Quick transition Treatment of vestibular neuronitis
Vestibular neuronitis (VN) is a disease of the peripheral vestibular system. It is characterized by the acute onset of severe systemic (rotational) dizziness and severe imbalance, which are accompanied by nausea and vomiting.
VN ranks third among all causes of peripheral vertigo after benign paroxysmal positional vertigo (BPPV) and Meniere's disease and first among causes of rotational vertigo lasting more than 24 hours.
The annual incidence of VN ranges from 3.5 to 15.5 people per 100,000 population. Both men and women are susceptible to the disease; the peak of VL occurs at 40-50 years of age.
Pathogenesis
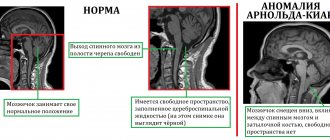
Normally (from the vestibular receptors at rest), the same sensory signal travels along the vestibular nerves in both directions. It is transmitted to the nuclei of the brain stem through the vestibular nerves. In LN, the pathological process reduces the signal from the affected side, causing an asymmetry in the tone of the brainstem nuclei. This leads to oculomotor disorders (nystagmus - involuntary oscillatory movements of the eyes), disturbances of perception (rotational vertigo), postural disorders (imbalance at rest and during movement), autonomic disorders (nausea, vomiting).
Symptoms and course of the disease
VL is characterized by a monophasic course—an acute or subacute onset followed by subsidence of symptoms. The duration of clinical manifestations ranges on average from 1 week to 3 months (maximum manifestations range from several days to several weeks), after which the disease disappears without a trace. The probability of VN recurrence is 2-5%.
The disease begins with severe dizziness, accompanied by a certain type of nystagmus. Dizziness increases with head movements and decreases with fixed gaze. In 78% of cases, it appears suddenly; in 22% of patients, 1-2 days before the onset of the disease, phenomena in the form of instability and slight loss of coordination of movements are noted. Oscillopsia is often observed - unclear visual perception of surrounding objects when performing passive or active head movements due to instability of the image on the retina. Coordination of movements and balance are sharply impaired. Almost all patients experience nausea, and 65% have vomiting.
During the first day, the patient lies in bed - the slightest movements of the head provoke nausea and vomiting. On the 2-5th day, the patient is able to move within the room (ward), but the gait remains unsteady, and sudden head movements or walking long distances provoke nausea. On the 10-14th day, the patient complains of “heaviness” in the head and fatigue, but overall he feels healthy and can return to his usual lifestyle.
In the first days of the development of the disease, the brain “understands” that the vestibular apparatus is transmitting an incorrect sensory signal: the healthy labyrinth is always in an active state, the other (affected) labyrinth is depressed, which is interpreted by the brain as a constant rotation in the healthy direction. Since it is impossible to restore conduction along the affected vestibular nerve in a short time, the brain blocks the activity of the healthy labyrinth, aligning the flow of sensory signals from both vestibular apparatuses. As the vestibular nerve recovers, the control system returns to its original, healthy state.
Treatment
Treatment of vestibular neuronitis should be aimed at reducing the degree of dizziness, stopping vomiting (symptomatic therapy), as well as accelerating vestibular compensation.
Symptomatic therapy comes down to the prescription of so-called vestibular suppressants. The drug of choice in this case is dimenhydrinate in dosages of 50–100 mg 4 times a day at regular intervals. Metoclopramide, benzodiazepines, and phenothiazines may also be used. For vomiting, injectable forms of drugs are used (cerucal, latran intramuscularly). The duration of therapy with vestibular suppressants is determined by the severity and duration of the presence of dizziness; they are rarely used for more than 3 days, because symptomatic therapy with drugs of this series inhibits recovery, although it brings relief to the patient.
To restore vestibular function, the best way is to use vestibular gymnastics; you can learn more about the exercises by clicking on the appropriate link. The combined work of the vestibular, visual and proprioceptive analyzers makes it possible to correct sensory mismatch. It should be remembered that the first days of doing the exercises may lead to some deterioration in well-being, but therapy should not be stopped. The tactics of vestibular rehabilitation and the nature of the exercises directly correlate with the stage of neuronitis; you can see this relationship in more detail in the table in the figure below.
The positive use of methylprednisolone in stepwise therapy with gradual withdrawal of the drug has also been shown. The use of antiviral antiherpetic drugs (valaciclovir, acyclovir, etc.) did not show an improvement in the restoration of vestibular function.
To accelerate the development of mechanisms of central vestibular compensation in combination with vestibular gymnastics, it is recommended to use betahistine hydrochloride preparations (the original drug Betaserc) in a course with a daily dosage of 48 mg (24 mg 2 times a day or 16 mg 3 times a day). Due to the agonistic effect on H3 histamine receptors, there is an increase in the release of neurotransmitters, exerting an inhibitory effect on the vestibular nuclei in the brain stem. Research suggests that betahistine may accelerate vestibular compensation mechanisms.
Diagnostics
In the vast majority of cases, diagnosis is based on a typical clinical picture. The diagnosis can be confirmed using videonystagmography (recording the movement of the eyeballs during a series of tests), the head impulse test (a test that evaluates the functionality of 6 semicircular canals at once - a component of the inner ear responsible for coordination) and the Fuduko test (a marching test that evaluates deviation of the patient from the original position). In addition, patients with VN exhibit spontaneous horizontal rotatory nystagmus, which intensifies when looking towards the healthy ear.
Other tests and studies, including audiometry (hearing tests) and MRI of the brain, are performed as indicated to rule out other causes of dizziness.
Differential diagnosis
VN is also differentiated (distinguished) from labyrinthitis, Meniere's disease, BPPV, neuroma (tumor) of the VIII pair of cranial nerves, multiple sclerosis, stroke, vestibular migraine.
Treatment of vestibular neuronitis
The main directions of treatment for patients with VN are reducing dizziness, nausea and vomiting (symptomatic treatment) and accelerating vestibular compensation.
Symptomatic treatment includes the use of drugs that suppress vestibular function: antihistamines (dimenhydrinate); benzodiazepine tranquilizers (diazepam); antiemetics (metoclopramide hydrochloride, thiethylperazine).
Symptomatic treatment is recommended for no more than 3 days, since it slows down vestibular compensation, which leads to long-term dizziness.
The effectiveness of glucocorticosteroids, which were previously actively used in patients with LN, is currently being questioned. We do not recommend their use, as there is no convincing evidence of accelerated vestibular nerve recovery in these patients.
Despite the presumed viral etiology of VN, associated in particular with herpes simplex virus type 1, the use of antiherpetic drugs also does not accelerate the recovery process, and they should not be used in the treatment of VN.
Piracetam, Trental, Mexidol, Actovegin, Cavinton, glycine and other drugs with unproven effectiveness are not recommended for the treatment of VN.
From about the third day of the disease, patients with VL are recommended to perform vestibular gymnastics - exercises that accelerate compensatory processes, from simpler to more complex. These are exercises for fixing the gaze, training oculomotor reactions, and maintaining balance in various postures while standing and in motion.
Vestibular neuronitis
During examination in the hospital emergency department, horizontal nystagmus directed to the left was noted. In the Romberg test, the patient deviated to the right. There were no other focal neurological symptoms. The dizziness continued for about 5 hours, gradually weakening. However, due to instability and nausea worsening with movement, he was almost unable to walk; I took a few steps only with support. Over the next two weeks, the condition gradually improved: attacks of systemic dizziness did not recur, instability occurred only with sudden movements and quickly getting out of bed. The occurrence of acute vestibular dizziness in a patient who suffered from acute respiratory viral infection a few days ago, the absence of focal neurological symptoms with the exception of horizontal nystagmus and vestibular ataxia, the course of the disease in the form of gradually (within several hours) decreasing dizziness and vestibular ataxia, persisting for several weeks and also gradually regressing, allowed us to diagnose vestibular neuronitis in the patient. What are the tactics for treating vestibular neuronitis in the acute period, what should be the rehabilitation, and what is the likelihood of relapse? The clinical picture of vestibular neuronitis was first described by Eric Ruttin in 1909 and then in more detail by Carl Nielen in 1924. The term vestibular neuronitis was coined by Charles Hallpike in 1949. Vestibular neuronitis is the third most common cause of acute vestibular vertigo after benign paroxysmal positional vertigo and Meniere's disease. The disease predominantly occurs between the ages of 30 and 60; men and women are affected equally often. Etiology and pathogenesis The etiology and pathogenesis of vestibular neuronitis are not completely clear. The disease is associated with selective inflammation (viral or infectious-allergic origin) of the vestibular nerve, as indicated by the results of a few pathomorphological studies. Viral etiology (most often herpes simplex virus type 1) of vestibular neuronitis is supported by the frequent development of the disease after a respiratory viral infection, the epidemic nature of the disease with a peak incidence occurring in late spring and early summer, as well as cases of simultaneous illness of several members described in the literature. families. The role of the herpes virus is confirmed by cases of the development of herpetic encephalitis with vestibular neuronitis. Vestibular neuronitis usually affects the superior branch of the vestibular nerve, which innervates the horizontal and anterior semicircular canals, as well as the elliptical sac of the labyrinth vestibule, as indicated by the frequent combination of vestibular neuronitis with benign paroxysmal positional vertigo, which is usually caused by otolithiasis of the posterior semicircular canal, innervated by the inferior branch of the vestibular nerve . Damage to the inferior branch of the vestibular nerve is much less common. Clinical presentation and diagnosis Vestibular neuronitis manifests itself as a sudden and prolonged attack of systemic dizziness, accompanied by nausea, vomiting and imbalance. The disease may be preceded by a respiratory viral infection. Sometimes, several hours or days before the development of an acute vestibular attack, patients experience brief episodes of dizziness or unsteadiness. Symptoms of vestibular neuronitis increase with head movements or changes in body position. Dizziness may improve with fixed gaze. Spontaneous nystagmus is characteristic, the fast phase of which is directed towards the healthy ear. The imaginary rotation of objects around the patient is also typically directed towards the healthy ear. In the Romberg test, the patient deviates towards the affected ear. Hearing does not decrease. Neurological examination shows no symptoms of damage to the brainstem or other parts of the brain. The duration of dizziness ranges from several hours to several days. Spontaneous nystagmus persists for 3–5 days, nystagmus when the eyes are moved towards the healthy ear in Frenzel glasses (that is, when gaze fixation is turned off) is observed for another 2–3 weeks. After the dizziness stops, patients continue to experience instability for several days or weeks. The timing of restoration of vestibular function depends on the degree of damage to the vestibular nerve, the rate of central vestibular compensation and the patient’s performance of vestibular gymnastics. In many patients, rapid head movements can cause oscillopsia and mild short-term instability for a long time after vestibular neuronitis. According to Okinaka et al., one year after the disease, vestibular function was completely restored in 40% of patients, partially in 20–30% of patients, and in other cases, unilateral vestibular areflexia remained. However, even in the absence or incomplete recovery of vestibular function, patients usually do not experience significant changes in daily activities due to vestibular compensation. In many patients who have suffered vestibular neuronitis, complaints of dizziness reflect an existing somatoform disorder. Vestibular neuronitis rarely (in 2% of cases) recurs; when the disease recurs, the “healthy” vestibular nerve is affected. If a patient who has been diagnosed with vestibular neuronitis has repeated attacks of vestibular vertigo, then other causes of vertigo should be looked for, among which the most common are Meniere's disease, benign paroxysmal positional vertigo and vestibular migraine. The diagnosis of vestibular neuronitis is based on the clinical picture of the disease: acute and relatively long-term (from several hours to several days) vestibular dizziness, accompanied by instability, horizontal or horizontal-rotatory spontaneous nystagmus with oscillopsia, nausea and vomiting. The diagnosis can be confirmed using a caloric test, which reveals vestibular hypo- or areflexia on the affected side. In a rare lesion of the inferior branch of the vestibular nerve, the caloric test is negative, but vestibular neuronitis is confirmed by changes in vestibular evoked potentials. Indirect signs of vestibular neuronitis can be detected using high-resolution magnetic resonance imaging (MRI) of the brain with gadolinium. Differential diagnosis is carried out with other conditions manifested by prolonged vestibular vertigo. Unlike vestibular neuronitis, acute labyrinthitis often occurs against the background of a systemic infection or acute otitis media and is accompanied by hearing loss. Perilymphatic fistula usually occurs after cranial trauma, barotrauma, severe coughing or straining, and is accompanied by hearing loss, confirmed by a fistula test. A stroke in the vertebrobasilar system is accompanied by other focal neurological disorders, central nystagmus, and brain damage according to MRI. Vestibular neuronitis is often difficult to distinguish from the first attack of Meniere's disease, which is more likely if the dizziness is accompanied by tinnitus, a feeling of fullness in the ear, and hearing loss. Treatment Treatment is aimed at reducing dizziness, nausea and vomiting (symptomatic treatment) and accelerating vestibular compensation. Symptomatic treatment includes the use of drugs belonging to the group of vestibular suppressants. The drug of choice is dimenhydrinate at a dose of 50–100 mg every 6 hours. Instead of dimenhydrinate, metoclopramide, benzodiazepine tranquilizers and phenothiazines can be used. For vomiting, use the parenteral route of administration (diazepam IM, metoclopramide IM, thiethylperazine IM or rectally in suppositories). The duration of use of vestibular suppressants is determined by the duration and severity of dizziness; they are generally not used for more than three days because these drugs slow down vestibular compensation. To speed up the restoration of vestibular function, vestibular gymnastics is recommended, which includes exercises in which movements of the eyes, head and torso lead to sensory mismatch. These exercises stimulate central vestibular compensation. However, performing them at first can be associated with significant discomfort. The tactics of vestibular rehabilitation and the nature of the exercises depend on the stage of the disease, which reflects the contents of Table 1. In patients with vestibular neuronitis, the use of methylprednisolone in the first three days of the disease (in an initial dose of 100 mg, followed by a dose reduction of 20 mg every three days) leads to a higher the frequency of restoration of vestibular function one year after the disease. Despite the presumably viral nature of the disease, the use of antiherpetic drugs in patients (alone or in combination with methylprednisolone) does not improve the recovery process. To accelerate vestibular compensation, in combination with vestibular gymnastics, you can use betahistine dihydrochloride (Betaserc 24 mg) 48 mg per day (1 tablet 24 mg 2 times a day). This drug, by blocking NS receptors of the central nervous system, increases the release of neurotransmitters from the nerve endings of the presynaptic membrane (histamine prevents the release of neurotransmitters), having an inhibitory effect on the vestibular nuclei of the brain stem. Experimental studies have shown that betahistine accelerates vestibular compensation. In an animal experiment, Betaserc had a dose-dependent effect on the electrical activity of polysynaptic neurons in the vestibular nuclei.
References 1. Albera R., Ciuffolotti R., Di Cicco M. et al. Double–blind, randomized, multicenter study comparing the effect of betahistine and flunarizine on the dizziness handicap in patients with recurrent vestibular vertigo'// Acta Otolaryngol. –2003. – Vol.123. –P. 588–593. 2. Arbusow V, Schulz P, Strupp M et al. Distribution of herpes simplex virus type I in human geniculate and vestibular ganglia: implications for vestibular neuritis. Ann Neurol–1999.–v.46.–p.416–419 3. Baloh RW Vestibular neuritis. N Engl J Med. –2003. –v348. –p. 1027–1032. 4. Bartal–Pastor J. Vestibular neuritis: etiopathogenesis // Rev Laryngol Otol Rhinol (Bord). –2005. – Vol.126: 279–281. 5. Brandt T. Vertigo. Its Multicensory Syndromes. – 2nd Ed. – London, 2000. 6. Fetter M, Dichgans J. Vestibular neuritis spares the inferior division of the vestibular nerve. Brain 1996. –Vol. 119:755–763. 7. Domingues MO Treatment and rehabilitation in vestibular neuritis // Rev Laryngol Otol Rhinol (Bord). 2005. – Vol. 126:283–286. 8. Gacek RR, Gacek MR The three faces of vestibular ganglionitis. Ann Otol Rhinol Laryngol –2002. –v.lll. –p. 103–114. 9. Godemann F., Siefert K. et al. What accounts for vertigo one year after neuritis vestibularis – anxiety or a dysfunctional vestibular organ? // J Psychiatr Res – 2005.–Vol. 39:529–534. 10. Halmagyi GM, Aw ST, Karlberg M. Et al. Inferior vestibular neuritis // Ann NY Acad Sci. 2002. –Vol. 956:306–313. 11. Heinrichs N., Edler C. et al. Predicting continued dizziness after an acute peripheral vestibular disorder // Psychosom Med –2007. – Vol 69: 700–707. 12. Huppert D, Strupp M, Theil D, et al. Low recurrence rate of vestibular neuritis: a long–term follow–up. Neurology. –2006. –v.67. –N10. –p. 1870–1871. 13. Karlberg M., Annertz M, Magnusson M. Acute vestibular neuritis visualized by 3-T magnetic resonance imaging with high-dose gadolinium // Arch Otolaryngol Head Neck Surg –2004. – Vol. 130:229–232. 14. Okinaka Y, Sekitani T, Okazaki H et al Progress of caloric response of vestibular neuronitis. Acta Otolaryngol. –1993. –v.503. –p. 18–22. 15. Philpot SJ, Archer JS Herpes encephalitis preceded by ipsilateral vestibular neuronitis // J Clin Neurosci. –2005. – Vol.12: 958–959. 16. Strupp M., Zingler VC, Arbusow V. et al Methylprednisolone, valacyclovir, or the combination for vestibular neuritis. N Engl J Med. –2004. –v. 351. – 354–361.