Data
· The syndrome occurs due to a lack of vitamin B1 (thiamine) and involves damage to the hypothalamus.
· More often the occurrence of the disease is associated with excessive alcohol consumption , less often with malnutrition, intestinal diseases, and decreased absorption of vitamin B.
· Wernicke's symptoms include blurred vision, difficulty coordinating the legs, and confusion. Symptoms may disappear and reappear.
· Without treatment, Wernicke's disease often develops into Korsakoff's psychosis.
· The key to successful therapy is stopping alcohol consumption and receiving thiamine B1 in the form of injections.
· If a patient with Wernicke-Korsakoff syndrome cannot independently stop drinking alcohol, he is recommended to undergo body cleansing and be coded.
· Wernicke's syndrome is also called acute upper hemorrhagic polioencephalitis.
What is Wernicke-Korsakoff syndrome?
Wernicke-Korsakoff syndrome consists of two diseases: Wernicke encephalopathy and Korsakoff psychosis. Both are serious complications due to a lack of vitamin B1 (thiamine). The most common cause of the onset and progression of the disease is long-term alcohol abuse . This condition is also observed in people with chronic diseases and can develop as a result of:
· Poor nutrition.
· Intestinal disorders that lead to insufficient absorption of vitamin B.
· Eating disorders and prolonged severe nausea and vomiting .
· Advanced helminthiasis.
· Malignant neoplasms.
· Immunodeficiency syndrome.
· Regular hemodialysis.
All of the above prerequisites significantly increase the chances of acute hemorrhagic polioencephalitis occurring in alcoholism.
Long-term vitamin deficiency causes brain damage, which becomes critical without proper treatment.
Radiation diagnostics
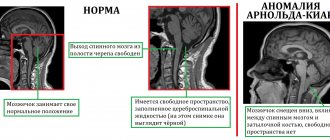
CT diagnosis of Wernicke encephalopathy is usually uninformative, however, in severe cases in the acute stage, a bilateral decrease in the density of the dorsal and medial nuclei of the thalamus can be observed.
MRI semiotics
T1-WI : slight decrease in the MR signal from the periaqueductal gray matter, dorsal and medial nuclei of the thalamus, mamillary bodies; in the chronic stage - manifestations of cerebral atrophy in the form of widening of the intergyral grooves of the cerebral hemispheres and cerebellum, mixed hydrocephalus.
T2-WI : increased MR signal from the structures described above, as well as from the tegmentum of the midbrain due to the involvement of its nuclei.
FLAIR: in this mode, the hyperintense MR signal from the above-described structures is better detected.
DWI: Restriction of diffusion from the above structures may be observed
Contrast-enhanced T1-weighted image: accumulation of contrast agent in the above-described structures is observed
MR spectroscopy: reduced accumulation of N-acetyl-aspartate in the frontal lobes, cerebellum
DIFFERENTIAL DIAGNOSIS is carried out with Alzheimer's disease, multi-infarct dementia, hereditary spinocerebellar atrophies, olivopontocerebellar degeneration, central pontine myelinolysis, other secondary toxic encephalopathies (drug-induced, due to carbon monoxide poisoning, drug addiction).
Fig.1. MRI of the brain in T2-FLAIR mode, axial plane: symmetrical hyperintense foci in the dorsomedial nuclei of the thalamus (curved arrows) and in the projection of the mamillary bodies (straight arrows) [1]
Fig.2. MRI of the brain in T2-FLAIR mode, axial plane (a, b): a - in a patient with a history of chronic alcoholism, minimal expansion of the lateral ventricles (curved arrow) and sulci of the cerebral hemispheres (straight arrow) is determined; b – the same patient 4 years later, there is progression of diffuse atrophy with an increase in the MR signal from the deep parts of the white matter (arrows)[1]
Example of description: ...a symmetrical local increase in the MR signal is determined in T2, T2-FLAIR mode from the dorsomedial parts of the thalamus, mammillary bodies, and periaqueductal gray matter of the midbrain. Subarachnoid convexital spaces and grooves are moderately unevenly expanded in the frontal and parietal lobes due to diffuse cortical atrophy. The lateral fissures of the brain are symmetrical and slightly widened.
CONCLUSION: MRI picture of symmetrical focal changes in the thalamus, hypothalamus and midbrain, diffuse cortical arttrophy; most likely corresponds to manifestations of pathology of toxic-metabolic origin (Wernicke encephalopathy).
How common is Wernicke-Korsakoff syndrome?
· Wernickes occurs in 0.1–2.3% of the population, much more often in alcoholics.
· Obtaining accurate statistics is complicated by the fact that many patients do not seek help and are not diagnosed.
· No more than 20% of all cases of acute hemorrhagic polioencephalitis are recorded during life, and about 80% are discovered during autopsy after death.
· About 17% of all older people have thiamine B1 deficiency and are at risk if they drink alcohol.
Symptoms of Wernicke-Korsakoff syndrome
The first signs of Wernicke's disease are:
· Visual impairment.
Ophthalmoplegia (paralysis of the eye muscles).
· Problems with balance and coordination.
· Memory deterioration and loss of the ability to concentrate on one task for a long time.
· In some cases, lapses in memory.
· Hallucinations and conditions similar to manifestations of delirium tremens.
· Increased anxiety, unreasonable fears.
In 30% of cases, confusion develops into Korsakoff psychosis, the symptoms of the disease increase and manifest themselves in the form of the following conditions:
· Involuntary spasms of the muscles of the tongue, lips, eyelids or cheeks.
· Mumbling to oneself, shouting incoherent phrases, lack of response to speech directed to a sick person.
· Deterioration of the reaction to light stimuli and its complete absence with the worsening of Korsakov's psychosis.
· Rigidity of the neck muscles.
· The tongue becomes bright crimson.
· Changes in muscle tone are observed.
Diarrhea begins .
· Blood pressure changes sharply .
If the disease progresses rapidly and there is no treatment, there is an increase in body temperature to 40 degrees, after 3 days there is a coma, and a week later death occurs.
Alcoholic encephalopathy: acute form
It begins with asthenic phenomena, sleep is disrupted, and appetite decreases. Products containing a high content of fat and protein are rejected by patients. There is a craving for carbohydrate consumption. Changes in diet and lack of essential microelements and vitamins lead to even greater disturbances in the body.
Sometimes an eating disorder leads to anorexia. The stomach and intestines suffer. A feeling of nausea, as well as morning vomiting, is a common occurrence with the disease. They are often accompanied by abdominal pain, heartburn, belching, stool disorders, and increased gas formation. There is a significant likelihood of exhaustion, and in such patients multiple damage to the peripheral nerves (encephalopolyneuropathy) is often detected.
Wernicke's alcoholic encephalopathy
A mental disorder may indicate the development of the classic version of Gaye-Wernicke syndrome. It is accompanied by:
- disturbance of consciousness,
- hallucinations,
- delusional
- changes of emotional and behavioral nature.
Short-term immobility is replaced by long-term motor excitement. The muscles of the human body are in constant tension. Patients are characterized by involuntary screams or delirium.
Against the background of general exhaustion, a patient with this form of alcoholic encephalopathy exhibits swelling of the face. The patient's coordination of movements is impaired. A person exhibits neurological disorders: involuntary oscillatory eye movements, different pupil sizes, decreased muscle strength along with limited movements. Breathing and pulse become more frequent, temperature rises, but blood pressure, on the contrary, decreases. The patient’s well-being and general condition worsens significantly. The tongue of such patients turns crimson, and the liver becomes enlarged. Problems with stool are common. Over time, patients develop and then progress in disturbances of consciousness. Their extreme degree - coma - is characteristic of severe forms of the disease.
From the first symptoms of a mental disorder (delirium) in a person to death, it can take from 10 days to several weeks. Moreover, the probability of death increases if other diseases (pneumonia, bedsores) are added to the main one.
A favorable development of events is when delirium lasts up to one and a half months, and the disease ends with psychoorganic syndrome. Its features:
- psychological helplessness;
- memory problems;
- inability to adapt to everyday life and the surrounding reality; decreased ability to work and stress resistance.
Question: How long do patients live after suffering a serious illness? — it is impossible to answer unequivocally. Everything is individual and depends on the characteristics of the body, as well as on the patient’s compliance with the recommendations of specialists. Acute alcoholic encephalopathy easily turns into a chronic form - this is important to know and remember.
Mitigated acute alcoholic encephalopathy
Mood swings, reluctance to communicate, asthenia, lack of appetite, as well as sleep disturbances may be the first bells indicating mitigated acute encephalopathy. Often such patients are anxious and hyper-suspicious. They are often diagnosed with inflammation of the peripheral intercostal, facial, occipital nerves, as well as the nerves of the lower extremities. The patient can remain in this state for up to two months, after which a mental disorder (delirium) develops.
Even after a long time after recovering from delirium, the patient continues to experience chronic fatigue, lethargy, patients are reluctant to talk, and they have memory disorders that are practically impossible to correct.
Hyperacute form of alcoholic encephalopathy
The disease develops extremely rapidly. Characterized by a high incidence of deaths. The first symptoms appear almost a month before the disease develops. This is followed by a severe mental disorder. The patient has various neurological (polyneuropathy) and somatic disorders. Symptoms of the disease also include:
- a sharp increase in body temperature up to 41 degrees;
- disturbances of consciousness develop.
Within a few days, such a patient can fall into a coma. The possibility of death is extremely high.
Those who survive are susceptible to developing pseudoparalytic syndrome. The state is characterized by imaginary carelessness, when the patient is satisfied with himself and the people around him, and he has no criticism at all. It is difficult to communicate with such patients; they overestimate their capabilities, and their behavior can be called ridiculous and inappropriate.
What symptoms should you pay special attention to?
When symptoms of visual disturbances, balance problems and confusion occur simultaneously and are aggravated by alcohol use, you need to seek help . Particular attention should be paid to:
· occurrence of memory lapses;
· anxiety, obsessive thoughts;
· deterioration of concentration;
· appearance of tremor in the limbs .
Such symptoms are often perceived as a hangover syndrome but in fact it may be the first manifestation of Wernicke-Korsakoff syndrome.
If a person has been abusing alcohol for several years and during a hangover experiences the following symptoms:
· he is shaking ;
· he sweats ;
· does not remember parts of events;
· behaves inappropriately under the influence of alcohol (suspicion of delirium tremens );
· suffers from repeated vomiting;
· feels upset bowel movements (diarrhea ) .
You should immediately call a narcologist to your home and cleanse your body of alcohol .
Wernicke's encephalopathy
The classic triad of symptoms - ophthalmoplegia, ataxia, confusion - is present in only a third of cases. Most patients are deeply disoriented, apathetic, and unable to concentrate; delirium with agitation is sometimes observed as a manifestation of alcohol withdrawal syndrome. Without treatment, stupor and coma may develop and death may occur. Oculomotor disorders include horizontal lateral gaze nystagmus, external rectus palsy (usually bilateral), conjugal eye movement disorder, and rarely ptosis. Ataxia (mainly abasia) is caused by a combination of polyneuropathy, cerebellar and vestibular ataxia. The pupils, as a rule, are not changed, but in the later stages of the disease they may be narrowed.
With timely administration of thiamine intravenously or intramuscularly, oculomotor disorders quickly disappear; only nystagmus is persistent.
Wernicke encephalopathy is usually accompanied by other manifestations of nutritional disorders - in particular, 80% of patients have polyneuropathy. Amblyopia and spinal spastic ataxia are much less common. Tachycardia and orthostatic hypotension are common, which may result from damage to the autonomic nervous system or be symptoms of the wet form of beriberi. Oculomotor disorders disappear within a few hours after administration of thiamine, while ataxia lasts longer, and in about half of the patients, complete recovery does not occur and the gait remains slow, shuffling, with legs widely spaced. Apathy, drowsiness, and confusion also disappear gradually. As these disorders regress, fixation amnesia - Korsakoff's syndrome - may come to the fore. This is a frequent companion to Wernicke's encephalopathy; in fact, we are talking about one disease - Wernicke-Korsakoff syndrome. Often Korsakov's syndrome persists, leaving patients with memory lapses, confabulations, and confusion in the sequence of events.
Course of the disease. About 15-20% of hospitalized patients die, and this is usually due to intercurrent infections (most often pneumonia, pulmonary tuberculosis and septicemia) or liver failure.
If the patient begins to recover, it usually happens as follows. Paralysis of the extraocular muscles can begin to regress within a few hours after administration of thiamine and almost always after a few days. If the patient does not respond to treatment in this way, then doubts arise about the diagnosis of Wernicke's disease. Abducens nerve palsy, ptosis and vertical gaze paresis regress completely within 1-2 weeks, but vertical nystagmus provoked by gaze translation sometimes persists for up to several months. Horizontal gaze palsies usually recover completely, but in more than 50% of patients, clear horizontal nystagmus caused by combined rotation of the eyeballs persists as a persistent consequence of the disease.
Diagnosis of the disease
The syndrome can be assumed based on the characteristic symptoms and the presence of a problem with alcohol in the patient.
To confirm the diagnosis, the following are prescribed:
· Blood analysis;
· CT scan;
· Magnetic resonance imaging with contrast;
· Neurological examination neuromyography to determine neural conductivity;
· 24-hour urine test to determine thiamine levels.
Even the appearance of characteristic symptoms is already a prerequisite for starting therapy and taking vitamin B.
Treatment of Wernicke-Korsakoff syndrome
In the early stages, the disease may show improvement with taking large amounts of vitamin B1 (thiamine). Therefore, it is very important that the patient or his relatives, at the first suspicion of the disease, seek qualified help.
· Thiamine is most often prescribed intramuscularly at 50–100 mg, less often intravenously. Injections are performed 2 times a day until the condition clearly improves, after which vitamin B can be prescribed in tablet form.
· To correct hypomagnesemia (which often develops along with a lack of vitamin B), magnesium sulfate is prescribed intramuscularly, 1-2 milliliters.
· Ascorbic and nicotinic acid.
· Other vitamin complexes.
Before starting treatment, the drinking patient must stop drinking and undergo body cleansing .
When the disease is advanced, such as severe amnesia or aggressiveness, there is no effective treatment. However, thiamine helps in providing relief after months of therapy.
Important: every person who is at risk or susceptible to this disease should regularly take B vitamins for prevention purposes.