Our clinic specializes in neurology and immunology. We employ neurologists with additional training in immunology. We use a comprehensive approach to the treatment of diseases of the nervous system, including the diagnosis and treatment of demyelinating diseases.
- Infection. Infectious and post-infectious damage to the nervous system
- Oncology and damage to the nervous system
- Autoimmune aggression. Autoimmune process
- Stress. Mental stress. Mental stress relief
- Metabolic disease. Treatment of metabolic disorders
- Discirculatory encephalopathy, circulatory disorders, treatment
- Intoxication of the body. Removing intoxication.
- Demyelination. Foci of demyelination
Infection. Infectious and post-infectious damage to the nervous system
An infectious lesion of the nervous system is an inflammation of its various parts:
- The membranes of the brain and/or spinal cord (meningitis, arachnoiditis);
- Substances of the brain (encephalitis) or spinal cord (myelitis);
- Peripheral nerves (neuritis, polyneuritis);
- Nerve roots of the spinal cord (sciatica);
- Nerve plexuses (plexitis);
- Nerve nodes (ganglionitis).
How does infection damage the nervous system? There are two options:
- The introduction of the pathogen directly into the nervous system (neuroinfection), with the destruction of elements of the nervous system. This is typical for viral (tick-borne) encephalitis, meningococcal meningitis, neuroborreliosis, tuberculosis of the nervous system, neurosyphilis, Varicella-Zoster virus and other infections. In conditions of reduced immunity, many even relatively peaceful microbes can cause severe neuroinfections.
- Damage to the nervous system by overly aggressive immunity ( autoimmune damage ) as a result of “overheating” of the immune system under the influence of an infectious irritant. The immune system recognizes microbes by surface protein molecules (molecular epitopes). Sometimes the molecular epitopes of a microbe turn out to be similar in structure to the molecular epitopes of our own tissues, for example, tissues of the nervous system. Then immune aggression can be directed not only at microbes, but also at one’s own tissue . This is how autoimmune destruction of elements of the nervous system occurs. This is typical, for example, for viral infections (cytomegalovirus, Epstein-Barr virus, herpes types 1, 2, 6, 8, hepatitis viruses).
Normally, each of us encounters the majority of potentially dangerous infections periodically or constantly. In this case, the disease does not occur as long as the immune system is able to protect the body. Danger awaits when immune defenses are reduced. Microbes, not meeting adequate resistance, invade the body and often themselves further block the functioning of the immune system (secondary immunodeficiency state).
Treatment of infection alone, without correcting the immune response, is almost always ineffective due to re-infection. Therefore, when planning treatment, we examine in detail your immune status and antibodies to a number of infections. When the picture of immunity and the infectious background is clear, a treatment plan is drawn up, covering two tasks:
- Suppress infection;
- Regulate the functioning of the immune system.
Oncology and damage to the nervous system
Many malignant tumors contribute to the formation in the body of a large number of toxins and immune factors that are aggressive to the body’s own tissues, incl. to the brain and spinal cord, to peripheral nerves, muscles. Paraneoplastic disease of the nervous system is damage to the nervous system not by a tumor, but by the immune system under the influence of a tumor. We have specialists and modern laboratory tests to diagnose paraneoplastic diseases of the nervous system and experience in their treatment.
Read more about laboratory tests for suspected paraneoplastic diseases of the nervous system.
Intoxication and autoimmune aggression can cause paraneoplastic syndromes and damage:
- muscles,
- peripheral nerves,
- brain and spinal cord.
Symptoms of paraneoplastic processes can be very diverse:
- paralysis and paresis,
- sensitivity disorders,
- hearing and vision impairments,
- imbalance,
- mental disorders.
What tissues of the nervous system can be affected by paraneoplastic syndromes?
- Peripheral nerves – polyneuropathy and polyneuritis.
- Muscles – myopathy and polymyositis.
- Brain – encephalopathy, encephalitis.
- Spinal cord – myelopathy.
Antibodies to NMDA receptor (autoimmune encephalitis), IgG
Antibodies to NMDA receptors are specific proteins produced against NMDA receptors in the nervous system. These antibodies are the cause of autoimmune encephalitis.
Synonyms Russian
Anti-NMDAR, antibodies to N-methyl-D-aspartate receptors.
English synonyms
NMDA-receptor antibodies, anti-NMDAR, N-methyl-D-aspartate receptor antibodies.
Research method
Indirect immunofluorescence reaction.
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Do not smoke for 30 minutes before the test.
General information about the study.
NMDA receptors are located on the surface of neurons in the central nervous system. Excitation and inhibition of these receptors underlies the mechanisms of memory, learning and consciousness.
The production of specific antibodies to NR1-NR2 by heteromers of NMDA receptors causes a reversible decrease in their number, disruption of their function and the development of symptoms of autoimmune encephalitis.
NMDAR encephalitis is the most common form of autoimmune encephalitis and most often presents as a paraneoplastic syndrome. Diagnosed in young women and children, it is associated with neoplasms, most often with ovarian teratoma.
Symptoms are nonspecific, characteristic of psychopathological conditions: depression, delirium, sound hallucinations. As the disease progresses, neurological symptoms may appear: memory loss, involuntary movements in various muscle groups, disruption of the autonomic nervous system, including the development of unstable hemodynamics, and respiratory failure.
Patients are often hospitalized in psychiatric, infectious diseases hospitals, and neurological departments with suspected organic pathology of the brain.
Diagnosis of this type of encephalitis is quite difficult. The disease is not characterized by specific changes that can be detected by MRI or PET-CT of the brain. When examining the cerebrospinal fluid, the changes are nonspecific.
A reliable diagnostic test is the determination of antibodies to NMDA receptors in blood serum and cerebrospinal fluid. For this study, an enzyme-linked immunosorbent assay is used to determine native antibodies to NMDA receptors in biological fluids. This analysis has high sensitivity and specificity, allows for cancer screening, verification of the diagnosis and initiation of early etiotropic therapy.
Patients with early initiation of antitumor immunotherapy have a better prognosis for complete restoration of nervous system function.
What is the research used for?
- To determine the cause of a nervous system disease.
- For differential diagnosis of encephalitis.
When is the study scheduled?
- When the genesis of psychopathological and neurological symptoms is unclear.
- With the simultaneous presence of psychiatric and neurological symptoms, especially in young patients.
- For symptoms of encephalitis in patients with a family history of cancer.
What do the results mean?
Reference values
Titer
Reasons for the increased result:
- autoimmune NMDAR encephalitis.
Reasons for the lower result:
- absence of disease.
Who orders the study?
Neurologist, oncologist, infectious disease specialist, psychiatrist.
Literature
1) NMDAR encephalitis: which specimens, and the value of values. Andrew McKeon and Vanda A Lennon. Lancet Neurology, The, 2014-02-01, Volume 13, Issue 2, Pages 133-135, Copyright © 2014 Elsevier Ltd.
2) The Importance of Keeping in Mind the Diagnosis of N -Methyl-D-Aspartate Receptor Encephalitis. Michael S. Zandi, Belinda R. Lennox and Angela Vincent. Biological Psychiatry, 2016-08-15, Volume 80, Issue 4, Pages e15-e15, Copyright © 2016 Society of Biological PsychiatryVolume 7, Issue 12, December 2008, Pages 1091-1098 LN.
3) Cellular and Synaptic Mechanisms of Anti-NMDA Receptor Encephalitis. Ethan G. Hughes, Xiaoyu Peng, Amy J. Gleichman, Meizan Lai, Lei Zhou, Ryan Tsou, Thomas D.
Autoimmune aggression. Autoimmune process
Some diseases of the nervous system are associated with the body's aggression against itself, namely, with an attack of the immune system on the tissues of its own nervous system (demyelination). Some autoimmune diseases are triggered by infection. Before drawing up a treatment plan, we will examine your immune status and infectious background in detail.
Our main task is to find the cause of autoimmune aggression and prevent its further development. In many cases, it is possible to put the autoimmune process into long-term remission or stop it completely.
Examples of autoimmune diseases of the nervous system:
- Multiple sclerosis;
- Disseminated encephalomyelitis;
- Polyneuritis, polyneuropathy, polyneuropathy;
- CIDP (demyelinating polyneuropathy);
- Guillain-Barre polyneuropathy;
- Polyneuropathy in rheumatic diseases;
- Encephalopathy and polyneuropathy due to viral hepatitis;
- Fibromyalgia and chronic fatigue syndrome.
Similar phenomena are observed in rheumatic diseases, when immune aggression is directed against joints, ligaments, muscles, and blood vessels.
Causes of autoimmune processes
Why do autoimmune diseases appear? This is usually due to the unfortunate coincidence of three main factors:
- Hereditary characteristics – autoimmune reactions occur more easily in people with certain genetic characteristics.
- Increased activity and decreased “intelligibility” of the immune system , which often occurs under the influence of stress, lack of sleep, operations, injuries, infections.
- The introduction of an infectious agent (virus, bacterium, parasite, fungus), similar in its antigenic structure to the myelin protein (sheath of nerve fibers). In such a situation, immune antibodies to the infectious agent will also be aggressive towards healthy tissue of the body.
The “phenomenon of myelin decompaction” is known, when, as a result of infectious or autoimmune damage, deep-lying myelin antigens are exposed, with which the immune system normally does not contact at all. These antigens are perceived by the immune system as foreign, and autoreactive immunocompetent cells and antibodies (autoantibodies) are formed to them, triggering further immune aggression.
Molecular mimicry and autoimmune reaction. The antigens of some microbes are similar to the autoantigens of healthy body cells. 1-Immune cell; 2-Infectious agent; 3-Nerve; 4-Identical receptors.
The resulting aggressive autoantibodies can participate in cross-autoimmune aggression to other tissues of the body . Therefore, in patients with demyelinating diseases, we often find other autoimmune processes:
- Autoimmune thyroiditis (inflammation of the thyroid gland);
- Fibromyalgia and chronic fatigue;
- Inflammation of tendons and joints;
- Antibodies to insulin and beta cells of the pancreas (risk of diabetes and obesity).
Treatment of autoimmune diseases
Treatment of any autoimmune disease involves reducing autoimmune aggression.
We get the most convincing treatment results from influencing three parts of the autoimmune process at once:
- Suppression of infection;
- Stimulation of weakened and suppression of “overheated” parts of the immune system;
- Regulating the functioning of the nervous system: restoring normal night sleep, reducing stress.
Stress. Mental stress. Mental stress relief
We know how to work with stress and its consequences. Stress not only depletes the nervous system, but also disrupts metabolism and immune function. During stressful situations, the body's functions are reorganized to prepare for a physical response to danger (to run, to fight). Being stuck in stress for a long time, in “combat readiness,” occurs to the detriment of the body’s current needs, and chronic diseases get out of control. Exacerbation of autoimmune diseases is especially characteristic. In most cases, the course of the disease can be significantly alleviated by preventing the influence of mental stress on the body.
The nature of stress . Stress is the body’s overpowering response to dangerous circumstances. The stress response to danger is provided by the evolutionarily ancient lower parts of the brain, which we inherited from fish (the autonomic nervous system).
Stress in humans, like in any animal, leads to an increase in the physical capabilities of the body (running fast, fighting, etc.), due to previously accumulated resources. All this happens independently of consciousness.
For example, someone yelled at you. In response, your heart began to beat, pumping blood into the muscles, the muscles tensed, the pupil dilated to improve vision, breathing became more active, saturating the muscles with oxygen, although you are not in physical danger and a forceful response is not required.
The stress response has not changed much in the process of evolution - under stress, the body prepares to repel a physical threat, even if no one is physically threatening.
In a social person, such reactions are usually not realized in behavior, and therefore remain for a long time in the form of an unrealized behavioral reaction. What if you are emotional, but control your behavior very well? This means that the nervous system will keep the body in an overactivated state for a long time, expending a huge amount of resources. .
In this case, there is a gradual depletion of the nervous system and metabolic disorder.
Stress and immunity. In chronic stress, the immune system becomes more aggressive, but is quickly depleted, losing the focus of the immune response.
In response to the introduction of an infection, a very strong, but insufficiently targeted response is possible, with an immune attack against the body’s own tissues:
- antimyelin process
- inflammation of peripheral nerves, muscles, joints, etc.
Therefore, in the treatment of autoimmune diseases of the nervous system:
- multiple sclerosis,
- disseminated encephalomyelitis,
- polyneuropathy, etc.
We often use modern antidepressants and psychotherapeutic treatment.
Reducing stress in the nervous system leads to significant changes in laboratory indicators of immune status and well-being.
Metabolic disease
A variety of metabolic disorders in the body can cause suffering in the nervous system because... it is very demanding in terms of nutrition and is very sensitive to the toxic effects of products of impaired metabolism. In our clinic, neurologists work in close cooperation with an endocrinologist; if necessary, we will offer you a joint consultation.
Most often we find two variants of metabolic damage to the nervous system:
- Polyneuropathy (polyneuropathy) is the suffering of peripheral nerve fibers (nerves of the limbs, optic and auditory nerves);
- Encephalopathy is a disorder of the brain substance.
A combination of polyneuropathy and encephalopathy is possible.
Treatment at our clinic includes:
- correction of metabolic disorders,
- restorative treatment for the nervous system (detoxification, nootropics, vitamins, magnetic stimulation, gymnastics, etc.).
Treatment of metabolic disorders at the Echinacea clinic
Some diseases that cause metabolic disorders that are detrimental to the nervous system:
- Diabetes mellitus is one of the common causes of polyneuropathy. More details here
- Hypothalamic syndrome is often accompanied by insulin resistance , i.e. cell immunity to the action of the hormone insulin. The nervous system is not able to absorb a sufficient amount of glucose. This is a possible cause of the development of polyneuropathy and encephalopathy. Read more here.
- Hypothyroidism, Thyrotoxicosis and Thyroiditis are diseases of the thyroid gland and a common cause of suffering in the nervous system. Read more here.
- Dysfunction of the parathyroid glands leads to disruption of calcium-phosphorus metabolism and calcium deposition in the subcortical nuclei of the brain. This is a possible cause of muscle cramps, hyperkinesis and secondary parkinsonism. Read more here.
- Liver and kidney failure are possible causes of damage to the brain and peripheral nerves. Characterized by increased levels of urea, creatinine, ALT, AST. GGT in biochemical blood analysis.
- Vitamin deficiency , especially B vitamins, can cause polyneuropathy. A typical case is a deficiency of B vitamins due to regular alcohol consumption.
- Storage diseases lead to the deposition of certain substances (copper, manganese, calcium, etc.) in the tissues of the nervous system and the death of its cells.
Tick-borne encephalitis
Encephalitis
Tick bite
Vomit
5899 01 February
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Tick-borne encephalitis: causes, symptoms, diagnosis and treatment methods.
Description
Tick-borne encephalitis is a dangerous viral infection that occurs in persistent natural foci and is manifested by high fever, intoxication and damage to the nervous system.
Causes of tick-borne encephalitis
The cause of the disease is an RNA-containing tick-borne encephalitis virus, which belongs to the genus of flavoviruses. Based on the composition of the genetic material and location of distribution, the Far Eastern, Ural-Siberian and Western subtypes are distinguished.
The virus is carried by ixodid ticks, which are also its main reservoir.
Thus, the virus is found where ixodid ticks live, the maximum increase in incidence is observed in May-June, and a second, less pronounced increase is recorded in late summer and early autumn, which is associated with the activity of ticks.
The virus cannot be transmitted from a person infected with tick-borne encephalitis to a healthy person.
The tick-borne encephalitis virus enters the human body in the first minutes of a tick bite or, which happens much less frequently, with the milk of an infected goat, or even less often, a cow. The virus initially multiplies and accumulates in the cells of the immune system, then enters the bloodstream and enters the lymph nodes, liver, spleen and other organs. There it multiplies and attacks the nerve cells of the cervical spinal cord, cerebellum, meninges, remaining there for a long time and penetrating deeper into the brain tissue.
Classification of the disease
The disease can occur in acute
or
chronic
form.
Non-focal acute forms are distinguished
, in the clinical picture of which it is impossible to identify a specific damaged structure of the nervous system, and
focal acute forms
with symptoms indicating the localization of damage to the nervous system.
The severity of the condition with tick-borne encephalitis can be mild , moderate and severe
.
Symptoms of tick-borne encephalitis
The incubation period (from the moment of infection to the first clinical manifestations) averages 7–12 days, but can vary from 1 to 30 days. Rarely during this period, precursors of the disease occur - general malaise, weakness in the muscles of the limbs and neck, numbness of the facial skin, headache, insomnia, nausea.
The disease begins acutely: with an increase in body temperature to 38–40°C, symptoms of intoxication (severe weakness, fatigue, sleep disturbances), as well as symptoms of irritation of the membranes of the brain (nausea, vomiting, severe headache, inability to press the chin to the chest ).
There is lethargy, confusion, redness of the face, neck, and upper half of the body. The patient may feel pain in the muscles of the whole body, most severely where movement disturbances will subsequently be observed; There may be numbness in areas of the skin or a sensation of crawling, burning, etc.
As the disease develops, the main symptoms appear, which determine its form. Most often, tick-borne encephalitis occurs according to the following clinical variants:
- in the form of fever
, lasting 3-5 days with symptoms of general intoxication, but without signs of damage to the nervous system. The outcome is a rapid recovery; - in the form of damage to the membranes of the brain
(most common in adults), which is manifested by unbearable headache, dizziness, nausea and vomiting that does not bring relief, photophobia; lethargy and lethargy appear. Body temperature is elevated, fever lasts 7–14 days. The prognosis is favorable; - in the form of damage to the membranes and substance of the brain
, when the symptoms of irritation of the meninges are accompanied by disturbances in movements in the limbs, including paralysis, visual impairment, hearing, speech, difficulty swallowing, etc. Sometimes convulsive seizures occur. The patient is poorly oriented in place and time, delusions and hallucinations are often observed. Recovery takes a long time, and movement disorders often remain for life. This is a severe form of tick-borne encephalitis, so death cannot be ruled out; - in the form of damage to the spinal cord
with the development of movement disorders (paresis and paralysis) in the muscles of the neck and limbs; - in the form of damage to nerve roots
and fibers with the development of disturbances in sensitivity and movement in the limbs.
Tick-borne encephalitis with a two-wave course of fever
is distinguished separately . The first rise in temperature is relatively mild, accompanied by symptoms of intoxication and irritation of the meninges, and the second (after a two-week break) with the development of a full clinical picture with signs of damage to the nervous system. Despite this, the prognosis is favorable, although transition to the chronic stage is possible.
Tick-borne encephalitis in children most often occurs in the form of fever or with signs of damage to the membranes of the brain.
Immunity to the virus after tick-borne encephalitis is lifelong.
Diagnosis of tick-borne encephalitis
To diagnose tick-borne encephalitis, it is necessary to confirm the fact of tick bite and the place where it occurred (find out whether the area is endemic for tick-borne encephalitis), clarify whether the patient has been vaccinated and whether immunoglobulin has been administered to him.
The doctor carefully examines the patient and conducts a complete neurological examination. It is important to exclude the possibility of other diseases, both infectious and non-infectious, accompanied by similar symptoms.
Laboratory diagnosis of tick-borne encephalitis includes determining the presence and increase in dynamics of the titer of IgM class antibodies and IgG class antibodies in the blood to the tick-borne encephalitis virus.
Discirculatory encephalopathy, circulatory disorders
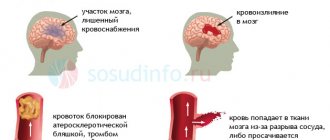
The human nervous system consumes a huge amount of energy and is therefore very dependent on nutrition. The delivery of oxygen, glucose and other necessary substances is provided by arterial blood. Metabolic products to be disposed of are evacuated with venous blood . With a lack of blood supply, the brain matter either gradually atrophies (encephalopathy) or dies within a few hours (stroke).
Poor cerebral circulation can be associated with narrowing and blockage of blood vessels for various reasons:
- Vasculitis (inflammation of blood vessels due to immune attack or infection). This rather dangerous disease usually leads to gradual, small-focal death of brain matter. With MRI, vasculitis is often confused with various types of encephalopathies and multiple sclerosis. More details here
- Atherosclerosis is the deposition of fat (cholesterol) between the layers of the inner walls of blood vessels. Deposition occurs in the form of plaques. Plaques bulge into the arteries and obstruct blood flow, causing chronic circulatory deficiency, with gradual atrophy of the medulla. The greatest danger is posed by ruptured plaques, fatty masses from which enter the blood and clog smaller arteries (stroke, acute cerebrovascular accident, cerebral infarction).
- An increase in blood coagulability and viscosity prevents blood from flowing through the smallest blood vessels (capillaries) and causes a chronic lack of blood supply to the brain. In addition, intravascular coagulation with blockage of the vessel is possible (stroke, acute cerebrovascular accident, cerebral infarction).
- Compression or tortuosity of a blood vessel. The arteries passing through the cervical vertebrae (vertebral arteries) are usually affected, causing dizziness, loss of balance, and visual and hearing disturbances.
Treatment of cerebrovascular accidents in our clinic begins with accurate detection of its cause. This is how we select a treatment method that is truly effective in this particular case. For diagnostics we use:
- Blood test for fats, vasculitis markers and coagulation;
- Doppler ultrasound and/or MR angiography to clarify the location of the narrowing of the blood vessel;
- X-ray, CT or MR tomography to look for deformations of the cervical vertebrae that are dangerous for blood vessels.
Diagnosis of Rasmussen's encephalitis
To make a diagnosis, it is important to collect all the patient’s complaints that may suggest this pathology. In the early stages of this disease, laboratory and instrumental methods are not very informative. In order to differentiate, the doctor prescribes additional examination methods, which include:
- laboratory tests of blood and urine - often no changes are detected;
- puncture and examination of the liquor fluid - no pathogenic microorganisms are detected;
- computed tomography - layer-by-layer examination of brain structures;
- MRI for Rasmussen's encephalitis - performed to check changes in dynamics;
- electroencephalography - a slow rhythm is recorded, peak-wave activity in the affected hemisphere;
- ophthalmological examinations - when examining a visual analyzer, structural changes are not visualized, but loss of a certain area or an entire field of vision can be diagnosed.
Intoxication of the body. Removing intoxication. How to relieve intoxication?
Intoxication is a painful condition associated with poisoning by any harmful substance (toxin), which adversely affects the state of the nervous system, liver, etc. Intoxication can be associated with the ingestion of a toxin from the external environment (ingestion, inhalation of vapors, etc.) or its formation within the body during various diseases. Many toxins lead to the death of: peripheral nerves (toxic polyneuropathy); brain substances (toxic encephalopathy); spinal cord (toxic myelopathy). Treatment of toxic lesions (intoxication) of the nervous system in our clinic involves detoxification and treatment aimed at restoring the functioning of the nervous system. Commonly used drugs for detoxification:
- Detoxifiers,
- nootropics,
- Antioxidants,
- vitamins (in case of intoxication with alcohol, lead, manganese, etc., administration of vitamins through a dropper may be indicated),
- restorative treatment after intoxication.
Detoxification - removal from the body of the substance that caused toxic encephalopathy and administration of drugs.
Intoxication with various substances can lead to various symptoms from the central nervous system:
- Alcohol, when consumed regularly, causes damage to the peripheral nerves of the arms and legs (alcoholic polyneuropathy) and the brain (alcoholic encephalopathy). Read more about alcohol intoxication.
- Lead causes mental agitation, impaired memory and intelligence, pain in muscles and joints, damage to nerve cells in the spinal cord with paralysis and other disorders. Poisoning is typical when in contact with certain types of gasoline, vapors containing lead (evaporation from batteries and lead melts).
- Manganese encephalopathy usually develops after consuming ephedrone, a homemade narcotic drug containing large amounts of manganese. Parkinsonism is characteristic, with impaired coordination of movements, tremors of the limbs, difficulties in changing body position, up to complete immobility.
- Long-term exposure to metallic mercury leads to a characteristic combination of cerebellar symptoms with mercury erethism (irritability, memory loss, insomnia, pathological fearfulness and embarrassment). Sometimes psychosis with mental agitation (delirium) develops. It was first described in workers involved in the production of felt hats, and was even called “mad hatter disease.” In individuals with certain immune conditions, low doses of mercury from dental fillings may cause abnormal immune reactions, but data on this issue are not yet sufficient.
- Intoxication in diseases of the kidneys and liver is associated with increased formation and/or insufficient excretion of metabolic products. Accumulated harmful metabolic products can cause damage to peripheral nerves and the brain.
- Intoxication in infectious diseases is caused by the formation of toxins as a result of the activity of pathogenic microbes and the destruction of body cells.
Classification of autoimmune diseases in neurology
The main autoimmune diseases affecting the central nervous system are:
- Multiple sclerosis and some rarer demyelinating diseases. Antibodies are produced against the sheath of nerve processes - myelin. The result is a disruption of signal transmission along nerve fibers. Main symptoms: various visual impairments, weakness and numbness of the arms and/or legs, unsteadiness, urination problems.
- Autoimmune encephalitis. A large group of diseases, the common feature of which is damage exclusively to the brain. Each encephalitis is distinguished by a specific type of antibody and, therefore, by some features of the clinical picture. However, for all autoimmune encephalitis there are a number of common symptoms: mental disorders, memory impairment, seizures.
Autoimmune diseases affecting the peripheral nervous system (nerve roots and nerves):
- Guillain-Barre syndrome. Acutely developing autoimmune disease. Antibodies are produced against the myelin of peripheral nerves. It manifests itself as ascending muscle weakness up to weakness of the respiratory muscles, less often numbness.
- Chronic autoimmune polyneuropathies. A group of diseases that manifest themselves as various combinations of weakness and numbness of the limbs and have a slowly progressive course.
Autoimmune diseases affecting the muscles and neuromuscular system:
- Myasthenia. Antibodies in myasthenia gravis affect the area where nerves and muscles connect—the synapses. As a result of exposure to antibodies, the sensitivity of the muscles to the signal coming from the nerves is reduced. Clinically, the condition is manifested by muscle fatigue - muscle weakness is not felt constantly, but increases gradually during movement.
- Myopathies. Muscle damage can also be autoimmune in nature. These diseases are united by a common symptom - muscle weakness, the severity and localization of which, however, varies depending on the disease and the type of antibodies.
Demyelination. Foci of demyelination
Myelin is the sheath of nerve fibers. Demyelination is the destruction of the nerve sheaths, and then the nerve fibers themselves. Demyelination of the brain, spinal cord, and peripheral nerves can occur for a variety of reasons. The most dangerous demyelination is due to the aggression of the immune system against myelin proteins. Treatment of demyelinating diseases in our clinic (DMD) involves searching for and treating the causes of demyelination and stimulating remyelination processes.
Possible causes of demyelination:
- Immune attack on proteins that make up myelin. This occurs due to an error by the immune system, under the influence of infection, or innate characteristics of the immune system. The immune system perceives myelin proteins as foreign and destroys them. This is typical for multiple sclerosis, multiple encephalomyelitis, chronic inflammatory demyelinating polyneuropathy (CIDP), Guillain-Barré syndrome, rheumatic diseases, and chronic infections.
- Metabolic disorders can lead to malnutrition and loss of myelin. This is typical for diabetes mellitus and thyroid diseases.
- Neuroinfection . Myelin can be a target of attack by certain infections, primarily viral ones.
- Paraneoplastic processes are complications of cancer.
- Intoxication with chemicals or aggressive waste products of the body itself (free radicals, peroxides).
Remyelination is the process of repairing myelin sheaths. The remyelination process can be stimulated in different ways - more details on this page
Treatment of Rasmussen's encephalitis
There are various therapeutic areas, namely:
- Symptomatic - involves taking anticonvulsants, anticonvulsants;
- Pathogenetic therapy - its effectiveness has not been fully proven. However, anti-inflammatory drugs, immunosuppressants and immunomodulators, and glucocorticosteroids can be used as a complex prescription. If there is no result, they can use plasmapheresis - purification of the blood from harmful, toxic substances, or immunosorption - removal of individual immune defense cells from the blood plasma;
- The surgical approach consists of performing an operation for Rasmussen's encephalitis. It can be done by removing the focus of the affected hemisphere of the brain or simply separating it from other anatomical and physiological structures, followed by deprivation of trophism.