- Characteristics of psychosis
- Who's at risk
- Causes
- Symptoms
- Diagnostics
- Treatment
- Forecast
- Prevention
Attention! Drug use causes irreparable harm to health and poses a danger to life!
Alcohol abuse is one of the main causes of diseases of the central nervous system. Korsakov's alcoholic psychosis is a psychotic condition that develops during prolonged alcohol abuse in the second and third stages of alcoholism. It is one of the types of chronic encephalopathy (organic brain damage).
Characteristics of psychosis
Korsakov's alcohol psychosis was previously known as polyneuritic psychosis, and is a mental disorder in patients suffering from chronic alcoholism, combined with polyneuritis. Characterized by severe memory impairment.
The pathology was first described by psychiatrist Sergei Korsakov in 1887. The doctor described a common disease in patients with alcoholism - damage to the peripheral nervous system, combined with memory impairment and spatio-temporal orientation. In 1897, the disease was recognized internationally and named Korsakoff syndrome.
Who's at risk
The average age of patients admitted with alcoholic psychosis is 50-60 years. It was noted that women predominate among the cases. Also at risk are people who have reached the third stage of addiction, who often take various substitutes for alcohol and low-quality alcoholic drinks.
Causes
The development of Korsakoff's psychosis is possible against the background of severe delirium and Gaye-Wernicke syndrome. The disease develops after a series of encephalopathies in patients with alcoholism. But in practice, there have been cases of gradual manifestation of symptoms with systematic intake of alcoholic beverages and progressive alcohol degradation. Rarely does the disease develop in conditions of a relatively favorable emotional state without previous signs of mental disorders.
The main factors causing the development of Korsakov’s alcoholic psychosis:
- acute lack of thiamine (vitamin B1);
- destruction of liver cells, toxic hepatitis, cirrhosis;
- damage to the intestinal mucosa.
Regular intake of alcohol stimulates the work of the small intestine, where the absorption of elements required for the normal functioning of the body occurs. The absorption of vitamins is impaired, which leads to the slow destruction of the limbic structures of the brain.
Vitamin B1 deficiency increases the risk of encephalopathy and delirium. If a patient in this condition does not receive medical care, in 80% of cases Korsakov alcoholic psychosis begins.
Neurological diseases contributing to the development of the syndrome:
- heart attacks and brain cancer;
- encephalitis of any pathogenesis;
- serious head injuries;
- degenerative dementias;
- surgical operations in the treatment of epilepsy.
Get help now
Do any of your relatives or friends have an addiction? Have you tried in every possible way to help, but as a result the person still returned to his past life?
You are not the first to encounter this problem, and we can help you.
We guarantee anonymity, we will persuade you to undergo treatment, and we will help you choose a center.
Call us
+7
or
Call me
results
In all patients, the development of CRS occurred acutely, while in 3 - against the background of acute pancreatitis with severe intoxication, abdominal pain syndrome, repeated vomiting and diarrhea, in 1 - chronic pancreatitis with malabsorption, in 1 - exacerbation of chronic ulcerative colitis, in 1 - after operations for gastric ulcers, in 2 - after surgery on the upper gastrointestinal tract for malignant diseases of the stomach and pancreas. 4 patients had long-term alcohol abuse, but the diagnosis of chronic alcoholism was not established. The demographic and clinical characteristics of the patients are shown in Table. 1.
Table 1. Demographic and clinical characteristics of patients with CRS included in the study Note. GDN - oculomotor disorders, ZR - impaired pupillary reactions, CS - Korsakov's syndrome, MA - cerebellar ataxia, TCS - tonic-clonic seizures; MCI is a moderately severe cognitive disorder.
Neurological and mental disorders arose in patients 24-72 hours after the onset of an acute gastroenterological disorder, manifested by epigastric pain, nausea, repeated vomiting with dysmetabolic disorders and dehydration, or after recovery from surgical anesthesia. CRS debuted with a disturbance of consciousness from somnolence to coma; 4 patients developed delirium, manifested by a disturbance in the level of consciousness, orientation in person, place and time, visual and/or tactile hallucinations. Ataxia, oculomotor disorders, and bulbar syndrome appeared 24-48 hours later. In 1 patient, generalized epileptic tonic-clonic seizures acutely developed, which turned into status epilepticus, resistant to antiepileptic therapy and resulting in death.
During the examination in the acute period of CRS, all patients were found to have disturbances of consciousness: in 5 - a decrease in the level of wakefulness from somnolence to coma, in 3 - psychomotor agitation, in 4 - meningeal syndrome, in 1 - bilateral ptosis, in 4 - impaired pupillary reactions, 3 had oculomotor disorders, 3 had nystagmus, 8 had cerebellar ataxia, 4 had bilateral pyramidal disorders.
A CT scan of the brain in 1 patient with a fatal course of CRS revealed a picture of cerebral edema with the presence of small hyperdense foci in the hemispheres and brain stem. At autopsy, multiple petechial hemorrhages were found in the brain. MRI revealed hyperintense lesions in the hypothalamus, mammillary bodies, brain stem, and cerebellum in 2 patients.
2 patients were treated in the neurological department, the rest were treated in intensive care. Along with treatment of the underlying disease, patients received symptomatic therapy with neuroleptics and bezodiazepines (6), antiepileptic drugs (2), and massive infusion therapy with solutions of colloids and crystalloids. In only 4 patients, the diagnosis of CRS was made in the acute period of the disease and they were prescribed pathogenetic therapy with thiamine; the remaining patients also included vitamin B1 preparations in suboptimal doses in the treatment complex, which may have prevented further development of the disease. Here is one of our observations.
Patient N.
, 23 years old. Diagnosis: Wernicke-Korsakoff encephalopathy, cerebellar ataxia, moderate cognitive impairment, lower mixed paraparesis, severe neurodynamic disorders, subcortical dysarthria.
Concomitant diagnosis: acute destructive pancreatitis, edematous form. Exacerbation of chronic calculous cholecystitis.
Upon admission, complaints of non-systemic dizziness, double vision, general weakness, memory impairment.
Entered the Department of Gastroenterology of the Moscow Regional Research Clinical Institute named after. M.F. Vladimirsky on September 25, 2015 with a diagnosis of chronic biliary pancreatitis in the acute stage. Chronic calculous cholecystitis." Due to the ineffectiveness of conservative therapy, he was transferred to the abdominal surgery department, where on 10/07/15 an operation was performed: diagnostic laparoscopy, cholecystostomy, drainage of the abdominal cavity. In the postoperative period, conservative, antibacterial and symptomatic therapy was carried out.
CT scan of the abdominal organs a week after surgery (10/14/15): showed that the patient has ongoing total-subtotal pancreatic necrosis with infiltrative changes in the surrounding soft tissues and the presence of collectors with dense contents; thickening of the walls of the gallbladder and the likelihood of a small amount of fluid in its bed were noted, as well as infiltrative changes at the level of surgery and the hepatic flexure of the colon.
On 10/21/15, the patient began to experience severe weakness associated with changes in body position, vomiting of eaten food, non-systemic dizziness and headache.
On 10/22/15, the patient was examined by a neurologist, who presumably diagnosed an acute stroke in the vertebrobasilar system and recommended MRI of the brain and MR angiography. But during MRI on 10.22.15, no data on the volumetric process and focal lesions of the brain substance were obtained; only asymmetry of the lumens of the vertebral arteries was revealed (hypoplasia of the left was not excluded).
On 10/28/15, the patient’s condition worsened: the patient was disoriented, drowsy, forgetful, dizziness increased and vision deteriorated. The ophthalmologist noted the presence of phenomena of initial stagnation of the optic discs. The patient was also consulted by an otorhinolaryngologist: no damage to the labyrinth was identified, but it was suggested that there was central vestibular ischemia and hemorrhage in the quadrigeminal region of the midbrain. A dynamic MRI of the brain was recommended.
On October 28, 2015, the patient also underwent a CT scan of the abdominal organs to exclude an increase in the underlying pathology. The preservation of infiltrative changes at the level of the parapancreatic region, porta hepatis, and subhepatic space was noted, although there was a slight decrease in comparison with the previous study. Infiltrative changes in fiber also became less pronounced. A catheter was visible in the lumen of the gallbladder. Otherwise, the condition of the parenchymal organs was without pronounced dynamics. Increased pneumatization of the transverse colon and sigmoid colon is determined. The lumen of the colon contains dense contents. In general, positive dynamics were noted.
On 10/30/15 the patient was consulted by Prof. S.V. Kotov, at the time of examination the patient complained of non-systemic dizziness, double vision and instability when walking. His general condition was assessed as serious. The patient was euphoric, disoriented in place and time, had amnesia for the events of the previous day, and did not control the functions of the pelvic organs. He complied with the doctor’s commands, but quickly became exhausted; answered questions. The level of consciousness was determined to be mildly stunned.
Neurological status: no meningeal syndrome. Cranial nerves: bilateral symmetrical ptosis to the lower third of the pupil. The pupils are symmetrical, reactions to light are lively. Internuclear ophthalmoplegia - when looking to the side, a horizontal medium-wide monocular nystagmus occurs in the extreme abduction in combination with the contralateral eye not reaching the inner corner of the orbit, vertical nystagmus when looking up. The face is symmetrical. Swallowing and breathing are not impaired. Tongue in the midline. Muscle strength in the limbs is diffusely reduced to 4 points. Tendon reflexes are symmetrical, low in the arms, lively in the knees, and absent in the Achilles. The finger-nose test is performed with intention tremor and misses. In the Romberg test it is unstable. No sensory disorders were detected at the time of examination.
Diagnosis: Wernicke-Korsakoff encephalopathy. Ataxia, internuclear ophthalmoplegia, cognitive impairment. Therapy with thiamine 200 mg intravenously twice daily was started.
Lumbar puncture at the time of examination of the patient by a neurologist is contraindicated due to the presence of brainstem symptoms, swelling of the optic discs and the threat of complications.
An MRI of the brain on 10/30/15 revealed damage to the gray matter of the midbrain tegmentum, mammillary bodies, hippocampus and hypothalamus with a slight accumulation of contrast in these areas, characteristic of CRS (Fig. 1).
Rice. 1. MRI of patient N. 10.30.15. 1, 2, 3, 4 — FLAIR, axial sections; 5 — T1-weighted image with gadolinium contrast, sagittal section; 6 — T1-weighted image with gadolinium contrast, coronal section. Symmetrical zones of pathological signal are visible in the tegmentum of the pons (1), midbrain (2), in the hypothalamus region (3), in the medial parts of the visual thalamus (4) on both sides. Accumulation of contrast in the area of the mammillary bodies (5) and periaqueductal gray matter (6).
Metabolic therapy was added to the treatment: a complex of vitamins B1, B6 and B12 (neurobion), choline alfoscerate, alpha-lipoic acid, dexamethasone. The daily infusion volume is 1200 ml.
On 11/03/15 the patient was transferred to the neurological department. His general condition at the time of transfer was moderate.
Respiratory rate 16/min, blood pressure 130/80 mm Hg, pulse 76 beats. per minute, the abdomen is soft, painless, peristalsis is clear, the liver measures 11×8×7 cm, the gallbladder is not palpable, urination is not impaired.
Neurological status: the patient is conscious, there are no meningeal symptoms. The palpebral fissures are symmetrical. Full movement of the eyeballs. The pupils are symmetrical, 6 mm, round. Direct and friendly reactions of the pupils to light are symmetrical and lively. The reaction to convergence with accommodation is reduced. Nystagmus is horizontal, medium-wide, vertical when looking up. Corneal and conjunctival reflexes are symmetrical. The face is symmetrical. There are no vestibular disorders. Phonation and swallowing are not impaired. Reflexes from the soft palate and posterior pharyngeal wall were preserved. Shoulder lift and head rotation are not impaired. Tongue in the midline. The volume of active and passive movements is not limited. Arm muscle strength D=S is characterized by 4 points, leg muscle strength D=S - 3 points proximally and 4 points distally. The tone in the limbs is reduced. Tendon and periosteal reflexes: from the hands D=S, live. Knees and Achilles are missing. Abdominal reflexes are low. There are no pathological reflexes. Performs finger-nose test and heel-knee test with missed hits and dysmetria. No clear sensory disturbances were identified. Mental state: the patient is euphoric, self-oriented, but orientation in place and time is difficult. Memory for current events is reduced. MOCA test - 12 points. There is a positive trend in the state of cognitive functions compared to the results of previous studies.
Consultation with a speech therapist (11.11.15): severe neurodynamic disorders, subcortical dysarthria.
Consultation with an ophthalmologist (11/19/15): the optic discs are pale pink, the borders on the upper and nasal sides are somewhat blurred. The excavation is normal. The retina is without features. Arteries and veins are not changed.
Recommended: diet No. 5; care of a cholecystostomy by a surgeon. Repeated K.T. abdominal cavity after 3 months.
The condition at discharge was satisfactory with positive dynamics during observation: absence of dizziness and diplopia, improvement of cognitive functions, reduction of coordination disorders, increase in strength in the limbs. The clinical picture, however, remained mild cognitive impairment, nystagmus, general weakness and severe weakness in the legs (the patient can move only with assistance).
Observation by a neurologist and an abdominal surgeon is recommended; general regimen, diet No. 5. Considering the impaired absorption of vitamins from the gastrointestinal tract, Neurobion 1 ampoule intramuscularly 2 times a week for a long time was prescribed, choline alfoscerate 0.4 g three times a day orally for 1 month. Exercise therapy, cognitive rehabilitation. Observation by a surgeon. Care for cholecystostomy at the place of residence. CT scan of the abdomen after 3 months.
The patient was examined 3 months after discharge: a general improvement in well-being and regression of neurological disorders were noted, although the patient still had complaints of weakness in the legs and forgetfulness. The neurological status revealed horizontal nystagmus when looking to the sides, bilateral increased tendon reflexes, a slight symmetrical decrease in strength in the legs (up to 4 points), MOCA test - 20 points. It is recommended to continue therapy with Neurobion and metabolic drugs.
Symptoms
The first signs of Korsakov's psychosis may appear in advance, before the onset of the underlying disease (about 2 years), among them:
- body aches;
- pain in the limbs;
- unsteady gait the next day after drinking alcohol;
- sleep problems - insomnia, nightmares;
- increased anxiety;
- fears for no apparent reason.
The disease is characterized by the following clinical manifestations:
- Fixation amnesia. The patient is unable to remember and store new information, events from the recent past and present. At the same time, memories from youth and even childhood are preserved. A mental disorder sometimes manifests itself with such intensity that a person loses the ability to learn, reacts inadequately to household changes, new people in the environment, or moving.
- Retrograde amnesia. The memory of events that preceded the disease or the onset of attacks is lost.
- Amnestic disorientation. The patient is not oriented in space and time, and loses the ability to perform life skills. Loses criticality towards one's own condition. Doesn't understand where he is, seems helpless.
- Confabulation is one of the early signs of the syndrome. The patient creates confused or imaginary versions of events that he cannot remember. Often such stories “pop up” when questioning patients, and not spontaneously. In terms of content, they may include facts from everyday life that sound plausible. Less often, the patient talks about imaginary adventures and incidents, fantastic events.
- Neurological signs - neuritis, accompanied by paresis, more or less pronounced atrophy of the muscles of the limbs, decreased sensitivity, weakness, paralysis. Sometimes tendon reflexes disappear.
General behavioral changes:
- passivity;
- lethargy;
- excessive fatigue;
- dysphoria;
- there is practically no facial expression;
- slow motor skills;
- apathy followed by fussiness;
- irritability;
- defects in visual fields, impaired pupil movement;
- anxiety;
- hypochondriacal disorder;
- decrease in intellectual abilities.
Severe psychosis leads to dementia. If the disease is malignant, there is a risk of death due to brain pathologies.
Korsakoff syndrome in alcoholism
Unfortunately, no matter what measures are taken to treat society from alcoholism and other addictions, the opposite effect occurs. This is especially true for young people. They started drinking more and that’s a fact! For this reason, a number of life-threatening diseases for the dependent and the public have become “younger,” including Korsakoff syndrome in alcoholism. A harmful passion manifests itself through quite tangible signs:
- cramps and pain in the legs at night;
- sparkles in the eyes darkening;
- impaired speech;
- broken connection between thoughts and actions;
- hand shaking (tremor);
- visual and auditory hallucinations;
- sleep disturbance, nightmares;
- excessive anxiety, unreasonable anger, irritability, panic and fear attacks.
A particular difficulty arises due to the fact that the alcoholic categorically does not want to admit his illness, which is alcoholism. And everyone is sure that they can stop drinking at any moment, at the first desire. Therefore, his relatives and friends play a big role in the treatment of the disease. They must pay attention to the following obvious signs:
- the patient loses interest in previous hobbies;
- behaves inappropriately;
- says strange things;
- constantly confused in thoughts;
- gait becomes unsteady;
- gets confused about time and location;
- does not recognize his relatives - wife, children, parents, etc.
He suffers from frequent depression, screams for no reason, makes scandals out of the blue, and constantly argues. May forget recent events - when to say hello again, re-read the newspaper. This is the behavior of a person suffering from addiction. As a rule, most try to avoid his company. Therefore, it is important to pay attention to the condition of a loved one in time and convince him to undergo treatment. Not only the patient, but also his relatives and friends do not always understand that alcoholism is a serious illness that causes mental disorders. Correct diagnosis and complex therapy with a diet rich in proteins and useful elements will restore the body and psyche. And loved ones should remember that there is no alcohol dependent person who does not dream of getting rid of his harmful addiction. All you need to do is help him take the main step - give up alcohol and seek adequate treatment.
Diagnostics
In making a diagnosis, it is important to talk with relatives who will give truthful information about the patient’s behavior, the duration of alcohol dependence, and the presence of previous signs.
Diagnosis of Korsakov polyneuritic alcoholic psychosis involves the following measures:
- Consultation with a psychiatrist and psychologist. Specialists determine the nature of memory loss, disorientation due to amnesia, the presence of accompanying delusional ideas, and confabulation. During the examination, to identify memory problems, the doctor conducts word recall tests and other types of psychological testing for rote and conscious memorization.
- Consultation with a neurologist. The symptoms of polyneuritis are determined. The doctor examines the condition of the limbs to identify muscle atrophy, paresis, and disorders of the musculoskeletal system. Also pays attention to the function of the eye muscles.
- Laboratory research. The patient donates venous blood for biochemical analysis. First of all, it is important to identify vitamin B1 deficiency and the general condition of systems and organs.
- Hardware diagnostics. MRI of the brain, computed tomography of the liver and other organs are performed.
When diagnosing, it is important to differentiate Korsakov's psychosis from other diseases, such as atherosclerosis, dementia, delirium, progressive paralysis, dissociative amnesia, memory impairment due to depression.
The main difference between Korsakov's psychosis and dementia is that the patient is conscious, able to think and answer questions clearly, only memory is impaired.
Clinical signs
The primary clinical signs of this pathology are aching pain in the lower extremities. Spontaneously occurring disorders . They are accompanied by tingling, burning and crawling sensations. It should be noted that these signs of Korsakov’s psychosis occur long before the full clinical picture appears.
If we talk about the symptoms of Korsakoff psychosis, it should be noted that this pathology is often accompanied by:
- unsteadiness of gait;
- sleep disorders;
- the emergence of causeless feelings of anxiety and fear;
- loss of interest in family and work.
Prolonged binge drinking can contribute to a deterioration in mental state, hallucinations and disturbances of consciousness.
Untimely treatment of this pathology can lead to severe amnesia, the appearance of fictitious memories and problems with time orientation. It is worth noting that the patient may not remember current information, but at the same time he will retain old memories .
Severe disorientation in polyneuritic psychosis is accompanied by the inability of patients to name the current date and even the year. They may forget what they said a few seconds ago and not realize where they are at the current moment in time. Gaps in memories are usually replaced by paramnesias. As a result, patients may confuse fictitious and real events. Situations often arise when a person suffering from Korsakov psychosis believes that an event from the distant past occurred relatively recently.
It should be noted that alcohol dependent people suffering from this pathology are often well aware of their problems and try to hide them from others. They retain the ability to operate with situational phenomena. Moreover, in the first minutes of a conversation, patients can give the impression of intelligent and well-mannered people. However, further acquaintance with these people makes it clear that they have mental disorders. Such conclusions can be drawn on the basis of narrow thinking, stereotyping and the introduction of fictitious facts into the conversation.
This disorder is accompanied by affective and asthenic disorders. Alcohol addicts show lethargy, passivity and fussiness. Demonstration of increased excitability and depressive symptoms is also possible.
Other clinical signs of polyneuritic psychosis include:
- confusion;
- carelessness;
- impaired pupil reaction;
- involuntary oscillatory eye movements;
- gaze paralysis;
- paresis of the limbs;
- violations of coordination of movements.
This pathology is presented in two forms - regressive and stationary. In the first case, the severity of clinical manifestations begins to decrease significantly over time, in the second, the intensity of disturbances in the functioning of the central nervous system does not change.
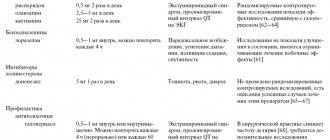
Treatment
After the diagnosis is made, the rehabilitation center prescribes complex therapy aimed at detoxification and restoration of the vital functions of the body. Acute psychosis can only be treated in an inpatient setting.
Therapy is carried out as follows:
- Detoxification: infusion therapy - droppers with saline and glucose.
- Vitamin therapy - a high dose of thiamine is administered (followed by a gradual reduction in dosage). This is an effective way to treat neuritis and any neurotic disorders.
- Drug therapy aimed at restoring cognitive functions, improving memory and concentration of the patient. For this purpose, nootropics (Phesam, Noopept) are introduced. For increased anxiety, antipsychotics (clozapine, pipothiazine) are administered in small doses.
- General condition monitoring. Prescribed for severe disorientation, passivity, and severe amnesia. Medical personnel monitor the daily routine, compliance with hygiene rules, and physical recovery.
- If the patient is bedridden, separate care is required to prevent bedsores and hypoventilation.
- Physiotherapeutic methods. This includes gymnastic exercises, hardware techniques that prevent complications and complete muscle atrophy.
One of the promising means of treating acute alcohol disorders and alcoholism itself is memantine - akatinol. According to research results, the drug improves the cognitive functions of patients suffering from Korsakoff's psychosis, and at the same time demonstrates a chance to reduce the severity of alcohol dependence.
Forecast
Treatment of alcoholic psychosis is characterized by relative effectiveness - the success of the procedures depends on the age category, general physical and mental condition, experience of alcoholism, and ability to adapt.
Memory defects with correct long-term treatment may disappear, but they may remain incurable and even worsen over time.
In general, if prescribed therapy is followed, the prognosis will be favorable. But some problems with thinking and psyche may persist. There is a risk of an unfavorable prognosis if medical assistance is not provided on time. In this case, the disease becomes malignant with a fatal outcome.