This type of brain tumor, such as astrocytoma, is the most common among neoplasms of the central nervous system and accounts for up to 50% of all tumors of the central nervous system. The favorite localization of cerebral astrocytoma is the cerebral cortex, less often - the cerebellum, brainstem and optic nerve. Specialists of the Northern Capital Medical Center help in the early diagnosis of this dangerous disease - our equipment allows us to identify the formation even before the first clinical symptoms appear.
Brain astrocytoma: what is it?
Prices for MRI of the brain What does a brain MRI show? MRI of the head MRI of the brain MRI of the pituitary gland MRI of the orbits MRI of the sinuses
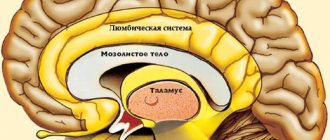
Astrocytoma refers to a tumor of neuroglia in the brain. This is a special tissue that is auxiliary in the central nervous system - it helps transmit signals and supports and nourishes neurocytes. A brain tumor formed from star-shaped cells - astrocytes - is called an astrocytoma.
Brain astrocytoma: causes of occurrence
Scientists have already identified the main factors that are present in most patients with astrocytoma:
- heredity burdened with cancer;
- unfavorable environmental, economic, social factors;
- traumatic brain injury;
- chronic concomitant diseases that cause intoxication of the body;
- hormonal changes in the body, such as pregnancy or menopause;
- excessive consumption of alcoholic beverages;
- occupational hazards (for example, radiation, oil refining or working with paint materials);
- viral infections with a high degree of oncogenicity.
The exact causes of the development of the disease have not yet been sufficiently studied, but it is easy to notice that modern people encounter most of the provoking factors quite often. It cannot be said for sure that these factors are absolute provocateurs of the development of cancer, but it has been proven that they have a detrimental effect on the body as a whole. Therefore, it is necessary to take care of your health and protect yourself from their excessive exposure, conduct timely preventive examinations, and also not delay diagnosis if complaints from the brain arise.
Moreover, malignant gliomas are characterized by a high relapse rate - at least 60-80% after a standard course of radiation treatment, and repeated conventional irradiation is usually limited in terms of tolerance of the nervous tissue, applied radiation dose ranges and timing.
To reduce the number of relapses and improve the results of combined treatment of patients with a number of specific histological types of tumors, chemotherapy is actively used, both in mono regimens and in combination. The combination of radiation and chemotherapy has significantly improved the results of treatment of patients with malignant gliomas, however, the treatment of relapses still remains a difficult task in neuro-oncology.
The emergence of new technical solutions in radiation therapy, the development of the stereotactic direction, in particular the Gamma Knife device, which makes it possible to achieve high conformity and selectivity of irradiation of tumors, reduce the radiation dose to critical structures and increase the dose to the tumor - expands the treatment options for patients, especially with relapses of gliomas after combination treatment.
NON-INVASIVE DIAGNOSTICS OF GLIAL TUMORS
To establish a diagnosis of a glial tumor, a combination of clinical data (history, neurological and neuro-ophthalmological examination) and the results of neuroimaging studies is used: spiral computed tomography (SCT), magnetic resonance imaging (MRI), MR and CT perfusion, as well as radionuclide diagnostic methods : single photon emission computed tomography (SPECT 99cTc - technetium) and positron emission computed tomography with labeled amino acids (11C-methionine)
Despite the improvement of radiological diagnostic methods, a final judgment about the degree of malignancy and type of tumor is possible only on the basis of a biopsy and pathomorphological examination of the tumor.
GLIOMAS OF LOW GRADE (GRADE I-II).
Piloid astrocytomas (PA) Grade I - account for 5-6% of all glial neoplasms with an incidence of 0.37 per 100,000 population per year. These tumors are most common in children (67%), predominantly affecting the cerebellum, optic nerves, chiasm, thalamus, basal ganglia and brainstem structures. The peak incidence occurs in the first two decades of life, with piloid astrocytoma accounting for 21% of all glial neoplasms between the ages of 0 and 14 years.
The gold standard in the treatment of NCC gliomas is a surgical method, which in most cases allows radical removal of the tumor.
Radiation therapy, as an independent method of treatment, is used in patients with small tumors of the visual tract that are difficult to remove, residual tumors after non-radical removal, as well as in the treatment of relapses of PA.
For piloid astrocytomas, radiosurgery with the Gamma Knife device is the method of choice for small tumor remnants after incomplete removal or relapse (Example 1), in cases where repeated surgery is impossible.
Types of brain astrocytomas
According to the degree of malignancy, all astrocytomas of the brain are divided into 4 grades, which differ significantly in course and prognosis.
First degree of malignancy
It includes a benign tumor that has regular boundaries. Pathological cells in it divide evenly and have the same size and shape. The growth of the tumor process is slow, and the main treatment option is surgery. Brain surgery allows you to completely get rid of the tumor if it was detected at this stage. The tumor is common among children with its favorite localization in the cerebellum and brainstem.
The frequency of occurrence among all types of brain astrocytomas reaches 15%. This is the least dangerous variant of the course of the disease, however, if the location of the tumor mass is unsuccessful, even this relatively favorable variety can lead to serious symptoms - this happens if the tumor tissue presses on vital centers in the brain.
Second degree of malignancy
Such a tumor is a neoplasm that has blurred boundaries. Cells multiply more actively than in grade 1, but the growth of the tumor process still remains relatively slow. A characteristic feature of this course is the high frequency of relapses and the young age of patients (approximately 25 years).
Despite the vagueness of the formation, it is still benign, and therefore does not metastasize. But such a tumor has the danger of degenerating into a malignant neoplasm, and this can happen at any time, absolutely unpredictably. Therefore, it is necessary to perform timely surgical treatment and add chemotherapy treatment if necessary.
Third degree of malignancy
Such brain astrocytomas are characterized by higher malignancy and uncontrolled cell division. Cancer cells lose their identity and no longer resemble normal astrocytes. The tumor grows rapidly and has no clear boundaries. This variant of the course is more common among patients aged 40 years, and males are more often affected by the disease.
Treatment is significantly difficult, since metastases appear in the central nervous system quite early. Dissipation of astrocytoma may occur before clinical signs and complaints appear. It is extremely difficult to cure the disease radically at the stage of metastatic screenings, so this variant of the course is considered unfavorable.
Fourth degree of malignancy
The tumor is characterized by a more extensive pathological process and the presence of metastases in the brain and spinal cord. Cancer cells in this case multiply uncontrollably and rapidly; stopping their division is almost impossible at the present stage of development of medical science. The prognosis for patients with such astrocytoma is unfavorable.
It cannot be treated, and all therapy is supportive in nature and is aimed at possibly prolonging the patient’s life, reducing pain and reducing overall negative symptoms.
Classification of astrocytomas
In order to understand what place anaplastic astrocytoma has among other glial neoplasms of a similar type, let us outline the principles of classification of astrocytomas.
Depending on the cytological features, all astrocytomas are divided into two types:
- Common astrocytomas (fibrillary, gemistrocyte and protoplasmic).
- Special astrocytomas (subependymal, piloid and microcystic cerebellar).
According to the generally accepted and most commonly used classification (proposed by WHO), brain astrocytomas are classified according to the degree of malignancy (and each degree has its own ranking according to stages):
- Pilocytic or piloid astrocytoma of the brain. Neoplasms of this type have the first degree of malignancy (the lowest). They are characterized by slow growth, they do not degenerate into cancer, and are considered ordinary benign tumors that respond to the proposed treatment. The most characteristic clinical manifestations are hydrocephalus and problems with coordination.
- Fibrillary astrocytoma of the brain is also considered a non-aggressive common benign neoplasm, however, a tumor of this type has a second degree of malignancy. Amenable to surgical treatment.
- Anaplastic astrocytoma of the brain - refers to the third degree of malignancy. In this case, carcinogenic processes are already observed, which are difficult to remove surgically, since the tumor spreads to neighboring tissues. Anaplastic astrocytoma of the brain most often develops in people over thirty years of age.
- Glioblastoma, gliosarcoma – fourth degree of malignancy. This type of cancer is the most dangerous and aggressive, so surgical treatment is significantly complicated, and the prognosis for life will be unfavorable. Glioblastomas are most often diagnosed in people over 40 years of age.
According to the histological type and characteristics of the growth of pathogenic cells, astrocytomas are divided into:
- Neoplasia having clear contours and well isolated from other brain structures. They are characterized by nodular growth, and the formation of cysts is possible. These include piloid, subependymal giant cell astrocytoma and pleomorphic xanthoastrocytoma. Tumors are benign and in rare cases can become malignant.
- Neoplasms with diffuse growth, i.e. there are no clear outlines of the tumor focus. In this case, pathogenic tissues invade neighboring tissues and grow rapidly. Approximately 70% of benign tumors degenerate into cancer. These tumors include anaplastic astrocytoma of the brain and glioblastoma.
Note. Anaplastic astrocytoma (who grade III) and glioblastoma multiforme are aggressive forms of cancer. They make up about 50-60% of all malignant neoplasms in the central nervous system.
Symptoms of brain astrocytoma
The first clinical manifestations of the disease include a headache of a local or widespread nature, which gradually ceases to be relieved by taking painkillers. The nature of such pain can be either bursting and aching, or sudden and acute, which is associated with a sharp disruption of blood flow due to compression of the blood vessels by the tumor. Seizures are common, which is why it is important to seek medical help for children and adults who experience sudden seizures, even if they have only had one seizure. This serves as an absolute indication for a person to contact a specialized medical institution to see a neurologist or epileptologist for the purpose of further diagnosis and instrumental methods to confirm the diagnosis.
In addition to cramps and headaches, changes in the psycho-emotional background, fatigue, irritability, and impaired ability to concentrate and remember are often observed. Patients may experience nausea and vomiting of central origin, which does not bring relief. There are complaints of visual impairment on the opposite side from the formation of the tumor process, the gait becomes unstable and shaky. Such symptoms develop due to the growth of a tumor that compresses the brain, resulting in increased intracranial pressure. In some cases, a perversion of taste preferences, a desire to eat inedible objects, or a change in taste sensations may develop.
Symptoms will vary depending on the location of the astrocytoma. Therefore, a competent specialist, with the correct interpretation of the clinical picture, can determine the localization of the tumor process even before performing instrumental research methods, although, of course, their implementation remains absolutely necessary for this disease. So:
- a lesion of the frontal lobe will be characterized by a disturbance in the sphere of the emotional and psychological components, the patient’s criticism decreases, there is an unreasonably elevated mood, half of the body on the opposite side of the lesion may be immobilized;
- with the development of a tumor in the temporal lobe, symptoms such as impaired memory and speech, poor coordination of movements will be observed, very often the first symptom is convulsive episodes and auditory disorders;
- astrocytoma of the brain in the parietal lobe is accompanied by a decrease in tactile and pain sensitivity from the trunk and limbs, agnosia (impaired perception of surrounding objects), the inability to perform simple manual manipulations and a violation of written speech;
- When a tumor affects the cerebellum, the patient cannot properly coordinate his movements and, most often, is unable to maintain balance. There is pronounced unsteadiness of gait, the person cannot move without support;
- the pathological process in the occipital lobe includes visual hallucinations and decreased vision on the opposite side of the lesion.
Symptoms
The first symptoms of any brain tumor may be due to the cause of the tumor. Height can put more pressure on the brain and symptoms may include:
- vomit;
- seizures;
- headache;
- personality changes;
- problems walking;
- visual changes;
- problems with memory, thinking and concentration.
Symptoms of an astrocytoma will vary depending on the location of the tumor in the head. For example:
- frontal lobe – gradual changes in mood and personality, paralysis on one side of the body;
- temporal lobe – problems with coordination, speech and memory;
- parietal lobe – problems with sensation, writing or fine motor skills;
- cerebellum – problems with coordination and balance;
- occipital lobe – vision problems, visual hallucinations.
Pilocytic astrocytoma (grade I malignancy)
Signs: benign tumor, has clear boundaries, grows slowly. More common in children. Typical locations: cerebellum, brain stem and optic nerves. After complete removal of the tumor, complete recovery is possible.
Fibrillary astrocytoma (grade II malignancy)
Signs: the tumor grows slowly and has no clear boundaries. Occurs in patients 20-30 years old. Treatment: surgery. Relapse is possible. In case of relapse, repeated surgery and radiotherapy are performed.
Diagnosis of brain astrocytoma
Symptoms of brain astrocytoma are nonspecific, so timely diagnosis is sometimes difficult. The examination plan is prescribed by a clinical physician - a neurologist or neurosurgeon. At the Medical Center “Medicine of the Northern Capital”, experienced radiology doctors can recommend diagnostic procedures that must be performed before visiting a specialized specialist - in this case, patients come to the attending physician with ready-made instrumental examinations. The clinician must carefully collect anamnestic data, identify family history, occupational hazards and other risk factors listed above. Pays attention to complaints, their intensity and duration, all this helps to identify the reason why a person decided to go to a specialized medical institution. For diagnosis, laboratory research methods are used, such as a general blood and urine test, a biochemical blood test and an analysis for tumor markers.
After a conversation with the patient, the following instrumental research methods may be prescribed:
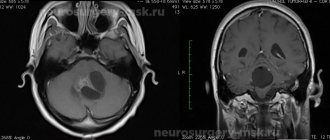
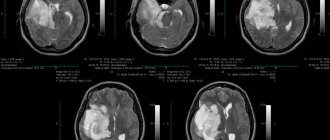
- Magnetic resonance imaging (MRI). This study is a modern diagnostic method that is highly informative and is usually used when a tumor is suspected. With astrocytoma, areas of altered brain tissue will be visible on the tomogram. The tumor can compress nearby brain structures, thereby causing their deformation or compression. To improve the effect and more accurately determine the extent of the tumor process, contrasting with drugs from the lanthanide group (gadolinium) is used, which makes it possible to differentiate glial tumors from each other. The more “malignant” the process, the more contrast agent is absorbed. If we consider the 1st degree of malignancy, then on the tomogram the tumor will appear as a round formation with regular boundaries and a clear contour. Further degrees of severity of the tumor process do not have clear boundaries, and this is manifested in the image by an increase in edema, loss of homogeneity of the tumor, in the later stages, multiple zones of necrosis and an increase in the number of hemorrhages.
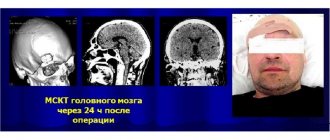
- Computed tomography (CT). This research method has the same advantages as MRI, but due to its structural features it is the subject of choice for people suffering from claustrophobia. Ideal for tumor growth in the skull bones.
- Ultrasound examination of the vessels of the head and neck (USDG BCA). Dopplerography allows you to assess the condition of blood vessels and exclude pathology of the vascular bed, and identify the severity of the disease.
- A biopsy is a mandatory component of the study, as it can reveal the heterogeneity of cellular structures and confirm the diagnosis of brain astrocytoma. The biopsy is performed in an open operating room, that is, in addition to the instruments intended for puncture, there are instruments for surgical intervention. If microscopic examination of the biopsy material confirms the presence of cancer cells, surgical intervention aimed at excision of the tumor is possible.
- Cerebrospinal fluid examination. When studying the component of the cerebrospinal fluid, an increase in the amount of protein catches the eye, b-lipoproteins appear, which should not be normal, and the total number of cells that have different composition and shape also increases. Such diagnostics are performed only in specialized medical institutions.
- Electroencephalography (EEG) has a characteristic clinical feature. At first, nerve impulses travel slowly, then there is a sharp increase in amplitude and their alternation, which makes it possible to suspect a focus of pathological activity that affects the reticular formation. The electroencephalogram of such patients consists of unevenly spaced notches with different frequencies of oscillatory movements;
- If necessary, neurologists can additionally prescribe an examination by an ophthalmologist, an otorhinolaryngologist, and certainly a neurosurgeon and an anesthesiologist. The anesthesiologist, depending on gender, age, weight and the presence of concomitant diseases, must select the correct anesthesia that would be useful during the operation.
Treatment of anaplastic astrocytoma
The effectiveness of treatment for anaplastic astrocytoma depends largely on its location and degree of pathogenesis. The main method of treatment is surgical removal of the tumor (by resection or craniotomy). Chemotherapy and radiation (radiotherapy) are required.
The choice of surgical technique for tumor removal depends on its size. For small anaplastic tumors in the early stages, it is possible to use less invasive stereotactic radiosurgical removal of the pathological focus. The operation is performed using a tomograph. However, this type of treatment is only possible for benign tumors.
Surgical treatment of astrocytomas by craniotomy is possible only for nodular types of tumor, and is not performed for diffuse type formations, because the neoplasia penetrates deeply into adjacent tissues. Therefore, subtotal removal of the tumor is performed in order to reduce the pressure inside the skull and prevent hydrocephalus.
Radiation treatment of anaplastic astrocytoma of the brain. For inoperable tumors, radiotherapy is the main type of cancer treatment; in other cases, it complements surgical treatment. Radiation stops mitoses in cells, some of them die. In parallel with this, chemotherapy is prescribed. Treatment with cytostatic drugs before and after surgery reduces the likelihood of relapses and prolongs the period of remission.
Treatment of astrocytoma
Treatment depends on the degree of malignancy of the pathological process, the characteristics of its localization and size.
Surgical intervention is prescribed to patients to excise the astrocytoma, while nearby healthy tissue is removed at the same time. This is important because the minimum number of cancer cells is enough for a relapse to occur. When removing a tumor of low differentiation and high degree of malignancy, chemotherapy or radiation therapy is added to the operation. However, operations for malignant neoplasms are more supportive in nature; as a rule, the infiltration of surrounding brain tissue is so strong that the distribution of healthy and damaged tissue is simply impossible, especially at a late stage the tumor gives metastases.
Chemo-radiation therapy is a drug or radiotherapy treatment aimed at suppressing the growth of cancer cells and destroying them. Damage to healthy tissues is often observed.
Features of the operation
Surgery is carried out after studying all possible risks and side effects, for example, if the tumor is large and grows further. But excision of the tumor is possible only if it is localized in an area accessible to the instrument and the patient’s health and age allow the procedure to be performed.
A computer or magnetic resonance imaging scanner helps to minimize risks during an intervention. To avoid relapse, healthy tissue is also excised. The manipulation is performed mainly under general anesthesia, with the exception of the location of the tumor near the speech or visual centers. Basic surgical techniques:
- removal of the tumor with an endoscope;
- open surgery.
As a rule, after traditional surgery, chemical and radiation therapy is performed.
The radiosurgery method can be used in the case of even an inoperable tumor.