Behavioral therapy in the treatment of overactive bladder and urinary incontinence
The International Continence Society (ICS) defines overactive bladder (OAB) as a condition in which the patient experiences a sudden urge to urinate that is difficult to control, often accompanied by frequent urination during the day and/or night.
OAB is not a disease, it is a complex of symptoms (syndrome), which in themselves are not life-threatening, but significantly reduce the patient’s quality of life. This diagnosis is established by excluding other possible conditions that have similar manifestations and require specialized treatment (for example, urinary tract infection).
According to modern data, about 16% of the adult population suffers from OAB. This disease occurs equally often in both women and men. However, in women, OAB is more often accompanied by urinary incontinence. The incidence of OAB and the severity of symptoms increase with age.
Today, there are many different treatments for OAB. According to the recommendations of the American Urological Association from 2012 (revision from 2014), all available treatment methods are divided into 5 groups depending on the ratio of benefits to the patient, as well as the invasiveness of treatment, the severity of possible complications and their reversibility.
The first line of treatment for overactive bladder is behavioral therapy. This type of therapy has no side effects, and its effectiveness is not inferior to therapy with M-anticholinergics, therefore it is recommended for all patients with OAB. However, to achieve maximum results, the patient is required to have the right attitude towards treatment, free time that the patient can devote to training, as well as periodic visits to a doctor or specially trained nurse for the purpose of correction and evaluation of the effectiveness of therapy.
“Behavioral therapy” is a collective term, it refers to a number of methods aimed at changing the patient’s habits or his environment. In most cases, these methods are used in combination with each other, which increases the effectiveness of therapy. There are two approaches to treating OAB using behavioral therapy. The first is to change bladder function by influencing urination patterns. In this case, a method called “bladder training” is used. In the second case, attention is paid to the pelvic floor muscles (exercises for the pelvic floor muscles to strengthen them and improve urinary retention, as well as teaching the patient techniques for suppressing the imperative urge to urinate).
Next, the main behavioral therapy methods used in the treatment of OAB will be presented.
Bladder training
The patient urinates at regular intervals. The initial interval is set based on the urination diary data and subsequently the interval between urinations gradually increases by 15-30 minutes.
*Bladder training is always combined with the technique of suppressing the imperative urge to urinate!
Suppressing the urgency to urinate
Against the background of an imperative urge to urinate, the patient makes rapid contractions of the pelvic floor muscles until the urge subsides. It is important to know that during an urgent urge you should not rush to the toilet. Motor activity against the background of an imperative urge only increases intra-abdominal and, consequently, intravesical pressure, which in turn strengthens the imperative urge. In addition, visual cues such as the bathroom or toilet can trigger urinary incontinence. During an imperative urge, you should sit down, if possible, relax the muscles of the body and perform a series of rapid contractions of the pelvic floor muscles aimed at suppressing the imperative urge. Only after the imperative urge to urinate has passed can you safely go to the toilet.
Exercises for the pelvic floor muscles
The patient performs 8-12 full voluntary contractions of the pelvic floor muscles. Each contraction is held for 6-8 seconds, after which the muscles relax. Rest between contractions is also 6-8 seconds. Upon completion of the exercise, 5-10 rapid contractions of the pelvic floor muscles are performed (without rest). This complex is performed 5 times a day.
Obesity
Based on clinical work, the positive effect of weight loss on urinary incontinence has been shown.
Smoking
To date, there are no studies proving the positive effect of quitting smoking on urinary incontinence. Nevertheless, this recommendation is quite logical: quitting smoking reduces the risk of developing bladder cancer. This recommendation is also appropriate in case of urinary incontinence, which manifests itself mainly when coughing.
Coffee
Consuming large amounts of caffeine contributes to the development of OAB.
Limiting fluid intake
This recommendation is appropriate for both patients with stress urinary incontinence and patients with OAB. In the first case, the positive effect is due to the fact that during physical activity, urine loss becomes significantly less when the bladder is not full. In the second, slower filling of the bladder associated with limited fluid intake leads to a reduction in the risk of involuntary contraction of the bladder muscle and, as a consequence, urgency.
*Applicable to patients with normal/high drinking regime. The drinking regime is established on the basis of a urination diary.
Frequent urination in women: what is “pollakiuria”, “polyuria” and “nocturia”
Frequent urination in women may be accompanied by an increase in urine output over 2 liters (polyuria) and normal daily diuresis, in which urine is released in small portions (pollakiuria). At night, urination is normally either absent or does not exceed once. Frequent urination at night is called nocturia.
Pollakiuria can be combined with pain and discomfort during urination, lower back pain, changes in general condition with an increase in temperature, which is most typical for inflammatory diseases of the bladder, ureters, pyelonephritis, exacerbation of urolithiasis.
There are many conditions in which frequent urination in women is not accompanied by pain. This:
- group of physiological conditions;
- endocrine diseases, when hormonal dysfunction affects the process of formation and excretion of urine;
- pathology of the kidneys and urinary tract;
- gynecological problems.
Let's look at all these reasons in more detail.
Physiological causes of frequent urination in women
It is natural that with an increase in the amount of fluid drunk, or consumption of caffeine-containing or alcoholic drinks (especially beer), urination becomes more frequent. When the body becomes hypothermic, or when swimming in ponds or pools, the urge to urinate also becomes more frequent. Eating large amounts of watery foods (watermelons, melons, cucumbers, cranberries) leads to increased urination, as they increase the water load on the body and have a diuretic effect. Various herbal preparations containing linden, thyme, lingonberry leaf, horsetail, mint and others have a similar effect.
Also, some medications that are used in the treatment of hypertension and heart disease increase the volume and frequency of daily diuresis due to their diuretic effect. By removing excess fluid from the body, these drugs stabilize blood pressure.
Pregnancy is a condition when the frequency of urination increases. In the early stages of pregnancy, this is due to hormonal changes in the woman’s body and the production of human chorionic gonadotropin (hCG), which increases the formation of female sex hormones - progesterone and estrogen - tenfold.
Progesterone promotes fluid accumulation in tissues and relaxes the muscles of the bladder and urethra. As a result of changes in hormone levels, increased urination occurs already in the first weeks of pregnancy. In the last three months of pregnancy, urination becomes more frequent due to the pressure of the enlarged uterus on the bladder, the presence of functioning kidneys in the fetus, and an increase in the amount of amniotic fluid and fluid in the body of the expectant mother.
During menopause, due to endocrine changes in a woman’s body, the tone of the bladder and pelvic floor muscles decreases. After 55 years of age, a woman’s urination becomes more frequent, and uncontrollable drops of urine are also possible as a result of urinary incontinence.
The production and excretion of urine is influenced by higher nervous activity. In case of fear, severe anxiety, or stressful situations, its production increases, which leads to a short-term increase in urination.
Mechanism of regulation of urine formation and excretion
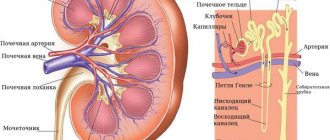
The leading role in the formation of urine belongs to the kidneys. The main structural unit of the kidney is the nephron, which consists of the glomerulus and a system of tubules with a collecting duct.
During the formation of urine, the following processes occur in the nephron:
- Filtration of blood and formation of primary urine up to 180 liters per day.
In this case, the liquid part of the blood with glucose, amino acids, sodium, potassium, calcium, phosphorus, salts and other compounds dissolved in it is filtered. The kidney filter normally does not allow blood cells and proteins to pass through. The filtration process takes place in the glomerulus, which is a collection of small capillaries. - Reabsorption is the reabsorption of primary urine components (water, glucose, amino acids, sodium ions, vitamins) into the body from the lumen of the renal tubules. The volume of reabsorption per day averages 178–179 liters, and the volume of residual urine is 1–1.6 liters. The reabsorption process is decisively influenced by antidiuretic hormone (ADH or vasopressin) and aldosterone. These substances regulate the reabsorption of water and sodium ions from primary urine. Any “breakdowns” in the production of these hormones can lead to changes in the volume and frequency of urination.
- Secretion is the release of harmful metabolic products (creatinine, urea, potassium ions, ammonia, drug residues, oxalates, urates, toxins) into secondary urine. Carried out by epithelial cells of the renal tubules.
Urinary organs - kidneys, ureters, bladder and urethra. The function of urine formation and urination is regulated by the coordinated work of the cerebral cortex, sympathetic and parasympathetic nervous systems, and hormones.
Therefore, both kidney disease and diseases of the nervous and endocrine systems can lead to frequent urination without pain. Bladder atony and overactive bladder are the results of a violation of the nervous regulation of urination.
Diseases of the female genital area in some cases can also affect urination due to anatomical proximity.
Endocrine diseases
Kidney function is influenced by vasopressin (antidiuretic hormone - ADH), aldosterone, as well as insulin and thyroxine. The following endocrine pathologies lead to frequent urination:
- Diabetes. The main symptom of this disease is an increase in fasting blood glucose levels due to an absolute or relative deficiency of the hormone insulin. When glycemia is more than 10 mmol/l, glucose is present in the excreted urine, which should not normally be present. Sugar “pulls water” and leads to an increase in the volume of urine produced, which causes urination to become more frequent. This symptom is combined with thirst and an increase in the amount of fluid drunk. It is also common for a woman to experience itching and inflammation of the external genitalia (vulvitis), which can additionally provoke a frequent urge to urinate.
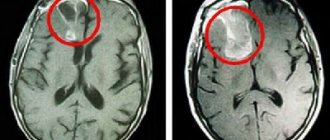
- Diabetes insipidus (diabetes) is a serious disease caused by insufficient production of antidiuretic hormone (ADH). This substance is formed in the hypothalamus and pituitary gland of the brain - centers for the production of many hormones in the body. The main effect of ADH is associated with the reabsorption of water from primary urine in the renal tubules and providing a certain concentration of urine. If the hypothalamic-pituitary zone is affected by a tumor, after neurosurgical interventions, in case of inflammatory diseases of the brain of any nature (viral, tuberculosis), or impaired blood supply, a deficiency in the production of ADH may appear. The result of this condition is polyuria up to 20–40 liters of urine per day, frequent painless urination, while the urine has a low concentration and is light. This condition is combined with severe thirst.
What kidney diseases can lead to frequent urination without pain?
Any kidney disease with a prognosis of chronic renal failure (CRF) can cause frequent painless urination in women.
With chronic renal failure, nephrons are gradually replaced by scar tissue. In the initial stages of insufficiency, there is an increase in urges at night, an increase in daily diuresis to 2–3 liters, while the urine becomes lighter and the specific gravity indicator in the general analysis decreases. As chronic renal failure progresses, the volume of daily urine becomes less than 500 ml, and the frequency of urination decreases. The kidneys cease to cope with the removal of harmful metabolic substances from the body.
Chronic renal failure can result from:
- Chronic glomerulonephritis is a lesion of the glomerular apparatus of the kidneys. Glomerulonephritis is provoked by hypothermia, bacterial and viral infections (scarlet fever, tonsillitis, streptoderma, chickenpox, etc.), autoimmune diseases (lupus erythematosus, vasculitis). The leading symptoms of glomerulonephritis are swelling, increased blood pressure and specific pathology in a general urine test (the presence of protein and leached red blood cells).
- Chronic pyelonephritis and nephritis - damage to the renal tubules and connective tissue of the kidneys as a result of prolonged inflammation, toxic effects of drugs (especially analgesics and non-steroidal anti-inflammatory drugs).
- Metabolic diseases: gout, urolithiasis, diabetes, amyloidosis. Gout is accompanied by the deposition of uric acid crystals and the formation of stones (urolithiasis) with the formation of a “gout kidney”, when the full functioning of the organ is impossible. With long-term diabetes mellitus, sclerotic damage to the glomeruli of the kidneys occurs - diabetic nephrosclerosis, which leads to the formation of chronic renal failure. Kidney amyloidosis is characterized by impaired protein-carbohydrate metabolism and deposition of amyloid protein in the renal tissue with the possibility of further development of chronic renal failure.
- Hereditary diseases and kidney anomalies: polycystic disease and various hereditary tubulopathies. Polycystic disease is manifested by the replacement of kidney tissue with cysts. Tubulopathies develop as a result of hereditary or acquired defects in enzymes that ensure adequate reabsorption of primary urine. This is renal glucosuria, when glucose is released in urine at normal blood sugar levels; renal diabetes insipidus, when the sensitivity of the renal tubules is reduced in relation to antidiuretic hormone. Accompanied by polyuria and frequent painless urination.
What gynecological diseases can lead to frequent urination?
The most common causes of pollakiuria in women are tumors and uterine prolapse, which cause pressure on the bladder and the urge to urinate with a smaller volume of filling.
Of all uterine tumors, the most common are fibroids. Their leading signs are disturbances in the woman’s menstrual cycle in the form of prolonged bleeding, pain in the lower abdomen, signs of anemia (weakness, drowsiness, dizziness, pale skin and mucous membranes).
Uterine prolapse is a condition that can occur in women who have given birth after 40 years of age. Predisposing factors for uterine prolapse are heavy physical labor with heavy lifting, excess weight, a tendency to constipation, ruptures during childbirth, a large fetus during pregnancy, and weakness of the pelvic floor muscles. Frequent urination occurs when the anterior wall of the uterus prolapses. In addition to this symptom, periodic pain occurs in the lower abdomen, sacrum and lower back, discomfort in intimate life.
In parallel with the prolapse of the uterus and the anterior wall of the vagina, a cystocele occurs - prolapse of the bladder. Cystocele develops as a result of weakness of the pelvic floor muscles, perineal ruptures during childbirth, and abnormal position of the uterus. The main complaints of a woman with cystocele are frequent urge, difficulty urinating, urinary incontinence when straining, and incomplete emptying of the bladder.
Comprehensive self-help program
Remember that only a psychologist with the required qualification level can choose methods of psychotherapy and draw up programs aimed at treating urinary neurosis. But there are times when the patient can try to get rid of this problem on his own.
A certain category of people will benefit from a program based on the well-known method of permanent desensitization. If you have problems with urination, you need to start making a detailed list of places of this process - from the simplest to the most problematic.
It is believed that many people suffering from bladder neurosis prefer to go to the toilet at home, being completely alone. Difficulties arise in most cases when visiting a public toilet. Therefore, you will have to find someone who can support you in self-treatment:
- A friend should stand behind the door so that when you pass urine you feel only comfort.
- When urinating, you can change the location of your friend, gradually moving him closer to the toilet door.
- After some time, such exercises can be started in a public toilet, choosing the least crowded place.
You can easily adapt such a program for yourself if you are worried about urinary incontinence. This therapy is successful if performed frequently, three to four times a week. Try to avoid negative thoughts until you empty your bubble.
Try to carry out your plan consistently; you should not act “under duress.” You should feel a significant improvement in your condition after just a few approaches.
If there are no positive changes, you need to visit a psychotherapist to apply more effective methods. People's bodies are different, and standard methods for solving problematic issues may not suit you. In this case, you will have to draw up an individual psychotherapeutic course program in order to achieve the expected effect.
Bladder neurosis is a neurological disease characterized by a frequent urge to urinate or, conversely, its absence. The disease has various development variations:
Urinary retention. It is impossible or not easy for a person to go small when there are other people nearby. This problem often occurs in schoolchildren. Frequent urge to urinate. The patient very often wants to go to the toilet, but he does not experience pain. With nervous tension, the disease worsens, and the person begins to walk even more often. But in this version, a person has no embarrassment in front of other people.
Bladder neurosis can manifest itself in the form of two differently directed symptoms.
- The first - the most common - is psychogenic urinary retention (paruresis). A person with symptoms of paruresis finds it difficult or impossible to urinate in the presence of other people. This is a fairly common problem, often first appearing at school.
- The second symptom is a constantly felt urge to go to the toilet, intensified as a result of nervous tension, as well as frequent urination. This manifestation of neurosis is often called nervous (neurogenic) bladder syndrome, although this is not an entirely correct name.
Both forms of neurosis are accompanied by various variations of fears of public shame. They are quite common types of social phobia, ranking second after fear of public speaking.
Diagnosis of the disease
Diagnosis is based on history and a thorough clinical examination. Cystalgia is diagnosed only after excluding other diseases of the bladder and urethra accompanied by dysuria.
Particular attention is paid to:
- for obstetric history and gynecological operations;
- on the nature of sexual relations (presence or absence of orgasm, painful intercourse), the use of contraceptives during sexual intercourse;
- collect data on menstrual function and previous diseases;
- for signs of inflammation of the genital organs, find out issues related to reproductive function.
An examination of the genital organs is mandatory. The external opening of the urethra is examined, since polyps and urethral prolapse often complicate the course of the disease. A laboratory examination of urine is carried out (the urine of patients with cystalgia does not have pathological changes).
Laboratory and X-ray radiological methods determine the function of the kidneys, upper and lower urinary tract.
Organic diseases of the bladder are excluded; for this purpose, cystoscopy and, if appropriate, other diagnostic methods (void cystoscopy, urethrocystography, ultrasound, etc.) are used. During cystoscopy, either no changes are noted in the mucous membrane, or there is an absence of a clear pattern of the mucosa in the area of the bladder triangle and the lower segment of the neck, as well as polyp-like growths on the neck of the bladder.
Patients with severe emotional neurotic disorders are consulted by a neurologist to exclude neurogenic dysfunction of the bladder, in particular, increased processes of contraction and relaxation of the detrusor and sphincters due to disruption of their innervation. In some cases, the hormonal function of the ovaries is assessed using the karyopyknotic index.
Causes of the disease
Today, much in the development of this urological disease still remains unclear, but, nevertheless, scientists have identified a number of factors that will play an important role in its development.
Reasons that can trigger the onset of cystalgia:
- the presence of certain gynecological diseases in a woman. In approximately 40% of such patients, the presence of cystalgia is also determined, especially if there is prolapse of the vaginal walls, the presence of tumor and inflammatory diseases of the pelvic organs;
- the presence of ovarian dysfunction, in approximately 68% of cases this is hypoestrogenemia, which as a result can provoke metaplasia (transformation) of the bladder epithelium, which will manifest itself as a certain violation of its basic functions. Most often, this phenomenon occurs if there is a disturbance in the menstrual cycle, as well as during menopause, during pregnancy, in the presence of hormonal changes occurring in the body;
- the presence of certain mental factors, which include conflicts and sexual dissatisfaction. In this case, the disease will be called psychosomatic cystitis;
- allergic mood of the body - for example, in a certain category of patients, as a result of taking a variety of dairy products, severe allergic swelling of the bladder neck occurs;
- impaired blood circulation and lymph drainage in the bladder area;
- imbalance of sex hormones, especially with a lack of estrogen;
- abortion;
- pelvic surgery;
- neurogenic bladder dysfunctions;
- congenital structural features of the genitourinary sphere;
- in rare cases, manifestations of cystalgia are a consequence of immunosuppression, so the examination will follow a specific plan - starting with a visit to a urologist and neurologist and ending with a study of the functioning of the immune system.
Get prices from the Israeli Ministry of Health
Enter your data and get the price list on Viber, WhatsApp or Telegram
In the case of cystalgia, there is initially no infectious agent or inflammation in the bladder area. Emotional, vulnerable women with an unbalanced nervous system suffer from cystalgia. They are not seasoned, pampered, perhaps under the influence of overly caring relatives.
Against the background of an unstable psychological state, any disease in the pelvic area becomes a trigger for the development of the disease. Such factors may include previously occurring acute cystitis, vaginitis, hypothermia, severe stress or shock.
All these factors cause a stagnant pathological reaction in the nervous system with excitation of nerve endings that are located in the wall of the bladder and in the urethral area. The woman begins to obsess over the sensations of discomfort in the bladder, stresses herself out, and gradually develops a fairly stable bladder dysfunction—cystalgia itself is formed.
Women who lead a sedentary lifestyle are more susceptible to cystalgia due to stagnation in the pelvis. Eating hot, spicy or salty foods also contributes to bladder dysfunction.
Symptoms and course of the disease
Almost all women who suffer from a disease such as cystalgia develop the same type of picture, which is directly influenced by strong emotional factors.
It is characteristic that all the main symptoms appear, most often, during the daytime.
Clinical manifestations:
- urination disorder;
- pain in the bladder and perineum;
- discomfort in the urethra.
Pain in the perineum and in the suprapubic region is usually clearly localized, radiating to the iliac or lumbosacral region (sometimes their localization is not clearly defined). As a rule, the pain is dull, constant, and appears during and outside the act of urination, during or after sexual intercourse; may occur without any reason and disappear after emptying the bladder. In addition to pain, there are often urinary disorders, expressed in pollakiuria, imperative and painful urination (especially at the end of the act), and a feeling of incomplete emptying of the bladder. The disease is characterized by a long course, alternating periods of remissions and exacerbations. Provoking factors can be cooling the body, constipation, drinking alcohol, spicy foods.
In almost all cases, the symptoms of cystalgia are not very pronounced. There is a very strong deterioration of the patient’s psyche, as well as a decrease in the standard of living as a result of unpredictable signs of the disease, which are disturbing due to their constancy. Most often, exacerbations are seasonal in nature, manifesting themselves most clearly in autumn and winter.
Manifestations may disappear and reappear after a few days or weeks, especially when provoked by stress. Examination of the bladder during cystoscopy does not reveal signs of inflammation, but there is an increase in blood filling of the vessels.
Treatment of bladder diseases
Neurogenic bladder dysfunction in adults: classification, symptoms, treatment
Bladder diseases in women, symptoms and treatment require correct diagnosis, medication and conservative methods of therapy. In order to promptly identify the disease and begin treatment, it is necessary to systematically monitor the woman with a doctor.
For urethritis
Therapy for urethritis may include antimicrobial drugs. For proper treatment, bacteriological urine culture is prescribed in order to identify the causative agent of the pathology. Individually for each patient, the urologist selects the most effective drugs that affect the identified pathogen, as well as therapy methods that help cure concomitant diseases and complications.
For cystitis
For cystitis, antibacterial treatment is prescribed using antibiotics, antifungals, antispasmodics, immunomodulators and other drugs.
It is recommended to take thermal procedures, douche with antiseptic agents, exclude spicy and smoked foods from food, drink more water, etc.
Anti-inflammatory folk remedies
Along with antibacterial drugs, it is recommended to combine treatment with the use of traditional medicine. For example, chamomile acts as an anti-inflammatory agent and kills pathogenic microflora. You can wash yourself and douche with chamomile infusion. Dill and cranberries are useful. Cranberry juice acts as a natural antibiotic for cystitis.
Find out how to treat urolithiasis in women from the material “Urinolithiasis, symptoms and treatment in women.”
For neurogenic bladder dysfunction
Since the causes of neurogenic bladder dysfunction are diseases of the nervous system and severe stress, the underlying disease that caused hypotension or spastic bladder dysfunction should be treated first. In addition to the urologist, a mandatory visit to a psychotherapist or psychologist is necessary.
It is usually very difficult to treat nervous diseases due to the need for an individual approach to the patient. If laboratory diagnostic methods have confirmed the absence of an inflammatory process in the bladder, then medicine suggests treatment with a psychotherapist, physical exercise, and taking sedatives.
For leukoplakia
Treatment of leukoplakia of the bladder initially comes down to conservative methods. They act medicinally on the causative agent of the pathological process. Antimicrobial, anti-inflammatory, immunostrengthening therapy is prescribed, as well as physiotherapeutic treatment of bladder structures using laser and electrophoresis, microwave treatment and magnetic therapy.
If there is no effect, surgical removal of the affected keratinized areas of the bladder is indicated through transurethral resection using a cystoscope inserted into the bladder through the urethra.
The procedure is safe, since the entire process takes place under the visual control of the surgeon due to the presence of a micro-camera and light radiation.
Another modern method for removing bladder leukoplakia is laser surgery, which is minimally invasive and non-contact. Foci of mucosal lesions are burned out and evaporate without bleeding, leaving only a thin film in their place.
After surgery, a course of hormonal therapy is prescribed to prevent relapse.
To diagnose leukoplakia of the bladder, a biopsy of the mucous tissue of the bladder wall is required, followed by histology of the resulting biopsy.
Self-medication of bladder leukoplakia is not acceptable, since the pathology is very serious.
Prevention of bladder diseases in women
Bladder diseases in women can be prevented. To prevent pathologies, effective prevention is needed:
- timely sanitation of chronic foci of infection in the genitourinary system;
- careful adherence to intimate hygiene rules;
- avoiding hypothermia;
- maintaining immunity;
- timely emptying of the bladder;
- proper nutrition and sufficient intake of clean water and fluids.
Dear women, since you are most susceptible to genitourinary diseases, monitor your condition! Do not self-medicate, get examined in a timely manner, and always be healthy and charming!
How neurosis manifests itself
A patient who suffers from bladder neurosis is usually very shy and sensitive. He reacts sharply to any criticism and remarks, he is afraid that other members of society will judge him for something.
This is due to the fact that because of the problem, such people feel very insecure and are afraid that they will be exposed.
Depending on the severity of the clinical picture, bladder neurosis can be divided into three degrees of severity - mild, moderate, severe. The first two forms can also appear in completely healthy people, for example, a strong desire to go to the toilet before some important public speech. But a severe degree develops into a phobia and terribly interferes with a person’s life.
Depending on what type of neurosis the patient has, his behavior may differ slightly. Characteristic signs for paruresis:
- to avoid visiting the toilet in public, patients severely limit their intake of liquid food or drinks;
- in order to urinate, such patients need complete privacy and silence (they spend more time in the toilet than a healthy person);
- such people cannot overcome themselves and urinate in public toilets, and they also cannot visit toilets anywhere, even with close friends;
- patients are embarrassed to go to the toilet if someone else is at home (especially if someone is waiting in line to see a white friend);
- they constantly have a feeling of anxiety, sometimes even panic, when the need arises to use a separate establishment;
- patients avoid going to public places for long periods of time. Long trips and travel will also be torture for them.
People suffering from paruresis cannot go to public toilets.
Symptoms of nervous bladder:
- constant obsessive fear of not being able to resist and wet yourself in public;
- reducing fluid intake to a minimum;
- an increasing feeling of anxiety that occurs if such a patient needs to leave the house, especially for a long time;
- before going even to the store, the patient carefully makes a plan where along the way he could go to the toilet;
- patients constantly run to the toilet, trying to squeeze out every last drop, this becomes an obsession;
- some always wear adult diapers to avoid embarrassment;
- Such people constantly condemn themselves and feel abnormal.
general information
Neurosis is a fairly common disease; according to statistics, it affects about twenty-two percent of the population; it is most often diagnosed in older people.
Neurosis and bladder disorder forces patients to urinate 8 times a day or more. The disease manifests itself in the form of 2 conditions:
- paruresis – shy bladder syndrome, in which the patient is unable to urinate if other people are near him. Males most often face this problem. According to experts, the phenomenon usually appears in people suffering from various nervous disorders, and it can cause a real inferiority complex;
- Cystalgia is a painful condition manifested by frequent urination, as well as a constant urge to go to the toilet, which intensifies due to nervous tension. However, there are no objective symptoms of damage to the bladder and other organs. It is a simulation of cystitis, but has nothing in common with this disease, except for similar symptoms. Basically, test results do not confirm the presence of cystitis. In this situation, it is necessary to seek help from a neurologist, since the problem lies in the functional pathology of the bladder. Cystalgia develops between the ages of twenty and fifty.
These conditions are common types of social phobia and are accompanied by different variations of fears of public shame. In children, the pathology is predominantly expressed in the form of enuresis.