Metastatic brain cancer (also known as secondary brain cancer) is the spread of cancer cells in the brain from a malignant tumor located in another part of the body. Some facts and figures:
- The secondary could occur 10 times more often than the primary, that is, the one that initially develops in the brain;
- Brain metastases occur in 20-40% of cancer patients (on average, every fourth);
- Every year, brain metastases are diagnosed in 50,000 - 70,000 Russians;
A couple of decades ago, with multiple metastases to the brain, the patient could be given up - neurosurgical institutions that were making progress in the treatment of primary brain tumors did not accept such patients, because surgical treatment in this case was already almost impossible. Even in the capital, no more than three specialists were ready to try radiation therapy, while several dissertations were defended on this topic, demonstrating very good results. But practical activities encountered clinical difficulties that made saving the patient very labor-intensive.
Metastases of malignant tumors in the brain occur in every fourth patient, and during post-mortem examination they are found in six out of ten. Metastases are detected an order of magnitude more often than primary tumors of the central nervous system, which neurosurgeons readily treat. Russian oncology statistics take into account only primary brain tumors and primary cancers in general, but do not know how many patients have metastases anywhere, and not just in the brain.
Any tumor metastasizes to the brain, but most often lung cancer, especially extremely aggressive small cell cancer - up to 80% of patients, as well as breast cancer, colon cancer, kidney cancer and melanoma, but all of them metastasize much less often than lung cancer. Today, brain metastases are found more often than at the end of the last century, which is greatly facilitated by neuroimaging methods - CT and MRI and increased survival of cancer patients as a result of advances in oncological science. The activity of oncologists has also increased noticeably, not only deciding to treat the most difficult patients, but also having the opportunity to care for such patients.
As a rule, by the time intracranial metastases are identified, most patients have other, sometimes incurable and widespread, tumor foci, their condition leaves much to be desired, and local therapy for intracranial metastases is fraught with early relapse. The introduction of high-tech treatment, both surgical and radiation, helped get rid of professional pessimism and increased the 5-year survival rate of patients, giving them a completely acceptable quality of life.
Why do brain metastases occur?
Metastasis is a rather complex process. It consists of several stages. The tumor must grow into neighboring tissues, then its cells break off and penetrate the blood or lymph vessels. Migrating with the bloodstream, cancer cells settle in different organs. They “dormant” for some time, then rapid growth begins.
Most often - in 48% of cases - brain metastases are associated with lung cancer. Non-small cell lung cancer is the most aggressive - it metastasizes to the brain in 80% of cases. Metastases are less common in breast cancer (15%), genitourinary system (11%), osteogenic sarcoma (10%), melanoma (9%), and head and neck cancer (6%).
Tumor metastases - symptoms and treatment
Tumor metastases are cancer cells that have spread throughout the body and become established in one or more internal organs. In 90% of cases, it is metastases that cause the death of a cancer patient [1][2]. Any malignant tumor can metastasize; this is one of the properties that distinguishes them from benign tumors.
It is now known that metastasis is a complex, dynamic process. It plays a role in the mutational load of the tumor (the number of mutations in the genetic code of cancer cells), the interaction between cancer and normal cells, and signaling molecules that are located in the intercellular substance (they interact with cells and control their growth and reproduction).
Probability of developing metastases
Whether metastases occur or not depends on several factors:
- Type of cancer. For example, basal cell carcinoma metastasizes extremely rapidly, and melanoma is a highly aggressive neoplasm in which metastases develop very quickly.
- Molecular genetic features of cancer. For example, triple negative breast cancer is more likely to metastasize than tumors that have estrogen receptors, progesterone receptors, or those associated with overexpression of the HER2 protein.
- The degree of malignancy of the tumor. The higher it is, the more aggressive the cancer and the higher the likelihood of it metastasizing.
- Features of localization. For example, breast cancer in the inner quadrant of the breast metastasizes more often than tumors in the lateral quadrants.
- Features of growth. Tumors with infiltrative growth metastasize more often and faster than tumors growing superficially. For example, fungal tumors of the colon and stomach are less malignant than infiltrative forms of cancer of these organs.
What affects the rate of spread of metastases?
The rate of spread of metastases also depends on the type of cancer, the degree of malignancy of the tumor and its molecular genetic characteristics. For example, high levels of TGF beta protein may increase the rate of metastasis.
However, more often in clinical practice, the rate of spread of metastases throughout the body is associated with the type of cancer and its location. For example, poorly differentiated tumors metastasize earlier than highly differentiated ones, and lung cancer, due to its good blood supply, spreads much faster than prostate cancer.
Once metastasis has occurred, it becomes very difficult to fight a malignant tumor; this is the last stage of cancer development . From this point on, treatment is palliative in nature: it helps to slow down the progression of cancer, prolong life and improve the condition, but not cure the patient [3].
Most often, malignant tumors metastasize to the bones, lungs, liver and brain. In some types of cancer, tumor cells spread along the surface of the peritoneum.
The complex chain of events, as a result of which a malignant cell breaks away from the mother tumor, migrates in the body and forms a secondary focus in another organ, is not fully understood, and work in this direction continues [1]. Some theories attempt to explain the causes of metastasis .
One of them says that due to accumulated mutations, an epithelial-mesenchymal transition : tumor cells begin to resemble those found in the body of the embryo and are involved in wound healing. They are irregular in shape, do not stay in place and can migrate in the body.
According to another theory, metastases occur from stem cells , which normally should replace cells that die as a result of damage or naturally. This theory is supported by the fact that tumor and stem cells have a number of common features in structure and biochemical processes.
It is believed that macrophages (“eater cells”), which normally should eliminate foreign particles, help spread metastases of a malignant tumor. In cancer, they support inflammation and angiogenesis (the process of forming new blood vessels). This promotes the migration of tumor cells.
In cancer patients, millions of cancer cells enter the bloodstream every day. But only a few of them can give rise to metastases. This depends on the histological type of the tumor (from which tissue it originated), the degree of aggressiveness of the tumor (stage of cancer), and cell differentiation (how much they have lost their normal features).
Clinical manifestations of metastases
Symptoms depend on the size of intracranial tumor foci, their number and location. Basically, clinical symptoms can be divided into two groups:
- local, due to the location of the tumor in a specific part of the brain responsible for certain functions of a certain organ;
- general cerebral symptoms associated with the size of additional tumor tissue interfering with the functioning of the brain itself.
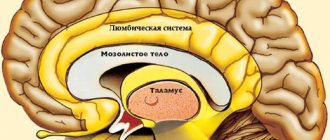
For example, a tumor near the structures that provide innervation to the eye will manifest itself as a loss of visual fields, when the eye does not perceive certain parts of the viewing sector. Many small nodes will give a picture of cerebral edema, since extra grams of tumor in a closed cranium interfere with the normal circulation of fluids and compress normal tissues.
In half of the patients, secondary brain tumors respond with headaches; very often the intensity of the pain changes along with the position of the head, when, when tilted at a certain angle, partial restoration of cerebrospinal fluid circulation temporarily leads to a decrease in pain. Unfortunately, over time, the growth of metastases will make the pain constant, and the confined space will lead to unbearable intensity. Dizziness and double vision are common when looking with both eyes.
Every fifth patient develops motor disorders up to paresis of half the body. Every sixth suffers from intellectual abilities, the same number suffers from changes in behavior, disturbances in movement and gait, seizures are slightly less common, but a completely asymptomatic course, when metastatic formations are detected only during examination, is also not uncommon. However, as the size of the tumor increases, even in such a relatively favorable situation, the functions of the body are quickly disrupted.
Swelling of the tissue around the tumor - perifocal edema, coupled with increased intracranial pressure (ICP) causes general cerebral symptoms with headache, dizziness, double vision, vomiting at the slightest movement or even when opening the eyes, constant hiccups, leading to depression of consciousness up to cerebral coma. A decrease in heart rate and breathing rate with very high “upper” systolic pressure indicates extremely high and potentially fatal intracranial pressure.
In practice, variants of the development of primary symptoms in cancer metastases to the central nervous system are distinguished according to the prevailing set of clinical signs.
- The apoplexy variant, similar to a stroke, develops acutely and is manifested by focal disorders - evidence of damage to a certain area of the brain. This option is usually associated with either blockage of the vessel or its rupture by a tumor, followed by hemorrhage into the brain.
- The relapsing-remitting variant is characterized by an undulating course, when the symptoms either decrease or progress, resembling atherosclerotic vascular damage.
In some patients, brain metastases are asymptomatic. They are discovered only during examination.
Get a treatment program
Metastases in the liver
A malignant tumor of each organ has “favorite” anatomical zones where metastatic formations most often appear, which does not exclude the development of secondary cancerous tumors in a completely atypical location. Thus, with cancer of the gastrointestinal tract, metastatic lesions of the liver are often observed, while with malignant lesions of the ovaries, liver lesions are quite rare.
Metastatic liver damage is varied in the size of the foci and their number, it is customary to distinguish:
- solitary lesion - the only one in the organ, as a rule, with cancer of low aggressiveness, it can reach quite large sizes;
- single metastasis - no more than 10 tumor foci;
- multiple lesions, often referred to as seeding, are characteristic of aggressive or advanced neoplasms.
In the liver, ultrasound reveals lesions of about a centimeter; smaller formations are not easy to see. CT or MRI are more informative - nodules of about three millimeters are visible.
If the patient has previously undergone antitumor therapy, after determining the functionality of the liver and other important organs, the diagnostic stage is considered completed and optimal therapeutic tactics are proposed.
In the absence of a history of treatment of primary cancer and the initial detection of tumor dissemination in the liver, it is impossible to speak unambiguously about the primary source. It is necessary to know the primary source of cancer cells in order to select the most effective drug treatment. To identify the type of cancer, an ultrasound-guided biopsy is performed to accurately target the node and collect material for microscopy.
Clinical manifestations depend on the volume of secondary tumor damage to the liver; tissue not involved in the process takes a long time to compensate for the cancerous damage to almost the entire lobe. Pain appears when the capsule is stretched by an enlarged liver tumor.
Even multiple metastases with the exclusion of almost all liver tissue from functioning may not manifest symptoms until the development of liver failure.
Signs of liver failure: nausea and vomiting, severe weakness and staining of the skin with bile pigments - jaundice, ascites, severe edema and deterioration of biochemical blood parameters.
Treatment is selected in accordance with the biological characteristics of the primary tumor; as a rule, chemotherapy is used at the first stage; further tactics depend on the effectiveness of the courses. In some clinical situations, local chemotherapy is possible, when a cytostatic agent is injected into the vessel feeding the tumor.
When solitary or single metastatic nodes exist in the liver for a long time, surgical removal is possible and often in combination with high-tech invasive local manipulations - radiofrequency ablation (RFA) or destruction with liquid nitrogen.
The Clinic uses all diagnostic and therapeutic methods, including innovative invasive interventions. The main advantage is the combination of high professionalism of the staff with the rare technical capabilities of the institution, optimal methods of caring for patients after treatment and individual programs to support the body in serious illness.
We will call you back, leave your phone number
Message sent!
expect a call, we will contact you shortly
How are brain metastases diagnosed?
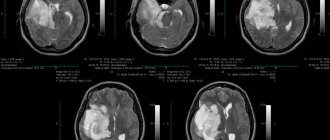
The “gold standard” in diagnosing metastatic brain cancer is magnetic resonance imaging (MRI). During this test, images of the internal structures of the body are obtained using a strong magnetic field. From the images, the doctor can judge the number, size, and location of metastatic foci.
A biopsy is a test during which a piece of tissue is removed and examined for cancer cells. If a person has already been diagnosed with cancer in another organ and lesions are found in the brain, there is usually no need for this diagnostic method. A biopsy is needed if there are lesions in the brain, but the primary tumor has not been found.
Brain cancer metastases
Secondary (metastatic) brain tumors occur 5-10 times more often than primary tumors [1]. In the USA, up to 170 thousand new cases of metastatic brain tumors are registered annually [2;3]. According to autopsy data, from 24 to 45% of all cancer patients have intracranial metastases [2;4;5]. The development of metastases, causing physical and mental disorders, leads to rapid disability of patients. Symptomatic (i.e., occurring with neurological symptoms) brain metastases (BM) occur in 8-10% of cancer patients. The incidence of GBM registration is likely to increase as overall survival of cancer patients increases due to improvements in drug treatment [6–8].
The prognosis for the life of patients with multiple brain metastases in the vast majority of cases is pessimistic and, on average, life expectancy does not exceed 8-12 months, with almost any combination of possible treatment methods [3]. Only 8% of such patients overcome the two-year survival threshold, and the 5-year survival rate is slightly higher than 2% [9]. The quality of life of patients during this entire period of time largely depends on the chosen treatment tactics.
The main localization options for primary tumors that metastasize to the brain: lung cancer, breast cancer, colon cancer, kidney cancer, skin melanoma. According to Shaw E, 1993, every third patient with lung or breast cancer, and with melanomas, 3 out of 4 patients suffer from metastatic brain damage [10]. Metastasis of cancer tumors to the brain occurs predominantly hematogenously from primary tumors or metastases in other organs and tissues. This process correlates with the volume of local blood flow: up to 80-85% of metastases occur in the cerebral hemispheres, from 10 to 15% in the cerebellum and 3-5% in the brain stem [4;11]. Macroscopically, as a rule, metastases are clearly demarcated from the medulla and have a round shape. During histomorphological examination, metastases are also usually well demarcated from the brain substance. The predominantly “mechanical” effect of metastases on brain tissue (as opposed to the diffuse growth of glioblastomas) is noted by V.N. Kornienko. (2006), based on a comparison of diffusion-weighted MRI data [12]. Siomin V. et al. (2005) note possible infiltration of adjacent tissue, especially in the case of small cell lung cancer and melanoma, or microscopic screenings of cancer cells that cannot be detected [5]. The presence of a cystic component may be due to necrosis, accumulation of altered keratin (squamous cell carcinomas) or increased mucus secretion (adenocarcinomas). Metastases of melanoma and choriocarcinoma are most prone to hemorrhages, and somewhat less often - renal cell carcinoma and bronchogenic carcinomas, but since Bronchogenic metastases are much more common and are the leading cause of hemorrhage [11].
The course of the disease in patients with GBM is, in most cases, aggressive. Almost 80% of patients have multiple (>3 lesions) GBM at the time of diagnosis, and approximately 10-15% of metastatic lesions are deep in the brain. These patients often have clinical manifestations of neurological and cognitive dysfunction, so improving the functional status and quality of life of these patients is as important as increasing overall survival (OS). The prognosis for patients with GBM remains poor: median OS does not exceed one month without treatment [13;14].
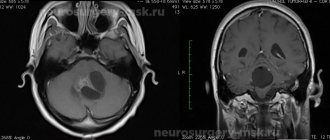
The generally accepted standard for diagnosing brain metastases is contrast-enhanced magnetic resonance imaging (MRI) . Other techniques (computed tomography, positron emission tomography) play a much smaller, usually auxiliary role
Information content of various MRI scanning modes in the diagnosis of intracerebral metastases:
Fig. 1 MRI without contrast enhancement. Picture of an apparently unchanged brain
Rice. 2 MRIs with contrast enhancement. Picture of total metastatic lesion
Symptomatic treatment. In most cases, they are malignant, incl. metastatic, tumors are accompanied by the early development of perifocal edema. Edema increases the volumetric effect of the tumor on the brain tissue, leading to its compression, focal impairment of brain function and increased intracranial pressure. Steroid hormones (Dexamethasone) help stabilize and reduce perifocal edema, which leads to a decrease or even temporary disappearance of symptoms, improving the quality of life of patients. However, it must be taken into account that steroid hormones do not affect tumor growth, and, therefore, their effect is temporary and will decrease as the pathological focus continues to grow. Steroid hormones are prescribed only by your doctor. Dosage adjustments should occur in agreement with him. In this case, you should follow a few simple but important rules:
- A single intramuscular injection of up to 8 mg of Dexamethasone is allowed
- When administering the drug two or three times, the last injection should be no later than 16-17 hours, which is most consistent with the natural rhythm of the production of steroid hormones in the body
- The use of steroid hormones must necessarily be accompanied by the use of drugs that suppress gastric secretion to prevent side effects.
Chemotherapy in this group of patients has insufficient effectiveness due to the limited penetration of most drugs through the blood-brain barrier. However, as noted by Peereboom DM (2005), chemotherapy certainly remains one of the main types of treatment for the primary site and extracranial metastases of most types of extracranial malignant tumors [15]. Thus, chemotherapy plays an important role in preventing the appearance of new metastases in the brain.
In recent years, a special direction of drug therapy has emerged and rapidly developed - targeted , the effect of which, unlike chemotherapy, is determined not by the toxic effect on pathological cells, but by the disruption of certain metabolic processes in the tumor, inactivation of specific enzymatic reactions, suppression growth of tumor vessels, etc. This direction in oncology currently occupies an increasingly important place, incl. and in the treatment of intracerebral tumors.
Surgical treatment still remains one of the main methods of treatment for patients with GBM [16;17]. Surgical treatment, as a rule, quickly reduces the clinical manifestations of mass effect and provides the opportunity to conduct histological and immunohistochemical examination of the tumor [16;18]. However, surgical treatment is not always possible, especially in patients with poor functional status (IC ≤70), with multiple metastatic lesions of the brain, or in the case of metastases located in functional areas of the brain [19;20]. Recurrence of metastases at the surgical site occurs in 10% to 50% of cases [21;22].
Whole brain irradiation (WBRT) is prescribed as a standalone treatment option, or as an adjuvant treatment after surgery or radiosurgery. Carrying out WBRT provides control of both visible GBM and micrometastases [23;24]. The latter circumstance, according to some experts, also plays a “preventive” role, although such an approach is apparently justified only for small cell lung cancer [4;25]. WBRT is most often performed in a total focal dose of 20 Gy in 5 fractions, 30 Gy in 10 or 15 fractions, and 40 Gy in 15 or 20 fractions [5]. On average, the survival of patients after WBRT alone is about four months and 6-9 months in the case of combined treatment (surgical resection and WBRT) [13;26-28].
Stereotactic radiosurgery (SRS) provides selective irradiation of small-volume intracranial pathological lesions in one treatment session while minimizing irradiation of surrounding normal brain tissue [29-31]. SRS is becoming the treatment of choice for the treatment of single and multiple GBM due to good local tumor control and low complication rates [30;32]. Radiosurgery using Gamma Knife is a well-established and widely available method for treating intracerebral metastases in developed countries. Developed in our country, this technique allows us to provide high-tech and effective care to cancer patients, helping to both increase their life expectancy and maintain its quality.
Table 1 Main morphological changes in metastases after SRS [33]
RESULTS OF STEREOTAXIC RADIOSURGICAL METASTASES USING THE GAMMA KNIFE DEVICE (SRCHN)
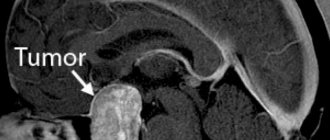
Rice. 3 Metastasis of non-small cell lung cancer in the medulla oblongata. Before SRCHN and 1 month after SRCHN
Rice. 4 Metastases of non-small cell lung cancer to the brain before SRCHN and 1 year after SRCHN
Rice. 5 Metastases of non-small cell lung cancer to the brain before SRCGN and 1 year after SRCGN
Rice. 6 Solitary metastasis of renal cell carcinoma in the chiasmatic-sellar region before SRCHN and 9 months after SRCHN This example clearly demonstrates the possibility of safe and highly effective use of SRCHN near functionally important intracranial structures (in this case, the optic nerves, chiasm and optic tracts), with rapid and obvious clinical improvement. In this case, the dose drop from 18 Gy (at the edge of the tumor) to 8 Gy (safe for the optic nerves) between the tumor and the visual pathways occurs at a distance of less than 3 mm.
This example clearly demonstrates the possibility of safe and highly effective use of SRHN near functionally important intracranial structures (in this case, the optic nerves, chiasm and optic tracts), with rapid and obvious clinical improvement. In this case, the dose drop from 18 Gy (at the edge of the tumor) to 8 Gy (safe for the optic nerves) between the tumor and the visual pathways occurs at a distance of less than 3 mm.
Is it possible to treat metastases larger than 3 cm with Gamma Knife?
Yes, you can. For this purpose the so-called Trainee radiosurgery .
The main limitation in the treatment of metastases is the size of the tumor. To obtain a convincing effect, it is advisable to use doses in the range of 18-24 Gy, but not less than 15 Gy at the tumor edge. When irradiating a tumor up to 3 cm in size, with a dose of more than 15 Gy at the edge of the tumor, on the one hand, the effectiveness decreases, and on the other, the risk of developing local radiation necrosis increases many times over. Trained radiosurgery (stage) allows irradiation of large metastases of 3-4 cm in 2-3 irradiation sessions with an interval of 2-4 weeks. At the first stage, a large tumor is irradiated with a dose lower than usually used: 10-12 Gy at the edge of the tumor. This effect in most cases leads to a short-term decrease in tumor volume within 2-4 weeks after irradiation. However, the effect of this impact will be unstable and recurrent growth will subsequently begin. In order to avoid this, a second (rarely a third) session of radiosurgery is performed, during which a larger dose of radiation can be delivered to the reduced tumor than in the first stage. This staged exposure allows for more effective and safe irradiation of large tumors and is a kind of analogue of hypofractionated (up to 5 sessions) irradiation at linear accelerators.
When is fellowship radiosurgery justified? First of all, in the presence of large metastases located in functionally important and deeply located areas of the brain, i.e. where surgical removal is extremely risky or impossible. It is also possible to conduct trained radiosurgery if there are general contraindications to surgical tumor removal, for example, with concomitant severe diseases (diabetes mellitus, coronary heart disease, etc.), or with simultaneous metastatic damage to other organs.
Fig. 7 The result of a trained radiosurgery of a large (4 cm) metastasis of renal cell carcinoma. Left: tumor in the deep parts of the left temporal lobe with growth into the temporal horn of the left lateral ventricle, with initial compression of the left cerebral peduncle. Right: 8 months after the second radiation session. Complete regression of metastasis. Large main arteries previously involved in the tumor are visible.
Is it possible to irradiate the entire brain after using a Gamma Knife?
Yes, it's possible. Although among most traditional radiologists who are not familiar with radiosurgery, there is an opinion that even a single radiosurgery procedure forever excludes the possibility of further use of whole-brain irradiation. Actually this is not true. The combination of both methods is not only possible, but in some cases it is justified. The practice of joint use has proven itself both in the form of a stereotactic radiosurgical boost technique followed by general irradiation of the head (for example, with multiple large intracerebral or their combination with metastatic lesions of the membranes), and at different stages of treatment, when patients are first identified with single or limited the number of metastases that are irradiated with radiosurgery, incl. repeated sessions of radiosurgery, but at some point (for example, when a large number of new metastases appear simultaneously), total irradiation is justified.
It is worth noting that the so-called The “preventive” effect of general brain irradiation does not make much sense, because any tumor cells (metastases) that enter the brain through the bloodstream after completing a course of such radiotherapy will also give active growth if drug therapy is not carried out (targeted, chemotherapy or immunotherapy)
Rice. 8 Combined use of stereotactic radiosurgical boost and whole brain irradiation (with an interval of 7 days) in the presence of large, closely located metastases in the cerebellar hemispheres. Left: at the time of radiosurgery. Right: 3 months after completion of treatment
Treatment of metastases
Without treatment, the life expectancy of a patient from the moment a metastatic lesion of the brain is detected hardly exceeds a month, but this is on average. Only the addition of high doses of hormones can double life expectancy and slightly improve its quality, but again only temporarily, while chemoradiotherapy can give up to six months of life.
Treatment tactics depend on several factors:
- Number, size and location of metastases;
- Possibility to remove lesions surgically;
- Sensitivity of the primary tumor to chemotherapy and radiation therapy;
- General condition of the patient;
- The presence of other metastases, the ability to fight them.
Prognostically unfavorable is the localization of the tumor in the posterior cranial fossa, inaccessible for manipulation, impaired circulation of cerebrospinal fluid and the likelihood of tumor wedging into natural cranial foramina. There is no doubt that only surgery, coupled with additional drug and radiation treatment, gives great hope. But neurosurgical intervention is possible with one or single tumor nodes, and, of course, technically accessible ones. Palliative surgery is performed when there is a threatening increase in pressure and bleeding, when the removal of even one of many nodes can radically improve the clinical picture in order to add conservative treatment in the future. There are different options for removing tumor nodes.
For types of cancer that are technically unremovable and sensitive to antitumor drugs, such as breast, small cell lung cancer and germ cell tumors of the testicle, chemotherapy is used at the first stage, which is then followed by irradiation of the entire brain. For radiosensitive tumors, treatment can begin with total brain irradiation. For tumors no larger than 3.5 cm and less than four nodes, stereotactic radiosurgery is effective as the only method. Several beams of radio waves are applied to the tumor from different sides; they intersect in one place - where the metastasis is located. As a result, cancer cells are destroyed, and surrounding healthy tissues receive the minimum safe dose. In combination with brain irradiation and chemotherapy, the result is better.
Radiation therapy is always accompanied by an increase in swelling of the brain tissue, so irradiation is always carried out against the background of dehydration - symptomatic therapy that relieves excess fluid. Therefore, the radiologist may refuse treatment to a patient who is resistant to diuretics, as well as with an already displaced brain, since further displacement can be fatal for the patient. They will not accept irradiation for a seriously ill patient with severe clinical manifestations, especially with convulsions or cloudy consciousness. After just one or two sessions of irradiation, the existing high intracranial pressure will be joined by radiation-induced tissue edema, and the patient’s already very unimportant condition will worsen.
Contact your doctor
Variants of sequences and combinations of methods are possible, both for newly detected brain metastases and for relapse after treatment. In any case, if active tactics are impossible and the process progresses, clinical guidelines recommend resorting to chemotherapy along with the best supportive symptomatic therapy (steroids, painkillers, anticonvulsants, etc.). The regimen is determined by the primary tumor, that is, some drugs help with lung cancer, and others with kidney cancer. Chemotherapy is carried out until signs of tumor progression are detected.
Treatment of metastases of malignant tumors in the brain is not the work of single enthusiasts, it is the work of a team of oncologists, neurosurgeons, radiologists, chemotherapists and resuscitators, armed with knowledge and excellent equipment for diagnosis and treatment, as in Euroonco clinics.
Metastatic brain tumors
Patients are prescribed anticonvulsants, steroids, painkillers and psychotropic drugs. The main treatment method for metastatic brain tumors is usually radiotherapy, which is used alone, in combination with chemotherapy or surgery. The indication for surgical treatment is the presence of an operable solitary metastasis (a secondary lesion with an undetectable primary process) or a single metastasis with a controlled primary tumor.
Typically, operations are performed for metastatic brain tumors located in the cerebellum, temporal and frontal lobes, that is, in areas with a relatively low surgical risk. After surgery, radiotherapy or chemotherapy is prescribed. Sometimes the goal of surgical treatment is not to remove a metastatic brain tumor, but to urgently reduce life-threatening intracranial pressure. If necessary, such interventions can be carried out repeatedly.
Chemotherapy is usually ineffective. The exception is situations when the primary tumor responds well to cytostatics, for example, in breast cancer, small cell lung cancer or lymphoma. Patients with metastatic brain tumors that are sensitive to chemotherapy are prescribed drugs that can cross the blood-brain barrier. Chemotherapy must be supplemented with other treatment methods (usually radiotherapy).
A promising modern method for treating metastatic brain tumors is 3D conformal radiation therapy - irradiation with thin beams of radiation aimed at the tumor. This technique allows for maximum impact on the tumor with minimal radiation exposure to healthy tissue. The procedure is carried out under MRI or CT control. The method has a number of advantages over traditional operations (painlessness, non-invasiveness, absence of anesthesia and postoperative period). Indicated for multiple metastatic brain tumors and high surgical risk due to the location of the metastasis.
For secondary lesions in the spinal cord, the same methods are used as for brain damage. The use of corticosteroids can reduce pain in 85% of patients, and radiotherapy in 70% of patients. Half of the patients experience improvement in motor functions during radiotherapy. Surgical interventions are performed when metastatic brain tumors are insensitive to radiotherapy, when neurological disorders progress, or when nerve tissue is compressed by a bone fragment. Anterior decompression or laminectomy is performed. After surgery, local radiotherapy is prescribed (with the exception of tumors that are insensitive to radiation therapy).
What is the prognosis for brain metastases?
The prognosis depends on the type of primary tumor, the number of metastases, the age and condition of the patient. On average, patients live 2-3 months. But if there are single metastases, the patient is under 65 years old, and there are no other metastases in the body, the average life expectancy can be 13.5 months.
Oncologists and resuscitators at Euroonco know how to help a patient with metastatic cancer. Competent treatment will relieve severe symptoms and give you valuable time.
| More information about treatment at Euroonco: | |
| Oncologist consultation | from 5100 rub. |
| Emergency oncology care | from 11000 rub. |
| Chemotherapy appointment | 6900 rub. |
| Palliative care in Moscow | from 40200 per day |
Book a consultation 24 hours a day
+7+7+78
To which organs does breast cancer metastasize?
Most often, breast cancer spreads to the bones, lungs, liver, brain, and lymph nodes. Secondary lesions in other organs are less common.
Treatment of bone metastases in breast cancer
Metastases in the bones manifest themselves in the form of pain and swelling. The tumor destroys bone tissue, which threatens pathological fractures - they arise from a small mechanical load. In order to strengthen bone tissue, treatment for breast cancer metastases to the bones includes the use of a special group of drugs - bisphosphonates. In pathological fractures, bones are strengthened with screws, plates and other structures.
Treatment of lung metastases in breast cancer
With metastases in the lungs, the patient is bothered by a persistent chronic cough and chest pain. The sputum that comes out during a cough may contain blood. For single secondary lesions, surgical treatment of lung metastases from breast cancer can be performed.
Brain metastases in breast cancer
Metastases in the brain from breast cancer lead to headaches, which become more severe, persistent, and painful over time. Other possible symptoms: convulsions, blurred vision, nausea and vomiting, changes in personality and behavior.
Liver metastases in breast cancer
Secondary lesions in the liver disrupt its functioning and the outflow of bile. Jaundice, skin itching, abdominal pain, digestive and bowel problems occur. The biochemical blood test showed elevated levels of liver enzymes. Ascites, an accumulation of fluid in the abdominal cavity, may develop. Treatment of liver metastases from breast cancer may include methods such as:
- Radiofrequency ablation: a needle-shaped electrode is inserted into the tumor site and a high-frequency current is applied to it. Intra-arterial chemotherapy is the administration of chemotherapy drugs into the hepatic artery. Chemoembolization is the introduction of a chemotherapy drug into the vessel feeding the tumor in combination with emboli - particles that block the blood flow. Laparocentesis is puncture and removal of fluid from the abdominal cavity in case of ascites. Sometimes surgical treatment is indicated.
Metastases in lymph nodes in breast cancer
Most often, with breast cancer, metastases are found in the axillary lymph nodes. At the same time, the lymph nodes enlarge and become noticeable, they can be felt. Swelling and swelling occurs in the arm (lymphedema). If the cancer has spread to nearby (regional) lymph nodes, it can often still be treated with surgery.
Metastases of breast cancer in the thyroid gland
Metastasis of breast cancer to the thyroid gland is rare. In this case, the prognosis becomes much worse. Sometimes removal of the thyroid gland (thyroidectomy) is indicated to prevent and control complications.