main mechanisms for the development of cerebrospinal fluid dynamics disorders.
1) An increase in the rate of secretion of cerebrospinal fluid (CSF) by the choroid plexuses.
2) Slowing the rate of cerebrospinal fluid resorption from the subarachnoid space due to obliteration of the cerebrospinal fluid channels after inflammatory diseases of the meninges or subarachnoid hemorrhages.
3) Slowing down the rate of cerebrospinal fluid production against the background of normal reabsorption of cerebrospinal fluid. Against this background, intracranial hypertension or intracranial hypotension may develop.
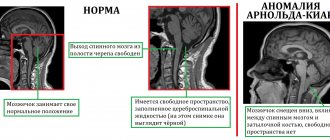
The rate of secretion and resorption of cerebrospinal fluid is influenced by the state of cerebral hemodynamics and the blood-brain barrier. An increase in brain volume due to edema or the development of intracranial space-occupying processes leads to increased intracranial pressure. Intracranial hypertension is observed when the patency of the cerebrospinal fluid ducts is preserved, as well as when they are occluded at various levels, which leads to excessive accumulation of cerebrospinal fluid in cavities located above the level of blockage. In case of liquorodynamic disorders, changes in cerebral hemodynamics are observed. With intracranial hypertension, due to malnutrition of the brain parenchyma, partial atrophy of the brain occurs over time, which leads to the development of hydrocephalus. If there is a process that occludes (blocks) the cerebrospinal fluid pathways, then hydrocephalus develops above the level of occlusion (blockage).
Classification of liquor dynamics disorders
Neurologists, neuropathologists, neurosurgeons, and reflexologists divide all disorders of secretion, resorption and circulation of cerebrospinal fluid into 2 groups.
1. Associated with changes in the volume of circulating cerebrospinal fluid - intracranial hypertension syndrome - intracranial hypotension syndrome - cerebrospinal fluid dystonia syndrome.
2. Caused by blockage of the cerebrospinal fluid pathways - occlusive syndromes, with complete occlusion (blockage) and partial occlusion.
Diagnosis of pathologies
Currently, there are several methods for diagnosing liquorodynamic disorders. The basis in this case is complaints and the clinical picture. In order for the doctor to make a more accurate diagnosis, it is necessary to initially talk with the patient, ask him about the complaints, the time of their appearance, duration, as well as the conditions against which they appear.
The accuracy of the diagnosis and the reduction of possible examinations are reduced after examining the patient; it is preferable to do this not during a period of calm and absence of a clinic, but at the moment of manifestation of the disease.
An examination is carried out, great attention is paid to checking nystagmus and palpation of muscles, especially the occipital muscles. After this, instrumental and laboratory diagnostic methods begin.
Laboratory
The most common and economically less expensive is a general blood test. It indirectly determines the presence of an inflammatory process. This is necessary to confirm or, conversely, exclude a possible cause of the disease.
Cerebrospinal fluid examination. The method is less common and requires highly trained specialists for this manipulation. With its help, the nature of the contents contained in the cavity of the brain and spinal cord is clarified. In case of liquorodynamic disorders, an increase in protein content may be detected. A mandatory point is the complete absence of an inflammatory component.
There are many more instrumental diagnostic methods compared to laboratory ones, and in addition, they have greater diagnostic value. Among them are the following:
- Ultrasonography. It allows you to evaluate not only the structures of soft tissues, but also possible mechanical causes that create a violation of the outflow of fluid.
- Angiography is a method for determining the condition of the vascular component of the body. In cases of liquorodynamic disorders, examination of the vessels of the head and neck is of great importance. With its help, you can identify even small disorders that give a clinical picture of the disease.
- Echoencephalography. This is a non-invasive way to detect pathological changes in the transmission of nerve impulses at the level of the brain substance.
- Computer or magnetic resonance imaging . These are ways to assess the state of brain structures, the volume of cavities and the sizes of component parts. Recently, the technique has become very popular due to the high accuracy of the resulting image compared to the previously common method of x-ray examination. Its significant disadvantage is high economic costs, as well as in some regions inaccessibility.
It is after a correctly developed diagnostic plan and the data obtained that the issue of selecting treatment is decided. It is useless to treat only symptoms, as this can lead to more rapid development of complications.
Symptoms of cerebrospinal fluid dynamics disorders
Intracranial hypertension syndrome
Intracranial hypertension syndrome develops as a result of a persistent increase in intracranial pressure above 200 mm of water column. Synonyms for intracranial hypertension syndrome are hypertensive syndrome, hypertensive syndrome.
Symptoms of intracranial hypertension syndrome, hypertension syndrome, signs of fluid-fluorodynamic disorders, symptoms of hypertensive cerebral syndrome
The clinical picture of hypertension syndrome is determined by the rate of increase in intracranial pressure. A characteristic symptom of this syndrome is a bursting headache (bursting headache), which occurs due to irritation of the receptors of the dura mater and intracranial vessels. In the initial period, the headache can be paroxysmal, usually manifests itself in the morning, and intensifies after physical activity. Later, the headache becomes constant and periodically intensifies. In young children, specialists from private medical practice in Saratov judge the presence of headaches by restless behavior and periodic crying. At the height of the headache, nausea and vomiting are often observed, which bring short-term relief. Autonomic reactions are noted in the form of increased sweating, changes and fluctuations in the child’s body temperature. At subsequent stages of development of intracranial hypertension, congestion in the fundus of the eye, disorders of higher nervous activity, delayed speech development, and delayed mental and motor (psychomotor) development in young children appear. Also observed are rapid heartbeat (tachycardia), disturbance of consciousness, and generalized clonic-tonic (tonic-clonic) convulsions. The final terminal stage of the disease is characterized by profound disturbances of consciousness (coma, stupor), the transition of tachycardia to bradycardia, and respiratory rhythm disorder. Manifestations of hypertension syndrome develop against the background of symptoms of the underlying disease. In young children, as intracranial pressure increases, there is an increase in the size of the head, fontanels, divergence of the sutures on the skull, and an increase in the venous pattern on the scalp. In older children, changes in the bones of the skull are manifested by increased vascular grooves, the appearance of digital impressions, and porosity of the dorsum sella.
Intracranial hypotension syndrome
Intracranial hypotension syndrome develops with a persistent decrease in cerebrospinal fluid pressure below 100 mm H2O. Art. Synonyms for intracranial hypotension syndrome are hypotensive syndrome, hypotensive syndrome.
Primary intracranial hypotension is quite rare. More often it develops as a result of liquorrhea (loss of cerebrospinal fluid), which can be observed after therapeutic and diagnostic interventions on the cerebrospinal fluid tract, as well as with arterial hypotension or an overdose of dehydrating drugs. The main symptom of intracranial hypotension is a headache, often of a squeezing nature (squeezing pain), which is relieved by lying down with the head down or by pressing the jugular veins. With intracranial hypotension syndrome, general weakness, dizziness, nausea, vomiting, and tachycardia are also observed. With a pronounced decrease in intracranial pressure, disorders of consciousness are observed from mild to stupor and coma.
CSF dystonia syndrome
CSF dystonia syndrome is characterized by instability of intracranial pressure and frequent changes. The symptoms of cerebrospinal fluid dystonia are the same as those of hypertension syndrome and hypotension syndrome.
Occlusive syndromes, Brunx attack
Occlusive syndromes develop as a result of blockade of the cerebrospinal fluid pathways at any level of the ventricular system. Clinically, occlusive syndromes are characterized by intracranial hypertension in combination with symptoms of damage to parts of the brain lying above the level of occlusion and the underlying disease. They are accompanied by Bruns' attacks. Bruns' attack has a number of symptoms - vomiting, rapidly increasing headache, impaired consciousness, forced head position, signs of brain stem dislocation.
Obstruction to the outflow of cerebrospinal fluid can occur at any level of the ventricular system.
Vascular type of headache
The arteriodilatatory variant of the vascular type of pain is associated with a decrease in the tone of the craniocerebral arteries, which occurs when the blood vessels are excessively stretched by the pulse volume of blood. Excessive pulse stretching of the hypotonic arterial wall sometimes occurs at normal levels of systemic blood pressure, but more often when it increases. If the artery of the soft integument of the head (superficial, temporal artery) is subjected to excessive pulse stretching, then compression of the adductor trunk of the artery in the temporomygomatic region with a finger, as a rule, reduces pain.
Clinic: throbbing headache. When permeability is impaired and plasma impregnation of the arterial wall develops perivascular edema. In these cases, the amplitude of the pulsation decreases and the headache loses its pulsating character, becomes dull, then aching or bursting.
Therapy: anti-migraine drugs containing ergotamine, dihydroergotamine, sumatriptan are used to relieve pain. Ergotamine drugs relieve pain due to a powerful vasoconstrictor effect and prevent neurogenic inflammation. Ergotamine in combination with caffeine or with caffeine and dimenhydrinate is prescribed as monotherapy or in combination with analgesics, antiemetics and sedatives.
For vegetative-vascular dystonia, xanthine-type drugs are prescribed: aminophylline, pentoxifylline, xanthinol nicotinate, which are usually prescribed in a course 1-2 times a year. This group of drugs acts on smooth muscles, relaxing them, relieves spasm of blood vessels, reduces pressure in the pulmonary artery system, has a diuretic effect, and also inhibits platelet aggregation.
The arteriospastic variant occurs with spasm of the craniocerebral arteries and with an increase in arterial tone, which entails ischemic dyscirculation and ischemic hypoxia.
Clinic: the pain is aching and dull in nature, and is perceived as a feeling of compression. Pain, as a rule, is accompanied by nausea, unsystematic dizziness, darkening and flickering of “black spots” in the eyes.
Therapy: antispasmodic drugs are prescribed: phosphodiesterase inhibitors (papaverine, drotaverine), α-adrenergic blockers (dihydroergotoxin, nicergoline), calcium antagonists (nifedipine, nimodipine). For hypertension associated with impaired blood supply to the brain, drugs that improve cerebral circulation are used. Among the prescription drugs of this series, the most famous are the cerebrovasodilator vinpocetine, BMCA cinnarizine, piracetam, nicotinoyl gamma-aminobutyric acid. It must be remembered that these drugs are contraindicated in patients with acute cerebrovascular accidents, gastric and duodenal ulcers.
The venous variant is caused by excessive blood filling of the venous vessels and difficulty in venous outflow.
Clinic: a feeling of heaviness in the head and a feeling of dull distension. It occurs or worsens when lying down, as well as when working with your head low, as well as when straining or coughing. Morning headache is typical. Sometimes the pain is limited only to the back of the head.
Therapy: drugs of choice are also xanthine drugs, due to their venotonic effect and ability to reduce platelet aggregation, as well as mild venotonics, for example diosmin + hesperidin.
Diagnosis of liquorodynamic disorders,
Diagnosis of liquor-dynamic disorders is carried out using a lumbar puncture with a change in liquor pressure. Computed tomography of the brain (CT), electroencephalography (EEG), ECHO-EG, angiography, pneumoencephalography, MRI, and nuclear MRI are also performed.
Treatment of intracranial hypertension syndrome, liquorodynamic disorders, hypertensive-hydrocephalic syndrome in Saratov, Russia
Sarclinic in Saratov provides conservative treatment of intracranial hypertension syndrome in children of various ages, intracranial hypotension syndrome and dystonia. All treatment methods are painless and safe. Treatment includes a variety of reflexology techniques, linear segmental reflexology massage methods, gua sha therapy, acupuncture techniques, laser reflexotherapy, tsubotherapy, and other reflexology methods.
How to treat liquor-dynamic disorders, how to cure hypertension syndrome, how to get rid of intracranial hypertension syndrome, how to cure hypertensive-hydrocephalic syndrome in children and adults
Complex differentiated treatment of sick children with hypertension, hypertensive-hydrocephalic syndrome and other benign disorders of liquorodynamics with the widespread use of effective reflexology techniques allows achieving satisfactory results even with severe neurological disorders.
Treatment of intracranial pressure
Intracranial pressure needs to be normalized and treated. An integrated approach to the problem, even after the first courses of treatment, even in severely ill patients, gives positive dynamics, speech and psychomotor development in children improves. The earlier treatment is started, the faster the impaired functions are restored and intracranial pressure is normalized. At the first consultation, the doctor will tell you about the main factors and symptoms of the disease: what is hypertension syndrome in newborns, infants, infants, children, children, adults, what is mild, moderate, severe cerebral hypertensive syndrome , hypertensive syndrome , cerebrospinal fluid hypertensive syndrome , how the army and residual encephalopathy are related to hypertensive hydrocephalic syndrome, what intracranial pressure should be normal, how to measure, determine, check, and how to reduce, lower, relieve, treat intracranial pressure. On the website sarclinic.ru you can see a doctor online for free.
Sign up for a consultation. There are contraindications. Specialist consultation is required. Photo: Sergiyn | Dreamstime.com\Dreamstock.ru. The people depicted in the photo are models, do not suffer from the diseases described and/or all similarities are excluded.
Related posts:
Minimal brain dysfunction in children, treatment of mmd in children
Cerebrasthenic syndrome: treatment, symptoms in children, adults
Movement disorder syndromes (muscular dystonia, cerebral palsy)
Tics, nervous tics, treatment, hyperkinesis, hyperkinesis treatment
Sleepwalking in children, adults, treatment, somnambulism, sleepwalking