Why is diabetes dangerous?
The content of the article
Patients with type 2 diabetes have a 2- to 4-fold increased risk of coronary heart disease (CHD), peripheral vascular disease, retinopathy, nephropathy, and neuropathy.
The main risk factors for diabetes are obesity, low physical activity, old age and heredity. The exact causes of diabetes are not yet completely clear. However, already in the 17th century it was believed that emotional stress could influence the development of this disorder.
More than 400 years ago, the famous English physician Thomas Willis (1621–1675) noticed that diabetes develops in people who have experienced prolonged stress, sadness, or have been involved in prolonged scandals. He argued that "nervous fluid" is important for the development of CD.
In the 19th century, William Osler repeated the same claim. And later, doctors recognized stress as a risk factor for developing diseases. Finally, science has shown that stress can both trigger diabetes and worsen its control. Epidemiological studies have shown an association between chronic emotional stress and the development of CD.
New prospective epidemiological studies clearly show that emotional stress, anxiety, anger, poor sleep and hostility increase the risk of developing type 2 diabetes.
Emotional stress
What are the dangers of neurological complications of diabetes?
Class Clinic
In terms of prevalence, diabetes mellitus is the leading endocrine disease in the world. According to the Russian Diabetes Association, in 2021 there were about 415 million diabetics in the world.
Diabetes mellitus is dangerous because it is accompanied by a violation of all types of metabolism: carbohydrate, fat, protein, mineral, water-salt. Such serious metabolic disorders naturally lead to serious complications, including from the nervous system. Neurologist at the Kaliningrad medical center Class Clinic Anna Valerievna Penkova spoke in detail about the neurological complications of diabetes mellitus.
What neurological complications can diabetes cause and how do they manifest?
The key point in the development of diabetes complications, including neurological ones, is a persistent increase in blood glucose, which leads to damage to the vascular wall. In this case, both large vessels and capillaries are affected. The most developed capillary network in our body is located in the kidneys, eyes, brain, and also in the limbs. These organs are the targets of diabetes.
When large and small vessels are affected, this causes an increase in their permeability and fragility of the vessels occurs. Phenomena such as thrombosis and atherosclerosis easily develop. The result of such vascular disorders of the nervous system is strokes, as well as chronic brain damage - diabetic encephalopathy. It is important to note that with the development of diabetes, the likelihood of strokes and other life-threatening conditions increases many times over.
Another dangerous condition among the neurological complications of diabetes is diabetic polyneuropathy. This disease occurs as a result of insufficient blood supply to the small peripheral nerves in the lower and upper extremities. Nerves experience oxygen starvation, which leads to disruption of their functions. Chilliness, tingling, numbness, a feeling of “crawling ants” in the hands, face, and feet begin. A characteristic sign is when a person walks barefoot on the floor and does not feel where he is stepping. There may also be a reverse effect when increased sensitivity develops, burning or pain occurs. Cramps may appear in the legs and calf muscles, and some patients wake up from cramps at night.
Quite often, with diabetes mellitus, individual large nerves are damaged in the form of mononeuropaity - neuropathy of the facial nerve (accompanied by paralysis of the facial muscles), trigeminal neuralgia (characterized by intense shooting pains in the face), neuralgia of the occipital nerves (shooting pains and numbness in the occipital region), neuropathy ulnar, radial, median nerves of the upper extremities with weakness and numbness in the fingers of one hand), etc.
How is diabetic polyneuropathy treated?
This is a case where we can improve the condition and eliminate the symptoms, but we cannot guarantee that they will not return, since the condition is a consequence of diabetes. Achieving long-term remission is quite difficult, but there are modern methods that can significantly improve the quality of life. The exact treatment regimen in such cases is prescribed by an endocrinologist and a neurologist, taking into account all the features of the disease.
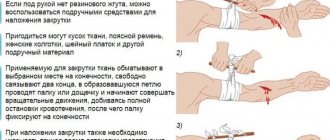
It is important to note that it is necessary to treat this condition even with minor manifestations in order to improve tissue nutrition and slow down the process of nerve damage as much as possible. With the development of diabetes and the absence of adequate treatment, tissue nutrition is disrupted so much that it leads to the immediate addition of a secondary infection, the development of non-healing trophic ulcers, and serious consequences even after minor scratches and abrasions. The appearance of gangrenous lesions in diabetes often leads to amputation of limbs.
What is important to remember about diabetes symptoms?
Unfortunately, people rarely pay attention to changes in their body, and situations often occur when a neurologist makes a diagnosis of diabetes mellitus. A typical case is when a patient consults a neurologist about chilliness in the legs and, based on the results of studies, he is diagnosed with diabetes mellitus. And then the patient remembers that he has had dry mouth, chilliness and high fatigue for a long time.
In case of any changes in the sensitivity of the limbs, chilliness, or convulsions, it is better to play it safe and consult a specialist, first of all, a neurologist. The earliest symptoms of diabetes are thirst and dry mouth, increased urine output, and increased appetite. The combination of these three symptoms alone should alert you. The appearance of neurological signs (numbness, convulsions, chilliness, etc.) against this background is a serious reason to contact a neurologist and endocrinologist.
In severe cases, in the later stages of diabetes, changes in tissue nutrition and metabolism can become irreversible. It is important to understand: the earlier treatment for diabetic complications is started, the more effective it will be.
We have developed a complex of physiotherapeutic procedures in combination with drug therapy to prevent the development of complications of diabetes mellitus and to treat existing neurological complications.
Make an appointment with Anna Valerievna Penkova on the website or by calling (4012) 777-800. When you register on the website, there is a 20% discount on your initial appointment.
Evidence for a link between stress and diabetes: experimental studies in humans
Despite the large body of evidence on the effects of psychosocial stress on blood glucose regulation in patients with diabetes, very few studies have been conducted in individuals without diabetes to determine the effect of psychoneuroendocrine activation on glucose metabolism.
One such study was conducted on 15 overweight refugees from Bosnia who were diagnosed with post-traumatic stress disorder. In all subjects, acute psychological stress resulted in postprandial glycemic peaks, selective reductions in systemic immune markers, decreased pre-inflammatory regulation of NF-κB, and increases in insulin levels associated with type 2 diabetes.
Stress-induced hyperglycemia has been found to be common in patients admitted to intensive care units, even when glucose homeostasis was previously normal. This is an excellent example of a “natural” experiment that clearly shows how acute psychological stress can disrupt glucose metabolism.
Diagram of glucose metabolism
What are the symptoms of diabetes?
One of the first symptoms of diabetes is frequent urination
. Due to the fact that the child begins to go to the toilet frequently, gets up at night, becomes thirsty, and begins to drink more liquid. Parents usually notice that the child begins to drink a lot of water. Due to the fact that the sick child drinks and eats a lot, he begins to lose weight. Next, weakness and fatigue appear.
How is diagnosis carried out? Childhood diabetes is fairly easy to diagnose. We measure blood and urine glucose levels, as well as ketone levels.
Epidemiological studies
Unlike experimental studies, epidemiological observational studies are based on data from individual surveys and questionnaires. They assess a variety of psychosocial stressors experienced, including major life events, financial or work insecurity, social isolation, and psychological stress at work.
This makes it possible to assess the effects of long-term stress. Some studies use objective methods to measure/assess stress.
One of the latest meta-analyses, including 8 studies involving more than 47,000 patients, clearly showed that work stress increases the risk of diabetes regardless of other factors such as age, gender, smoking, alcohol consumption, physical activity, and obesity.
Interesting results were obtained when analyzing data from the Whitehall II study. Psychosocial stress at work was found to increase the risk of developing type 2 diabetes in women, but did not increase the risk in men. It is important to note that in women, these side effects are exacerbated by obesity.
This association between gender, stress and type 2 diabetes was observed in 4 other studies conducted in Canada, Serbia, Sweden and Australia.
Acute and chronic stress in modern society
In modern society, people live in an environment where (probably for the first time in human history) the system described above has become harmful instead of providing protection. The physical and social environment, especially over the last 200 years, has changed beyond recognition. But the biology of modern man has remained essentially the same as that of primitive people.
In modern society, physical threats are much less common, but social life often produces psychological and social upheavals that allow the activation of frequent or persistent fight-or-flight responses.
Because psychological stress is deeply ingrained in modern society, it is often referred to as psychosocial stress, and the conditions and events that can cause it are called psychosocial stressors.
Psychosocial stressors can be divided into direct and indirect depending on the impact on the human body.
- Direct include mechanisms by which psychosocial stressors themselves lead to pathophysiological changes. The term psychoneuroendocrine activation is used to describe this process.
- Indirect include the mechanisms by which psychosocial stress influences behavior - eating habits, physical activity, smoking and alcohol consumption, which ultimately affects the development of type 2 diabetes.
An indirect effect of stress is emotional eating.
Treatment of diabetes
Before starting treatment, it is necessary to conduct an accurate diagnosis of the body, because a positive prognosis for recovery depends on this.
Treatment of diabetes is aimed at:
- decreased blood sugar levels;
- normalization of metabolism;
- preventing the development of diabetes complications.
Further, treatment varies depending on the type of diabetes. Let's look at them separately.
Treatment of type 1 diabetes (insulin dependent)
As we already mentioned in the middle of the article, in the “Classification of Diabetes Mellitus” section, patients with type 1 diabetes constantly need insulin injections, since the body cannot produce this hormone itself in sufficient quantities. There are currently no other methods of delivering insulin to the body other than injections. Insulin-based tablets will not help with type 1 diabetes.
In addition to insulin injections, treatment for type 1 diabetes includes:
- diet;
- performing dosed individual physical activity (DIPE).
Treatment of type 2 diabetes (non-insulin dependent)
Type 2 diabetes is treated by following a diet and, if necessary, taking antihyperglycemic drugs, which are available in tablet form.
Diet for type 2 diabetes mellitus is the main method of treatment due to the fact that this type of diabetes develops due to improper nutrition of a person. With improper nutrition, all types of metabolism are disrupted, therefore, by changing their diet, a diabetic in many cases gets better.
In some cases, with persistent types of type 2 diabetes, the doctor may prescribe insulin injections.
Diet for diabetes
When treating any type of diabetes, diet therapy is a must.
A nutritionist for diabetes mellitus, after receiving tests, taking into account age, body weight, gender, lifestyle, outlines an individual nutrition program. When dieting, the patient must calculate the amount of calories, proteins, fats, carbohydrates, vitamins and microelements consumed. The menu must be followed strictly as prescribed, which minimizes the risk of developing complications of this disease. Moreover, by following a diet for diabetes, it is possible to defeat this disease without additional medications.
The general emphasis of diet therapy for diabetes is on eating food with minimal or no content of easily digestible carbohydrates, as well as fats, which are easily converted into carbohydrate compounds.
What is emotional eating and how to deal with it
Emotional eating is generally defined as eating in response to emotions. Research shows that emotional eating is usually associated with anxiety, tension, fatigue, sadness, loneliness and stress. People consider stress, tension and the desire to relax as the most common causes of emotional eating. Stress can change the need to eat in two ways:
- It is believed that the occurrence of undereating or overeating is influenced by the intensity of stress.
- Chronic stress is associated with an increased desire to consume high-calorie foods, that is, foods high in fat and sugar. In this case, after eating the patient usually feels better.
Dissatisfaction with basic needs can also be a cause of emotional eating.
Dieting and calorie restriction causes chronic psychological stress, increases cortisol levels in the blood and is a common cause of emotional overeating. Dieters are more likely to experience intense cravings for certain foods that are difficult to resist than those who do not diet.
Eating without feeling hungry and reacting to emotions consumes many extra calories, which leads to weight gain. Stress-induced nutrition is one of the factors contributing to the development of obesity. During emotional eating, people consume varying amounts of additional calories, ranging from negligible amounts to hundreds of thousands during an attack. Normal overeating involves an increase of 1,000–2,000 kcal, but 20% of people consume up to 5,000 kcal per meal, 10% – up to 6,000 kcal.
Binge eating
The American Psychiatric Association has developed the following definition of a binge eating episode. It has 2 characteristics:
- Eating an amount of food that clearly exceeds what most people would eat in a similar period and under similar circumstances over a specified period of time (for example, 2 hours).
- Loss of control while eating. If a small amount of food is eaten during an attack, but the patient feels a loss of control while eating, this is called subjective overeating.
Emotional overeating is treated comprehensively: psychotherapy changes the personal reaction to stress, teaches methods of stress reduction, eating with a feeling of hunger and satiety, that is, intuitive eating, and ways to not eat in the absence of physiological hunger.
If the patient cannot resist and control the condition, the endocrinologist prescribes drugs that control the feeling of hunger, for example, reduxin. Reduxin is a very effective and strictly prescription drug.
Diagnosis of diabetes
Early diagnosis can be made using relatively inexpensive blood glucose testing.
- Analysis for glycated hemoglobin (HbA1c). Measures your average blood sugar levels over the past 2-3 months. The analysis does not require preparation.
- Analysis of fasting plasma glucose levels. Checks fasting glucose levels. The analysis is usually scheduled for the morning, on an empty stomach.
- Oral glucose tolerance test (OGTT). Tests your body's response to a sugar load. To perform this test, you need to drink a glucose solution. Blood sugar levels are measured before and after drinking the solution.
- Anytime plasma glucose (APG) measurement. Checks blood sugar levels at a certain point in time, at any time of the day, without prior preparation for the test. Your doctor may order this test if you have obvious symptoms of diabetes, such as unexpected weight loss, extreme fatigue, and/or others.
Direct effects of stress
Activation of the sympathetic-adrenal system ultimately leads to the development of arterial hypertension. In addition, elevated cortisol levels can interfere with normal glycemic control by impairing insulin secretion and reducing insulin sensitivity, and elevated adrenaline levels promote hepatic glucose uptake.
Thus, hypertensive patients who are overweight and often under stress should be considered potential diabetics and this should be taken into account when choosing individual treatment.
Different classes of antihypertensive drugs have different effects on tissue insulin resistance:
- Insulin resistance is enhanced by diuretics (with the exception of indapamide) and beta-blockers (with the exception of vasodilators).
- Calcium channel blockers and angiotensin receptor blockers do not affect tissue insulin resistance.
- Tissue insulin resistance is reduced by angiotensin-converting enzyme inhibitors (ACE inhibitors) and imidazoline receptor agonists.
Imidazoline receptor agonists are effective in controlling blood pressure and have beneficial metabolic effects by reducing sympathetic nervous system hyperactivity. Several imidazoline 1 receptor agonists have been registered in Europe. The high selectivity of drugs for imidazoline 1 receptors results in more pronounced hypotensive activity and better tolerability of treatment. This avoids side effects such as drowsiness or dry mouth, which are common with older drugs in this class, and can therefore be used in patients of working age.
A recent study showed that modern drugs increase adiponectin levels. Adiponectin is a hormone secreted by adipocytes. Low concentrations of adiponectin have been shown to be associated with an increased risk of developing diabetes mellitus and heart failure. The level of adiponectin decreases with increasing obesity, development of metabolic syndrome, and diabetes mellitus.
New studies have shown that concomitant use of modern imidazoline 1 receptor agonists with other antihypertensive drugs not only effectively controls arterial blood pressure and reduces its variability, but also reduces insulin resistance.
Thus, these are suitable drugs for the treatment of hypertension in overweight patients, especially those who frequently experience stress.
For example, Tenaxum, approved in Europe, clinically significantly reduces heart rate - HR is now identified as a new and important prognostic risk factor in patients with arterial hypertension, and does not reduce the mechanisms of adaptation of the heart to stress, i.e. remains close to physiological adaptation (patients do not feel weak).
The drug Tenaxum
Rilmenidine improves lipid and glycemic parameters and is effective in reducing arterial hypertension in postmenopausal women with excess body weight and sympathetic hyperactivity predominant in the pathogenesis of arterial hyperactivity due to newly emerging hormonal changes with age.
Anxiety disorders in patients with diabetes mellitus
Anxiety disorders are widespread in patients with diabetes mellitus (DM), especially in patients with type 2 DM. Anxiety disorders significantly worsen disease compensation. Consequently, the risk of developing diabetic complications increases and the quality of life of patients decreases. In this regard, timely identification of anxiety disorders in this group of patients is necessary. Treatment of anxiety disorders in patients with diabetes is challenging due to numerous concomitant somatic diseases. Tofisopam (Grandaxin®) is an effective and safe drug for the treatment of anxiety disorders in such patients.
Table. Efficacy of Grandaxin and Atarax in the treatment of TR in patients with diabetes, M ± m
Diabetes mellitus (DM) is a chronic disease characterized by metabolic disorders and persistent pathological hyperglycemia. It ranks fifth among diseases in terms of prevalence and sixth among causes of death in the elderly.
The chronic course of diabetes, the nature of complications, and the need for frequent self-monitoring of glycemia using an invasive method lead to an increased risk of developing mental disorders, especially anxiety and depressive states. It should be noted that in patients with diabetes, anxiety disorders (AD) are often combined with depression. And while much attention is currently paid to the study of the development of depression in this group of patients, the relationship between TD and diabetes remains poorly understood. However, TD in patients with diabetes is observed no less frequently than depression. Thus, the results of a study conducted by E.G. Starostina et al. showed that in patients with diabetes, the frequency of TR is comparable to the frequency of depression – 39.5 versus 40.0% [1].
The incidence of TR in patients with diabetes is higher than that in patients with other chronic somatic diseases. Particularly significant are types of TD such as phobias, panic disorder, generalized anxiety disorder (GAD), and organic anxiety disorder (OTD).
Traditionally, pathological anxiety is considered as a patient’s reaction to the presence of diabetes. The role of TR in the development of diabetes has not yet been studied.
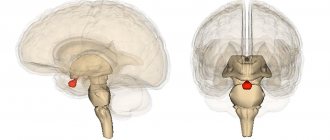
According to the existing theory, the biochemical and pathogenetic connection between TR and diabetes is explained by dysfunction of the hypothalamic-pituitary-adrenal axis in response to chronic stress. One of the neuroendocrine manifestations of psychoemotional stress is the secretion of corticosteroid hormones by the hypothalamus, followed by activation of the adrenal glands and an increase in their production of glucocorticosteroids.
Chronic stress can lead not only to adrenal fatigue, but also to disruption of the negative feedback mechanisms of cortisol secretion. The latter is often observed in endocrine pathologies: obesity, impaired glucose tolerance, as well as in some mental disorders - depression, TR. Chronic hypercortisolism contributes to an increase in visceral fat, disruption of carbohydrate and lipid metabolism. The connection between chronic anxiety and hypersecretion of cortisol was revealed using the dexamethasone test [2].
The association of TR with diabetes and obesity has been demonstrated in a number of studies. Thus, in a screening study by AN Niles et al. in a study of 42,249 patients, it was found that TP significantly increased the risk of developing diabetes (relative risk (RR) 1.3) and obesity (RR 1.2) [3]. In a large population-based study, IC Chien et al. the frequency of diabetes in patients with TR was significantly higher than in the general population - 11.89 versus 5.92%, respectively. The prevalence of diabetes in the group of patients with TR was also higher than in the group of patients without TR – 2.25 versus 1.11%, respectively [4].
Epidemiology of anxiety disorders
Symptoms of pathological anxiety in patients with diabetes, according to the literature, are observed in 40.0% of cases. At the same time, GAD - in 14.0% of cases, subsyndromal anxiety - in 27.0%, which is six to seven times more than in the population.
For patients with type 2 diabetes, constant forms of anxiety are more typical - GAD, OTR and subsyndromal; for patients with type 1 diabetes - paroxysmal anxiety in the form of phobia of hypoglycemia and injections [5].
GAD is associated with increased nonspecific inflammatory response, obesity, and arterial hypertension, factors that significantly contribute to the development of diabetes. In addition, GAD can cause an unhealthy lifestyle - lack of physical activity, overeating, smoking, which also contributes to the development of type 2 diabetes.
A study by SS Deschênes et al. demonstrated that GAD occurs in 60% of patients with type 1 diabetes. Diabetes increases the risk of developing GAD or increases the symptoms of an anxiety disorder. When GAD is combined with depression, the risk of developing type 2 diabetes doubles (RR 1.99 with 95% confidence interval (CI) (1.22–3.25), p = 0.006). The relationship between isolated GAD and diabetes has not been identified. These results were obtained through statistical analysis taking into account socio-demographic factors, as well as factors related to health status (smoking, alcohol consumption, body mass index (BMI)) [6].
E.G. Starostina et al. when examining 228 patients with type 1 and type 2 diabetes, TR was detected in 39.5% of cases, 15.0% of which were GAD. Anxiety disorders were more common among patients with type 2 diabetes (60.0 vs. 35.0%). In patients with type 2 diabetes more often than in patients with type 1 diabetes, persistent anxiety disorders were detected: generalized (22.4 versus 9.3%) and organic (18.0 versus 0%). However, pathological phobias of hypoglycemia and insulin injections were recorded eight times more often in patients with type 1 diabetes – 14.8 versus 1.7%. It is important to note that in this study, the diagnosis of “anxiety disorder” was made based on the results of not only psychometric scales, but also consultation with a psychiatrist [2]. In another study by the same author, during which 200 people (48 men and 152 women) with diabetes were examined (type 1 diabetes - 61 patients, type 2 diabetes - 139 patients), “pure” TR was studied in patients with diabetes. The effect of TR on the course of DM was assessed by comparing data from 87 patients with DM and TR and data from 46 patients with DM but without TR. Anxiety disorders were identified in 44% of participants. Moreover, in patients with type 1 diabetes they were recorded less frequently than in patients with type 2 diabetes – 26.2 and 51.2% of cases, respectively [5].
In a screening study by LT Wu et al. anxiety disorders were found in 14% of patients with type 2 diabetes. In persons without diabetes, their frequency was 7.5%. Using logistic regression analysis, it was demonstrated that the presence of type 2 diabetes increases the likelihood of developing TD, as well as other mental disorders [7].
The relationship between TR and diabetes differs between men and women. Thus, R. Demmer et al. found that the cumulative incidence of diabetes over 17 years of observation was 11.0% in men and 8.0% in women (p
In another screening study, N. Sun et al. The prevalence of TR among patients with type 2 diabetes was 43.6%. Moreover, it was higher among women than among men [9].
The relationship between TD and diabetes was also assessed in a longitudinal study by S. Hasan et al. The observation period is 27 years. The number of participants was 3489. The authors showed that diabetes only increases the risk of post-traumatic stress disorder throughout life. Women with diabetes had a longer duration of TR compared to women without diabetes [10].
The influence of anxiety disorders on the course of diabetes mellitus and the development of complications
Anxiety disorders in patients with diabetes primarily lead to deterioration in compliance with treatment and adherence to dietary recommendations. Thus, L. Gentil et al. found that TR in combination with depression is accompanied by a significant deterioration in compliance with oral glucose-lowering drugs [11]. If a patient has a phobia of insulin, he stubbornly refuses such therapy. With hypoglycemia phobia, the patient tries to maintain a higher level of glucose in the blood. E.G. Starostina et al. showed that patients with hypoglycemia phobia had an average glycated hemoglobin (HbA1c) level 1.3% higher than patients without the phobia. This difference is clinically significant with respect to the risk of developing complications of diabetes [2].
Anxiety disorders are associated with overeating. Patients with diabetes and TR have a significantly higher BMI than patients with diabetes but without TR [6, 8].
Patients with TR are also more likely to smoke and other bad habits.
In a study by N. Sun et al. It was noted that the combination of TD with depression leads to unsatisfactory glycemic control in patients with diabetes [9].
TR are an independent risk factor for the development of cardiovascular diseases and their adverse outcomes. In particular, in the work of M. Tsai et al. involving 40,896 patients with diabetes, an association of TR with an increased risk of stroke was demonstrated [12].
Results of the study by E.G. Starostina et al. indicate that patients with diabetes and TR have higher HbA1c levels than patients with diabetes without TR. For patients with type 1 diabetes, the difference was 0.9%, for patients with type 2 diabetes – 0.5% [2]. In the presence of diabetes and TR, higher values of both systolic blood pressure (SBP) and diastolic blood pressure (DBP) were recorded, the frequency of arterial hypertension was 85.0 versus 46.0% of cases, respectively (p
In addition to the negative impact on the course of diabetes, TRs significantly worsen the quality of life of patients.
Diagnostics
Timely detection of TR is a difficult task, since there are a number of somatic symptoms that are similar to those of diabetic autonomic and distal neuropathy, micro- and macroangiopathies. TD can be identified in patients with diabetes using psychometric scales - the Hospital Anxiety and Depression Scale (HADS), the Spielberg-Hanin scale. These diagnostic methods are available to both endocrinologists and primary care specialists.
The International Group for the Development of Recommendations on GAD suggests that general practitioners ask two questions to screen for the disease:
- whether you have felt restless, tense or anxious most of the time in the last four weeks;
- Do you often experience tension, irritability and sleep disturbances?
If an affirmative answer is received to at least one of the questions, it is necessary to ask additional questions to identify TR [13].
Risk groups for developing TR include patients with severe diabetes. TR should be suspected in patients with labile diabetes, difficult to control glycemia, poor compliance with treatment and non-compliance with recommendations for lifestyle changes. Patients with chronic pain due to diabetic neuropathy are a particular risk group. Patients who experience significant weight gain should also be evaluated for the presence of TR.
Symptoms of TR can be constant or paroxysmal.
Anxiety can be associated with situations that pose no real danger. Characterized by anxiety, fears, and a tendency to make negative forecasts. There is often causeless anxiety.
Patients look tense, restless, and fussy. They tend to constantly adjust their clothes or hair. Patients are unable to completely relax, muscle tone is increased. Patients with TD often replay past and expected events in their heads, which may result in sleep disturbances, difficulty concentrating, and memory impairment. Such patients are characterized by general weakness and increased fatigue.
However, general weakness in patients with diabetes may be associated with both the presence of TR and long-term decompensation of diabetes. The latter condition can be excluded by laboratory testing.
Autonomic symptoms of anxiety include increased heart rate, blood pressure fluctuations, headaches, nausea, diarrhea, increased urination, and pale or red skin.
Autonomic symptoms of TR must be differentiated from complications of diabetes, such as autonomic diabetic neuropathy. Special diagnostic tests can help identify diabetic complications.
Paroxysmal anxiety occurs as a panic attack - attacks of pronounced anxiety or fear with a variety of vegetative manifestations (rapid heartbeat, sweating, feeling of suffocation, nausea). There is often a fear of death, a fear of going crazy. Paroxysmal anxiety (panic disorders) should be differentiated from hypoglycemia. The only reliable confirmation of the latter is considered to be a blood glucose level below 3.3 mmol/l, determined using a glucometer.
If the patient suffers from cardiovascular diseases, panic attacks should also be differentiated from attacks of angina pectoris and heart rhythm disturbances.
Treatment
For TD, both medication and psychotherapy (mainly cognitive-behavioral and relaxation techniques) are indicated.
Unfortunately, today high-quality psychotherapeutic care is not available to the majority of the population, so pharmacotherapy is of particular importance.
Among patients with diabetes and TR (n = 90) examined by E.G. Starostina et al., the majority took anti-anxiety medications prescribed by therapists, neurologists, or independently. At the same time, their doses were insufficient, the courses of treatment were short or, on the contrary, very long. The drugs turned out to be ineffective (herbal remedies) or had a high potential for dependence and other side effects (phenobarbital in Corvalol and analogues, benzodiazepines) [2]. In another study, E.G. Starostina et al. of 87 patients with TR and diabetes, only 8.0% had previously consulted a psychiatrist and neurologist. 59.8% of patients with TR had previously taken psychotropic drugs, and in 82.7% of cases independently, without consulting a psychiatrist or neurologist. In the vast majority of cases, these were drugs containing phenobarbital and benzodiazepines [5].
Today, antidepressants, antipsychotics and anxiolytics are used for TR. From the first group of drugs, selective serotonin reuptake inhibitors (SSRIs) and tricyclics (TCs) can be used. It is necessary to prescribe TC to patients with diabetes with caution due to the risk of weight gain and worsening of the glycemic profile during such therapy. In addition, these drugs have pronounced cholinergic and adrenergic side effects, which limits their use in patients with concomitant somatic diseases. A relative disadvantage of SSRIs is considered to be an increase in individual symptoms of TR in the early stages of treatment and a delayed anti-anxiety effect. Adverse reactions of SSRIs include nausea, increased appetite, and sexual dysfunction. The use of antipsychotics in patients with diabetes also has a number of limitations: the risk of weight gain, dizziness, and excessive sedation.
Traditional benzodiazepines (phenazepam, alprazolam, clonazepam), related to anxiolytics, are not recommended for long-term use, since pharmacological dependence develops after 14 days from the start of treatment.
Grandaxin
Therapy for TR requires long-term use of anti-anxiety medications. From the group of benzodiazepines, only tofisopam (the drug Grandaxin, Hungary) is approved for use for three months.
Grandaxin has anti-anxiety and vegetostabilizing effects, while there are no sedative and muscle relaxant effects, which is extremely important for elderly and senile patients [14]. In addition, Grandaxin does not have cardiotoxicity, which is important for patients with diabetes and concomitant diseases of the cardiovascular system [15].
A convenient dosing regimen and low cost are additional advantages of Grandaxin.
The effectiveness of TR therapy with tofisopam (Grandaxin) and hydroxyzine (Atarax) in patients with diabetes was studied by E.G. Starostina et al. in an open comparative randomized prospective study. Participants: 60 patients with DM and TR. The duration of treatment is three months. The observation period after drug withdrawal is one month. The condition of the patients before the start of treatment, after three months of treatment and one month after its completion was assessed using the Spielberg-Hanin scale and the Giessen Psychosomatic Complaints Questionnaire (GPCI). Tofisopam was prescribed in an average therapeutic dose of 50 mg three times a day.
Anti-anxiety therapy was accompanied by a decrease in psychological symptoms of TR. A good effect was observed in approximately 30.0% of patients, satisfactory – in 60.0%, no effect – in 9.0% of patients. The results of comparing the effectiveness of Atarax and Grandaxin are presented in the table.
Patients receiving Grandaxin experienced an improvement in carbohydrate metabolism - a decrease in HbA1c levels. In those taking Atarax, the dynamics of HbA1c did not reach statistical significance. In addition, treatment with Grandaxin, in contrast to treatment with Atarax, was accompanied by a significant decrease in heart rate, SBP and DBP.
At the end of the course of treatment, Grandaxin was discontinued immediately; no signs of withdrawal syndrome were recorded in patients. Tolerability of Grandaxin was characterized as good. One month after treatment, no relapse of TR was noted [16].
The positive effect of Grandaxin on the cardiovascular system in patients with coronary heart disease (CHD) was also demonstrated in a study by K.Yu. Skvortsova et al. It was shown that the addition of Grandaxin to complex antianginal therapy in patients with coronary artery disease was accompanied not only by a decrease in the severity of anxiety-depressive disorder, but also by a more pronounced decrease in the total duration of ischemia (by 53.0% compared with patients who did not receive Grandaxin) [17].
In the work of E.V. The Kulesh drug Grandaxin was used in 23 patients with coronary artery disease and various types of pain syndrome. During therapy, a decrease in psychoemotional disorders was observed in 19 (82.0%) cases. In eight out of 12 patients with atypical pain syndrome, its decrease was recorded. In no patient did the frequency and intensity of typical exertional angina attacks change significantly [15].
Thus, Grandaxin can be considered as an effective and safe drug for the treatment of TR in patients with diabetes.
conclusions
Science has demonstrated the direct and indirect effects of long-term stress on the development of hypertension and diabetes. When prescribing an antihypertensive drug, the doctor is responsible for patients from the moment of diagnosis until treatment. Therefore, it is necessary to take into account individual risk and seek the most appropriate solution for each individual patient.
According to guidelines for the treatment of hypertension published by the European Society of Cardiology, the first and perhaps most important goal is to reduce blood pressure itself to the target value, that is, less than 140/90 mmHg. Art., And for patients with CD – less than 140/85 mm Hg.
The new guidelines state that all major antihypertensive drugs—diuretics, beta blockers, calcium channel blockers, ACE inhibitors, angiotensin receptor blockers—are appropriate for the initiation and follow-up of hypertension. However, if the hypertension is refractory or the patient has a specific debilitating condition, such as stress or metabolic syndrome, other antihypertensive drugs, such as imidazoline receptor agonists such as rilmenidine, may be added.
Such drugs not only effectively control, but also reduce blood pressure variability. have a beneficial effect on metabolism, i.e. reduce insulin resistance, hyperactivity of the sympathetic nervous system, and heart rate.
It is important to understand that all drugs have side effects and contraindications, and therefore should be taken exclusively as prescribed by an endocrinologist.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter