Causes
For a long time, the main cause of vascular dementia was considered to be acute cerebrovascular accidents (hereinafter referred to as ACVA, which means, first of all, stroke). A stroke develops as a result of blockage of an artery by an embolus or thrombus (ischemic stroke) or when an artery ruptures and hemorrhages in the brain (hemorrhagic stroke). In this case, due to lack of nutrition, neurons die.
After a stroke, the likelihood of developing vascular dementia increases significantly. Within 1 year after a stroke, vascular dementia develops in a quarter of patients. The nature of the manifestation of symptoms depends on the area of the brain in which the disorder occurred. The size of the lesion also plays a role. Vascular dementia usually develops when more than 50 ml of brain volume is affected.
However, if circulatory disorders occur in areas important for cognitive functions (visual thalamus, hippocampal region, frontal prefrontal cortex, etc.), then a smaller area of neuronal death can lead to the development of vascular dementia. If other areas are affected, motor disorders and other post-stroke manifestations may occur.
It has now been established that vascular dementia is not always associated with acute disorders. It can occur due to a chronic dyscirculatory process - blockage of small vessels that occurs unnoticed by the patient (the so-called subcortical vascular dementia). It has also become possible to detect these disorders thanks to the spread of digital technology and the spread of neuroimaging methods in medicine.
Neuroimaging (functional MRI, PET, etc.) allows one to observe “silent” areas of vascular lesions in the brain that previously went unnoticed as not leading to an acute lesion (stroke). The development of vascular dementia is possible with a decrease in blood perfusion in the brain.
This occurs against the background of acute or decompensated chronic heart failure, a decrease in circulating blood volume, and a sharp decrease in blood pressure. All these phenomena lead to insufficient blood supply in the peripheral microcirculatory zones of all vascular beds and neuronal death. Based on this, the occurrence of vascular dementia is influenced by two components: stroke and a chronic discirculatory process. When these disorders occur simultaneously, they reinforce each other, leading to more pronounced symptoms.
Let's consider the mechanism of development of vascular dementia.
When the vascular link in various parts of the brain is damaged, neurons do not receive the required amount of oxygen and nutrients, which leads to the death of these cells. Initially, the brain compensates for the violations - they do not appear externally. Over time, the potential is depleted, negative changes begin to affect the state of memory, speech, concentration and speed of thinking. As a result of these cognitive disorders, a person’s behavior changes, and his independence decreases.
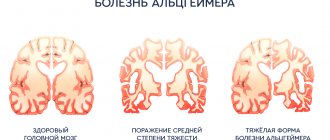
All types of vascular dementia account for up to 15% of all cases of dementia in the elderly. There are also often cases of mixed dementia, which combine vascular dementia with Alzheimer's disease. It is believed that as a person ages, the risk of vascular dementia decreases, while the risk of developing Alzheimer's disease increases.
In this regard, the vascular factor is recognized as especially dangerous in the Russian Federation, where life expectancy is still not very high and part of the population simply does not live to the age of onset of another type of dementia. Vascular dementia is also widespread compared to Alzheimer's disease in some Asian countries (Japan, China), and a number of Scandinavian countries (Finland, Sweden).
Risk factors for vascular dementia are:
- high or low blood pressure,
- cerebral atherosclerosis,
- hyperlipidemia,
- cardiac ischemia,
- diabetes,
- arrhythmias,
- hyperhomocysteinemia (now this factor is considered doubtful),
- pathology of heart valves,
- vasculitis.
Smoking, poor diet and a sedentary lifestyle contribute to the risk of developing vascular dementia.
Types of disease
Each type of senile dementia has its own code in ICD-10.
F00*
For Alzheimer's disease . The disease has neuropathological features and progresses over the years. The onset of the disease is 50–65 years .
Neurotic character traits become aggravated, anxiety and fear for oneself and loved ones come to the fore, poor memory aggravates the anxious state.
It is difficult for a person to express his thoughts. Over time, the help of a social worker is required. The pathological condition is dealt with by a neurologist and a psychiatrist.
Basic drugs with cholinesterase inhibitors that correct the patient’s well-being:
- Donepezil,
- Memantine,
- Nootropics.
Treatment with folk remedies:
- withania root,
- black tea with sugar,
- ginseng.
F01
Vascular dementia . The consequence of hypertension is damage to the blood vessels of the brain. Makes itself felt in old age.
Brain neurons die from insufficient blood supply, the cause is atherosclerosis and coronary heart disease. The attending physician is a neurologist.
Drugs
prescribed :
- Nootropics.
- Memantinol.
As additional treatment methods, you can resort to traditional medicine :
- lemongrass is steamed,
- Eleutherococcus is taken in drops.
Concomitant diseases : arterial hypertension, concussions, stroke.
F02.0
Pick's disease . A type of senile dementia with lesions in areas of the brain located in the frontal lobes.
It manifests itself in the same way: antisocial behavior, disinhibition of instincts, loss of cognitive abilities.
Treatment: neuroleptics and anticholinesterase agents.
F02.1*
For Creutzfeldt-Jakob disease . Genetic and viral pathology causes mutation of a healthy protein.
To read: Infantile amnesia: why don’t we remember our childhood?
The pathogenic prion protein accumulates in the body, destroying healthy brain cells (there are no cells suitable for the development of the virus in other tissues).
Cases of infection have been reported from eating beef.
Signs of pathology remain unnoticed until old age . It is after 55 years that the degenerative properties of tissues allow the protein to develop in the human body.
F02.2*
For Huntington's disease . A hereditary disease caused by degeneration of gamma-aminobutyric acid.
A hallmark of this type of dementia is the presence of hallucinations and antisocial behavior. The disease is transmitted by a dominant type.
This type of dementia is difficult to distinguish from other types; the only symptom, a marker of the disease, is hyperkinesia.
F02.3*
For Parkinson's disease . Parkinson's disease is a debilitating neurological condition that causes dementia.
A lack of dopamine in the brain and insufficient transmission of dopamine to nerve endings make it difficult to move smoothly and make speech poor.
Protein deposits in the brain replace healthy tissue, blocking dopamine receptors, resulting in akathisia and tremors.
F02.4*
For an illness caused by the human immunodeficiency virus [HIV] (B22.0+) . HIV dementia is a complex of symptoms caused by microorganisms that do not develop if a strong immune system is present.
The severity of this type of dementia in older people is practically not observed - this is a special form of HIV infection.
F03
Unspecified (NOS “not otherwise specified”) . Senile dementia with no symptoms.
The illness is on the verge of psychology/psychiatry and is often hysterical in nature. Common name: senile sclerosis.
Senile and presenile dementia
Presenile dementia occurs at early retirement age. Alzheimer's disease is an indicative type of presenile dementia.
A person ceases to understand the speech of others, and difficulty reading newspapers arises. The patient lets himself go.
Habits from a past life are forgotten, hygiene and comfort fade into the background.
Life activity decreases, by the age of 60–65 a person stops moving and slowly dies.
Alzheimer's type
Classic dementia of the Alzheimer's type is quite severe. It is diagnosed after 65 years , most likely, this is the middle - late stage of the disease.
To read: Nocturnal and other types of epilepsy in children and their symptoms
The patient cannot distinguish complex phrases spoken to him at moderate volume. The sounds of speech perceived from the outside turn into cacophony. Rigidity of character is due to the restructuring of the brain to a simplified mode.
There is no place for hobbies and friends in a person’s life; all the time he is focused on himself and his experiences. Amnestic dementia syndrome, as a marker of the disease, occurs at a late stage of the disease.
Characterized by the inability to remember any dates or numbers.
At this stage the person becomes incapacitated . Mnestic-intellectual functions disintegrate, a person completely loses the concept of time and space. The rhythm of wakefulness is disturbed, night sleep is superficial.
The prognosis of the disease is disappointing, leading to complete maladaptation and disability . The drugs relieve only neurological symptoms, such as high blood pressure and tremors.
Symptoms
As a rule, “vascular dementia” is diagnosed if cognitive impairment was preceded by a stroke. Quite often, accompanying signs are symptoms of focal brain damage, for example, manifestations of hemiparesis (weakness of the muscles of one side, anisoreflexia, pathological foot signs, etc.). A characteristic symptom is a walking disorder - a slow, shuffling gait and instability (which patients themselves often call dizziness).
As mentioned above, the cause of vascular dementia lies in circulatory disorders in the brain. The potential for disturbances to occur exists in different areas of the brain. Therefore, the external manifestations of vascular type dementia differ significantly in each case. Let's list the most typical ones.
Dementia caused by damage to the midbrain is manifested by mesencephalothalamic syndrome. The first manifestations are confusion and hallucinations. A person becomes apathetic, withdraws into himself, does not care about his appearance, and neglects personal hygiene. His psychophysiological state is usually characterized by increased drowsiness. In some cases there are speech disorders.
In dementia caused by damage to the hippocampus, first of all, there is an impairment in the ability of memory to retain information about current events (long-term memory can be retained).
As a result of a stroke, apathetic-abulsic syndrome is observed in the prefrontal regions of the frontal lobes. The patient behaves inappropriately, there is no criticism of the condition. Inadequacy consists in repeated repetition of one’s own words and actions, or the words and actions of others.
Subcortical lesions lead to disruption, first of all, of daily activities: it is difficult for the patient to concentrate on one subject and maintain one type of activity; problems arise with making plans. There is also a violation of the skills of information analysis (separation of the main from the secondary).
A stable sign of vascular dementia is impaired urination; it is observed in almost all persons suffering from dementia.
Symptoms of vascular dementia are also noticeable in the psycho-emotional sphere. There is a general decrease in mood and self-esteem, emotional instability, depression appear, and self-confidence is lost.
Causes of dementia
Dementia is a multi-etiological condition that may be based on various brain diseases. To date, several dozen diseases are known, the clinical picture of which can manifest itself as dementia. However, the most common causes of dementia in old age are the previously mentioned Alzheimer's disease, dementia with Lewy bodies (DLB), cerebrovascular disease, frontotemporal degeneration, Parkinson's disease, etc. In addition to primary diseases, dementia can occur as a result of systemic metabolic disorders associated with uncompensated somatic diseases, intoxications, and deficiency conditions.
Diseases leading to dementia
The main diseases leading to dementia can be divided into the following groups.
I. Neurodegenerative diseases. II. Vascular diseases of the brain III. Mixed dementia (presence of post-ischemic cysts, senile plaques and neurofibrillary tangles) IV. Dysmetabolic encephalopathies V. Neuroinfections and demyelinating diseases VI. Traumatic brain injury VII. Brain tumor VIII. Liquorodynamic disorders (normotensive resorptive hydrocephalus).
Neurodegenerative diseases
Alzheimer's disease.
Dementia with Lewy bodies.
Frontotemporal dementia (FTD).
Primary progressive aphasia.
Corticobasal degeneration.
Dementia with predominant damage to the basal ganglia:
• dementia due to Parkinson's disease;
• dementia with progressive supranuclear palsy;
• dementia with Huntington's chorea;
• dementia due to other degenerative lesions of the basal ganglia.
Vascular diseases of the brain
Consequences of a single stroke in a “strategic” zone.
Multi-infarct dementia.
Vascular dementia associated with chronic cerebral ischemia.
Binswanger's disease.
Dysmetabolic encephalopathies
Alcoholism.
Hypoxic encephalopathy.
Somatogenic disorders:
• hypoxemia (with respiratory failure);
• hepatic encephalopathy;
• renal encephalopathy;
• hypoglycemic encephalopathy.
Hypothyroidism.
Deficiency states (deficiency of B1, B12, folic acid, proteins).
Intoxication with metal salts (aluminum, copper).
Intoxication with drugs (anticholinergics, barbiturates, benzodiazepines, neuroleptics, lithium salts, etc.).
Hepatolenticular degeneration.
Neuroinfections and demyelinating diseases
HIV-associated dementia.
Spongiform encephalitis (Creutzfeldt-Jakob disease).
Progressive panencephalitis.
Consequences of acute and subacute meningoencephalitis.
Progressive paralysis.
Multiple sclerosis.
Diagnostics
Dementia of the vascular type is diagnosed in the presence of clinical data, characteristic anamnestic or neuroimaging signs of cerebrovascular disease: previous stroke or cases of subclinical local cerebral ischemia.
It is also important to have a cause-and-effect relationship and a relationship in time between brain damage of vascular etiology and the development of cognitive impairment. The very presence of dyscirculatory disorders according to neuroimaging, as well as the presence of neurological disorders - hemiparesis, speech and swallowing disorders, walking and urination disorders, are mandatory.
It is necessary to differentiate between Alzheimer's disease and vascular dementia.
Once the syndrome of dementia is identified, it should be syndromicly distinguished from depression, moderate or even mild cognitive impairment and delirium. To diagnose depression, various questionnaires and tests should be used (clock drawing test, HADS anxiety and depression scale, Montreal Mental Status Scale, MMSE test, etc.).
The distinction between vascular dementia and dementia due to Alzheimer's disease is often difficult. If in Alzheimer's disease the deterioration can occur slowly and constantly, then in the case of vascular dementia the deterioration occurs suddenly (for example, after stroke) and proceeds in stages.
When the vascular component predominates, the following signs are common: focal neurological symptoms (rigidity, hemiparesis, bradykinesia, bulbar disorders), neuropsychological disorders depending on the location of the cerebral infarction (aphasia, lack of sensory sensitivity, apraxia), gait disturbances (with Parkinson-like or ataxic movements), urinary disorders with urinary incontinence and urgency.
In addition to a thorough neurological examination and targeted laboratory tests, MRI or MSCT is necessary to identify infarcts and white matter lesions.
It must be remembered that quite often the same patient exhibits both signs of vascular dyscirculation and symptoms of Alzheimer's disease. Modern research indicates that the chronic dyscirculatory process is a risk factor for the development of Alzheimer's disease and plays a pathogenetic role in the neurodegenerative process, based on this, the vast majority of cases of dementia are mixed in their pathogenesis - vascular-degenerative.
ICD-10 - disease codes
F30 Manic episode
F30.0 Hypomania F30.1 Mania without psychotic symptoms F30.2 Mania with psychotic symptoms. 20 with mood-appropriate psychotic symptoms. 21 with mood-inappropriate psychotic symptoms F30.8 Other manic episodes F30.9 Manic episodes, unspecified
F31 Bipolar affective disorder
F31.0 Bipolar affective disorder, current hypomanic episode F31.1 Bipolar affective disorder, current episode of mania without psychotic symptoms F31.2 Bipolar affective disorder, current manic episode with psychotic symptoms. 20 with mood-appropriate psychotic symptoms. 21 with mood-inappropriate psychotic symptoms F31.3 Bipolar affective disorder, current episode of moderate or mild depression. 30 without somatic symptoms. 31 with somatic symptoms F31.4 Bipolar affective disorder, current episode of severe depression without psychotic symptoms F31.5 Bipolar affective disorder, current episode of severe depression with psychotic symptoms. 50 with mood-appropriate psychotic symptoms. 51 with mood-incongruent psychotic symptoms F31.6 Bipolar affective disorder, current episode mixed F31.7 Bipolar affective disorder, in remission F31.8 Other bipolar affective disorders F31.9 Bipolar affective disorder, unspecified
F32 Depressive episode
F32.0 Mild depressive episode. 00 without somatic symptoms. 01 with somatic symptoms F32.1 Moderate depressive episode. 10 without somatic symptoms. 11 with somatic symptoms F32.2 Severe depressive episode without psychotic symptoms F32.3 Severe depressive episode with psychotic symptoms. 30 with mood-appropriate psychotic symptoms. 31 with mood-inappropriate psychotic symptoms F32.8 Other depressive episodes F32.9 Depressive episodes, unspecified
F33 Recurrent depressive disorder
F33.0 Recurrent depressive disorder, mild current episode. 00 without somatic symptoms. 01 with somatic symptoms F33.1 Recurrent depressive disorder, current episode of moderate severity. 10 without somatic symptoms. 11 with somatic symptoms F33.2 Recurrent depressive disorder, current episode severe without psychotic symptoms F33.3 Recurrent depressive episode, current episode severe with psychotic symptoms. 30 with mood-appropriate psychotic symptoms. 31 with mood-inappropriate psychotic symptoms F33.4 Recurrent depressive disorder, in remission F33.8 Other recurrent depressive disorders F33.9 Recurrent depressive disorder, unspecified
F34 Chronic (affective) mood disorders
F34.0 Cyclothymia F34.1 Dysthymia F34.8 Other chronic affective disorders F34.9 Chronic (affective) mood disorder, unspecified
F38 Other (affective) mood disorders
F38.0 Other single (affective) mood disorders. 00 mixed affective episode F38.1 Other recurrent (affective) mood disorders. 10 recurrent short-term depressive disorder F38.8 Other specified (affective) mood disorders 21
F39 Unspecified (affective) mood disorders
Treatment
Treatment of vascular dementia should be aimed at correcting the pathological factors leading to this condition, as well as directly correcting cognitive functions. It makes no sense to describe all kinds of treatment regimens and give the names of specific drugs with their course and single doses in this article, because each specific case requires an individual approach.
The general principles of therapy for vascular dementia should be the correction of hypertension and cholesterol levels (however, you should not reduce cholesterol levels below 3.5-4 mmol/l due to the risk of a combination of Alzheimer's disease and vascular dementia, and Alzheimer's disease reacts negatively to low cholesterol levels , although, unfortunately, it is not entirely clear why), as well as the use of antiplatelet or anticoagulant therapy.
It is important to carry out a course of treatment with antioxidant (Mexidol, Cytoflavin, etc.), neuroprotective (Actovegin, Ceraxon, Cortexin, etc.), vasoactive (Sermion, Cavinton, etc.) drugs, with individual selection based on availability contraindications in the patient and the clinical picture as a whole, as well as (the author’s opinion), anti-dementia drugs should be used, and the drug of choice should be memantines (Akatinol, Marux, etc.).
An equally important point is non-drug therapy, namely proper patient care and psychological comfort. After all, if you are surrounded by close people, and they treat you with a positive attitude, life becomes a little better.
Forecast
At the present stage of development of medicine, the prognosis for recovery for any type of dementia is unfavorable. Dementia is considered to be an irreversible condition. There is also an unfavorable prognosis for work ability (a patient with dementia is a priori disabled), a relatively unfavorable prognosis for life, but vascular dementia itself is not the cause of the patient’s death.
Death often occurs due to cancer, acute vascular accident, and infectious lesions (especially important among which are diseases of the genitourinary tract due to poor hygiene in patients with dementia).