Complex treatment of movement coordination disorders in Moscow. Diagnosis of the causes of ataxia and accompanying symptoms using the clinic’s advanced equipment, formation of an individual treatment program for the disorder using drug therapy and physiotherapeutic techniques.
Neurologist consultation
Chaika Natalya Vladimirovna
Neurologist, 1st category
Physiotherapist, hirudotherapist
11 years of experience
Leave your phone number. The clinic administrator will call you back.
Make an appointment
Admission fee for the promotion:
3000 rubles
We treat any types of ataxia:
- Vestibular - if you suffer from dizziness, frequent nausea and vomiting, hearing loss, gait has become unsteady.
- Cerebellar - if there is a lack of coordination of movements in the dark and with eyes closed, the gait becomes unsteady, the reaction becomes slow, and speech becomes slurred.
- Cortical - if walking is unsteady, it is difficult to take a step or turn, stand still, and auditory hallucinations appear.
- Psychogenic - if walking becomes broken and weaving, with crossing legs or sudden steps to the side.
- Sensitive – if you lose your balance when closing your eyes, and you have to raise your legs high and forcefully lower them to the floor.
Principles and goals of our work:
- We don’t just treat symptoms, but diagnose and eliminate the cause of the disease
- We use not only medications, but also advanced methods of hardware physiotherapy and a system of exercise therapy exercises
- We create individual therapy for disorders according to the symptoms and needs of each patient
- We restore healthy mobility and clear orientation in space, healthy hearing, speech and writing functions.
- We eliminate side symptoms - nausea, headache and neck pain, weakness, auditory hallucinations.
Symptoms
Specific manifestations of deterioration in coordination are:
- loss of balance without movement (in a standing or sitting position (static ataxia);
- gait instability, imprecision of movements (kinetic ataxia);
- a feeling of loss of balance in the absence of a visual stimulus, with eyes closed (sensitive ataxia).
Damage to the vestibular apparatus often occurs asymmetrically, which is also a distinctive symptom. With this pathology, the body deviates towards the localization of the lesion. This symptom is revealed if you ask the patient to take a few steps with his eyes closed.
In addition to deterioration in coordination, patients are usually concerned about the following manifestations of dysfunction:
- hearing impairment;
- dizziness;
- noise in ears;
- nystagmus;
- nausea or vomiting.
Consequences of coordination disorders. Why do you need a doctor?
Problems with walking and reaction, orientation in space and making simultaneous body movements is a dangerous condition in itself: after all, it does not allow you to fully work and live in society, and can cause an accident in the workplace or domestic accidents. But even more dangerous can be those destructive processes and diseases that are hidden behind discoordination:
- Multiple sclerosis
- Consequences of a stroke
- Chronic cerebral ischemia
- Acute alcohol or drug poisoning
- Brain tumors
- Diabetes
- Hypothyroidism
- Infectious diseases (HIV, neurosyphilis, cerebellitis, etc.)
- Congenital malformations of the brain
- Genetic metabolic diseases
Without timely diagnosis and the help of doctors, these diseases progress, cause disability and take away lives.
Characteristics of the disease
Impaired coordination of movement is called “ataxia” by the medical term. This condition is a sign of an inflammatory process that was triggered by problems in the functioning and distribution of nerve impulses sent from the brain.
To carry out effective treatment, it is necessary to conduct a comprehensive diagnosis and eliminate the factors that initially influenced the process of human brain activity. Self-medication in such a situation is impossible and unacceptable. This is because serious consequences such as disability or death are possible.
The musculoskeletal system is subject to control by the nervous system. Neurons located in the spinal cord and brain are interconnected. Thanks to their coordinated work, a signal is transmitted to the main human organ. From there comes a response impulse that provokes action.
With high-quality communication between neurons from different areas, the signal is clear and lightning fast. If there are problems in any part, the impulse is supplied slowly or is absent altogether. The disturbance is called loss of motor coordination.
Most often, the disease occurs in older people who have crossed the 60-year threshold, regardless of whether they are men or women. The reason for the occurrence, first of all, is the aging of the body and the inability to clearly and fully carry out assigned tasks. The disease can develop not only in adults, but also in children.
How is the diagnosis done?
1. Consultation with a neurologist. At the initial appointment, the doctor reviews the patient's symptoms, takes a medical history, and performs a neurological examination and vestibular tests.
2. Diagnostic procedures. Based on the data obtained during consultation and testing, the neurologist prescribes an individual set of diagnostic procedures to the patient. This may include:
- General, biochemical blood test, hormone test
- X-ray of the skull
- Magnetic resonance, computed tomography of the brain and cervical spine (MRI and CT)
- Electrocardiography (ECG)
- Electroencephalography (EEG)
- Duplex scanning and rheoencephalography (USDG) of cerebral vessels
- Genetic analysis
3. Additional consultations. A neurologist can prescribe additional consultations for the patient with related specialists - a cardiologist, endocrinologist, oncologist, otolaryngologist and others.
Impaired movement coordination
06.05.2020
Not everyone who staggers is drunk!
If coordination of movements is impaired, dizziness and falls are possible, and as a result, injuries.
In this state, it is difficult for a person to control his movements. Often people with impaired motor coordination cannot care for themselves, which leads to disability. Causes of the disease.
• diseases of the brain (tumors, injuries, cerebrovascular accidents, etc.);
• various neurological diseases; • diseases of the vestibular apparatus (labyrinthitis, vestibular neuronitis, etc.) • alcoholism, drugs, poisoning with toxic substances; • hormonal abnormalities; • hereditary diseases; • lack of vitamin B 12. Characteristic symptoms of the disease.
• The main symptom is unsteadiness when standing or walking.
A person cannot support himself on his feet, staggers in different directions, leans back, and falls are possible. • Tremor of the limbs is also a common symptom; when a person needs to perform a specific action, his hands begin to shake. For example, if he tries to bring a cup to his lips. Because of this, it is difficult for a person to serve himself. • Impaired handwriting due to the inability to make movements associated with fine motor skills. • Speech disorders. Speech becomes intermittent. • Breathing problems. Breathing becomes frequent, intermittent and uneven. • Dizziness and headaches may be accompanied by nausea and vomiting. ❗If such symptoms appear, you should immediately consult a neurologist. It is much easier to recover if the disease is detected early. An experienced doctor will conduct an examination, check the state of the nervous system, collect an anamnesis of the disease, if necessary, prescribe additional examinations to make the correct diagnosis. Examinations necessary to make a diagnosis - impaired coordination of movements.
• CT and MRI of the brain and cervical spine will detect abnormalities in the structure of the brain, and the presence of tumors or hemorrhages will also be visible.
• Examination by an otolaryngologist (ENT doctor) to examine the inner ear and evaluate your hearing. • Laboratory tests: a toxicological analysis will help identify signs of poisoning, a blood test to detect inflammatory processes in the body, checking the concentration of vitamin B12, a blood test to determine the content of hormones. • ECG. • Ultrasound of internal organs. Treatment.
Treatment of this disease is individual and is related to the cause that caused these deviations. You may need treatment from several specialists in addition to the neurologist. • If tumors or hemorrhages are detected, surgery is most often required. • To normalize cerebral circulation, drugs that improve cerebral blood flow are prescribed. • In case of poisoning with toxic substances, the body is cleansed using various solutions. • If there is a lack of vitamin B12, medications containing this vitamin are prescribed. • In addition to drug therapy, the following are prescribed: massage, physiotherapy, exercise therapy. In order to determine the disease in another person, conduct a 1-minute test with him: ask him to close his eyes and touch the tip of his nose with his finger or draw a geometric figure in the air. If movement coordination is impaired, it will be difficult for him to perform such actions. If you notice such abnormalities in yourself or your relative, immediately contact a neurologist at our medical center. The doctor will help you cope with this disease.
Back
Complex treatment
To fully treat motor coordination disorders and restore motor activity, we create an individual therapeutic complex, which includes both medication, exercise therapy, and physiotherapy methods.
Drug therapy
- Vestibular suppressants – for the treatment of dizziness and loss of spatial orientation.
- Antiemetics – for the treatment of nausea and vomiting due to dizziness.
- Stimulators of vestibular compensation - to restore the ability to maintain balance.
- Antithrombotic and vasodilator agents - for the treatment of blockage of cerebral vessels, improving local blood flow.
- Histamine preparations - to restore hearing, eliminate tinnitus, improve blood microcirculation.
- Nootropics - to restore healthy thinking, memory, speech and concentration, reaction speed, to stimulate metabolism in brain neurons.
- Sedatives, antidepressants, antipsychotics - for the treatment of psychogenic ataxia against the background of mental disorders, to increase the adaptive capabilities of the brain and central nervous system.
Exercise therapy for vestibular rehabilitation
The basis of vestibular gymnastics - physical therapy to restore the healthy functioning of the vestibular apparatus - are three types of exercises:
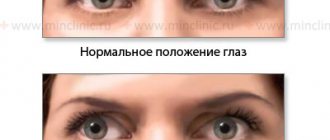
- For adaptation. Training to restore vision and improve the vestibulo-ocular reflex, which is responsible for visual acuity and maintaining balance when rotating the head.
- For habituation. Exercises to repeat characteristic body movements that cause dizziness, to develop habituation and gradually reduce the negative reaction to these maneuvers and body positions.
- For sensory replacement. Training on the use of preserved, healthy sensory systems to replace damaged ones - for example, on the use of the visual and somatosensory systems in cases of disorders of the vestibular system.
Physiotherapy
As an auxiliary therapeutic agent in the rehabilitation of balance, we use advanced methods of hardware physiotherapy:
- Translingual neurostimulation (TLNS). The impact of electrical impulses on the receptors of the tip of the tongue allows you to transmit a controlled signal through the brain stem to the structures of balance and coordination control - the cerebellum, vestibular nuclei and reticular activating system - and stimulate their healthy functioning.
- Biofeedback therapy with stabilometry. Under the guidance of an instructor, the patient undergoes classes on a stabilization platform, which evaluates the position and movements of his body. In this case, the person is connected by sensors to a biofeedback device (BFB) - it analyzes blood pressure, pulse and electrical activity of the brain. This procedure helps to explore the individual characteristics of walking and movement disorders and teaches the patient to cope with them.
- Magnetotherapy. The effect of magnetic fields on the brain and cervical-collar area improves blood supply and cellular interaction of the brain, helps eliminate muscle spasms and pinched nerve endings, and comprehensively improves the balance organs.
Conjugate eye movement disorders
Conjugate eye movement is provided by the centers of the cerebral cortex, midbrain, pons and cerebellum, as well as by pathways. Therefore, with lesions of the central nervous system, oculomotor disorders occur quite often.
In the case of unilateral pontine lesions , when the paramedian reticular formation or the nucleus of the abducens nerve is involved, horizontal gaze paresis develops, directed towards the lesion. Bilateral damage to these pontine structures causes complete horizontal paresis, in which eye movement is only possible in the vertical plane. In the case of a less severe lesion, incomplete horizontal paresis of gaze or installation horizontal nystagmus develops, with the direction of the fast phase towards the lesion. As a rule, other neurological symptoms are also present. With lesions of the cerebral cortex or the upper segment of the brain stem, horizontal gaze paresis may also occur, usually transient, without impairment of vestibulo-ocular reflexes.
It is known that the control center for vertical eye movements is located in the midbrain. Damage to the roof of the midbrain leads to paresis of upward gaze, occasionally in combination with a weakened pupillary response to light and while maintaining the reaction to accommodation and convergence of the eyes with converging nystagmus when looking upward. In young people, this convergence disorder is usually caused by pinealoma and hydrocephalus, in older people - by stroke. Paresis of downward gaze is less common; it can occur with bilateral damage to the center of the midbrain in the area of the red nucleus. Such paresis can occur acutely, for example, during a stroke, but as a rule, it develops gradually, occurring in the symptoms of Parkinson's disease, supranuclear progressive palsy and other degenerative diseases of the central nervous system.
With a lesion in the midbrain, a violation of the parallelism of the visual axes and in the vertical plane often occurs (the so-called vertical strabismus). This convergence disorder, at first glance, is very similar to trochlear nerve palsy, but differences still exist. In addition, other central oculomotor abnormalities, as well as focal neurological manifestations, are usually present.
Internuclear ophthalmoplegia is a central partial ocular convergence disorder caused by a lesion in the medial longitudinal fasciculus, which connects the pontine oculomotor nuclei with the midbrain. Such a lesion leads to paresis of the rectus medialis muscle on the side of the pathology, complete or partial disruption of the convergence of this eye, with nystagmus of the other when trying to look to the side. The condition of internuclear ophthalmoplegia can be unilateral or bilateral and not be accompanied by other neurological symptoms.
Multiple sclerosis is one of the common causes of acute bilateral internuclear ophthalmoplegia, especially in young women. Unilateral ophthalmoplegia, which occurs in the elderly, is usually caused by lacunar infarction and often manifests itself against the background of vasculitis (for example, with SLE), diabetes mellitus, cerebral aneurysms and other diseases.
With central lesions, either fast or slow eye movements are often selectively impaired. When saccades are disrupted, eye dysmetria occurs when, when the gaze moves from object to object, the eyes either “do not reach” it or “skip” it. In severe cases, opsoclonus varies in severity: from short saccades occurring in the horizontal plane (myoclonus) to constantly occurring chaotic saccades. Such convergence disorders may occur due to damage to the cerebellum or brainstem. The occurrence of opsoclonus is characteristic of neuroblastoma in children, as well as paraneoplastic syndromes, for example, in the case of oat cell lung cancer, in adults.
Disturbances of saccades occur in many degenerative pathologies of the central nervous system: Wilson's disease, progressive supranuclear palsy and spinocerebellar degenerations.
Congenital oculomotor apraxia is accompanied by the patient’s inability to direct the eyes in a given direction. Therefore, during the first two years of life, he develops saccadic compensatory head movements. Such a violation of eye convergence can also be acquired when lesions occur in the cerebral hemispheres or brain stem, which leads to the impossibility of saccades or the occurrence of slow and hypometric saccades.
Due to some pathologies of the central nervous system , smoothness in slow pursuit eye movements is lost and they become intermittent. This condition is not always a sign of a disease; these convergence disorders are often caused by fatigue, decreased attention, or taking certain medications. However, when slow pursuit movements are impaired in only one eye, this may indicate damage to the brain stem, parieto-occipital cortex, or cerebellum. Disturbance of vergence eye movements can also be psychogenic. At the same time, it can be difficult to distinguish it from an organic lesion. Ocular convergence may be impaired after stroke, demyelinating diseases, or traumatic brain injury. Patients report double vision when looking at close objects. Eye movements are preserved, with the exception of eye convergence. If this disorder exists for a long time in combination with reading difficulties, it can be assumed that congenital ocular convergence insufficiency is not associated with nerve damage.
Ocular convergence in some patients may persist even when looking into the distance. This may indicate the presence of a convergence spasm, combined with a spasm of accommodation, as well as constriction of the pupils. When accommodation spasm occurs, blurred vision occurs; it has both an organic nature, for example, with neurosyphilis, encephalitis, or traumatic brain injury, and a psychogenic nature - with emotional overload.
Diversion disorders are less common. One of their manifestations is the sudden onset of convergent strabismus and diplopia, while eye movements are preserved. In the case of an acute disorder, after an illness, the prognosis is favorable and no treatment is required.
Other causes include demyelinating diseases, encephalitis, neurosyphilis, and trauma.
MOTION DISEASE: DRUGS OF CHOICE
Preferanskaya Nina Germanovna
Associate Professor, Department of Pharmacology, Faculty of Pharmacy, First Moscow State Medical University named after. THEM. Sechenova, Ph.D.
Motion sickness itself is also a peculiar reaction of the body, arising from monotonous vibrations when moving in space. In 1881, JA Irwin proposed calling this condition a disease of movement - kinetosis (<gr. kinma (lat. kinesis) - movement).
To date, it has not been possible to fully elucidate the mechanism of motion sickness; the closest approach to this process is the theory of “sensory conflict”, which describes this condition as the body’s response to conflicting signals from the organs of vision and vestibular apparatus arriving at the centers of the brain and spinal cord. As a result, the processes of regulation of the body's reactions to maintain balance are disrupted. When the vestibular apparatus is overexcited, “motion sickness syndrome” occurs in poorly trained individuals. More often than others, people with low vestibular stability, women (10%) and children (from 2 to 12 years old - 58% and from 12 to 20 years old - 45%) are susceptible to motion sickness. A child under two years of age is more resistant to motion sickness; motion sickness is not observed in newborn children.
Depending on the individual characteristics of the body and the intensity of the provoking stimulus, various symptoms of motion sickness are observed: dizziness, pale skin, frequent yawning, excessive sweating, cold sweat, salivation, tachycardia, dyskinesia, nausea, vomiting, etc. English scientist AJ Benson, 1984), who studied motion sickness, considers this a normal reaction of a healthy human body that does not have any limitations or functional impairments.
Medicines that alleviate the suffering of people with “sea”, “air” and “road” illness are called anti-sickness, or anti-kinetic. There is no universal cure for motion sickness. Anti-motion sickness drugs are classified depending on their effect on vestibular receptors localized in the mediator systems of the cerebellum, medulla oblongata and other parts of the central nervous system. For this purpose, drugs from the following medicinal groups are used:
- antihistamines;
- antiemetics;
- anticholinergic drugs;
- agents that normalize microcirculation in the central nervous system;
- homeopathic anti-sickness remedies;
- anti-motion sickness herbal medicines;
- actoprotectors;
- nootropics;
- drugs belonging to different groups;
- Dietary supplement Let's look at the first two groups: antihistamines and antiemetics.
ANTIHISTAMINES Dimenhydrinate
(Dramine) is a complex salt of diphenhydramine with chlortheophyllinate. Blocks H1-histamine receptors - has an antiemetic, sedative, central anticholinergic, local anesthetic effect, depresses the central nervous system. It weakens the effects of vestibular stimulation, acting primarily on the otoliths, and in high doses – on the semicircular canals. Used for prophylaxis against sea and air sickness, for the treatment of vestibular and labyrinthine disorders. Available in tablets of 0.05 g (50 mg). To prevent seasickness or air sickness - 50-100 mg per 30 minutes. before the trip. The maximum daily dose for adults is 300–400 mg. When used, the following side effects may occur: dryness of the mucous membrane of the mouth, nose and throat, loss of appetite, urticaria, angioedema, bronchospasm. During the treatment period, care must be taken when driving vehicles and other potentially dangerous activities that require increased concentration and speed of psychomotor reactions.
Promethazine hydrochloride
(Pipolfen) - a phenothiazine drug - has antihistamine, antiallergic, sedative, antipruritic, hypnotic, antiemetic, local anesthetic effect, also providing an M-anticholinergic effect. Prevents and soothes hiccups. The clinical effect begins to develop after 20 minutes. and continues for 6 hours, sometimes up to 12 hours. Quickly and well absorbed from the gastrointestinal tract. With different routes of administration, it passes through the BBB and the placental barrier. More than 90% binds to plasma proteins. Metabolized in the liver to form sulfoxides and demethylated promethazine derivatives. The drug is widely used for migraines, sea and air sickness, and other kinetoses. Available in TB. 5, 10 mg for children and adults: 25 mg TB. and tablets of 25 and 50 mg. To prevent motion sickness, once 1 hour before travel: adults - 25-50 mg, children - 10-20 mg. When taken, dry mouth (if taken orally), nausea, constipation, drowsiness, anxiety, psychomotor agitation, and extrapyramidal disorders may occur.
Chloropyramine
(Suprastin) - has antihistamine, antiallergic, anticholinergic, antispasmodic effects, also blocking M-cholinergic receptors. It also has antipruritic, sedative and hypnotic effects. Concentration in the blood reaches a maximum within 2 hours. and remains at a therapeutic level for 4–6 hours. When used, lethargy, weakness, slowed psychomotor reactions, drowsiness, dizziness, impaired coordination of movements, dry mouth, nausea, gastrointestinal disorders may occur; rarely - gastralgia.
Meclozine
(Bonin) - chewable tablets with raspberry flavor - blocks H1-histamine receptors, has weak anticholinergic properties, blocks M1-cholinergic receptors, and also has an antiemetic effect. It is used for the prevention and relief of nausea, vomiting, dizziness during seasickness and air sickness. Apply 25 mg (1 TB) 1 hour before travel, but not more than 50 mg (2 TB). The drug has a long duration of action; 1 TB doses can be used repeatedly throughout the trip. 1 time per day. Contraindicated in children under 12 years of age, during pregnancy, and in patients with glaucoma. When using it, dry mouth, general weakness, and drowsiness may occur.
ANTIEMETICS
Metoclopramide, tb. 10 mg
(Reglan, Cerucal) - blocks D2-dopamine receptors of the trigger zone of the vomiting center and serotonin 5-HT3 receptors of the medulla oblongata, has an antiemetic effect, eliminates nausea and hiccups. The drug is used for vomiting, nausea and hiccups of various origins. Application: adults - 5-10 mg 3-4 times a day for 30 minutes. before meals (swallow the tablet whole and wash it down with a small amount of water); children over 6 years old - 5 mg 1-3 times a day. Side effects: constipation or diarrhea, dry mouth, feeling tired, drowsiness, headache, dizziness, depression. Use caution in patients with impaired renal function, children and adolescents.
Domperidone
(Motilium) - blocks D2-dopamine receptors in the myenteric plexus, peripheral and central dopamine receptors in the trigger zone of the medulla oblongata, eliminates the inhibitory effect of dopamine on cholinergic neurons, motor function of the gastrointestinal tract and increases the evacuation and motor activity of the stomach. Has an antiemetic effect, soothes hiccups and eliminates nausea. Recommended for adults and children over 5 years of age, administered orally within 15–20 minutes. before meals. Children under 5 years of age with chronic dyspeptic symptoms - 2.5 mg/10 kg 3 times a day and, if necessary, additionally before bedtime. For severe nausea and vomiting - 5 mg/10 kg 3-4 times a day and before bedtime. If necessary, the dose can be doubled. Allergic reactions such as skin rash and hives may occur during use.
Thiethylperazine
(Torecan) is a piperazine derivative of phenothiazine, a centrally acting antiemetic that blocks H1-histamine receptors and dopamine receptors in the nigrostriatal pathways. Unlike most phenothiazines, it has virtually no antipsychotic effect. It also has alpha-adrenergic and M-anticholinergic effects. Acts on the chemoreceptor trigger zone and the vomiting center. Eliminates dizziness by influencing coordination centers in the reticular formation. The effect develops quickly, usually after the first injection.
Indications for use: sea and air sickness; dizziness of central and vestibular origin. Used orally and rectally. Adults and children over 12 years old - 6.5 mg 1-3 times a day, in more severe cases - intramuscularly (with intravenous administration, severe arterial hypotension may develop. - Author's note) - 6.5-13 mg. Possible dry mouth, constipation, headache, dizziness, drowsiness, convulsions, decreased blood pressure, orthostatic hypotension, tachycardia, photosensitivity, retinal pigmentation, peripheral edema, agranulocytosis, leukopenia, thrombocytopenia.
To be continued…
How to do coordination exercises
Exercises with your body weight
You can choose several exercises and do them separately, or create interval training and pump up not only coordination, but also strength and endurance.
Moving around a square
Place your feet slightly wider than your shoulders, lean forward and place your hands on the floor - this is the starting position. At the same time, lift your right arm and left leg off the floor, turn your body to the right, turn over with your stomach towards the ceiling and lower your left foot to the floor, and place your right hand behind your back.
Then repeat the same in the opposite direction. Raise your left arm and right leg, turn your body to the right and return to the starting position. You can always perform this exercise in one direction, as shown in the video, or return in the opposite direction.
Jumping Lunges and Runner's Stance
Perform two jumping lunges with alternating legs. Then move your front leg back and place it on your toes, bend over with a straight back and touch the floor next to your supporting leg with the opposite hand. Move your other hand back, behind your back.
Practice at a slow pace to begin with to get the hang of the movement, then increase your speed.
"Skater" from a lunge
Lunge backwards and come out with a jump. Then lower yourself back into a lunge, and when you come out, jump to the side with your free leg. After landing, do not lower your other leg to the floor - immediately jump back and repeat the exercise from the beginning.
Try to jump to the side as far as possible, accompanying the movement with your hands. Do the required amount on one side, and then change legs and do the same on the other.
Burpee with side jump
Burpee uses many muscle groups and trains endurance. And if you add a little balance to it, it's a great coordination workout.
Perform a burpee on one leg and then jump wide to the side. If this is too difficult for you, try the speed skater jump variation. Do one push-up while lying down, and then three jumps from side to side, landing on one leg.
Chameleon
Squat down and place your hands on the floor. Walk your hands along the floor as far as you can while lying down, but do not straighten your knees. Without leaving the prone position, take a step forward with your right foot and left hand, and lower yourself into a push-up.
Then push yourself up, step with your right arm and left leg, and lower yourself back into a pushup. At each step, touch the floor with your chest, try to place your bent leg closer to your pelvis.
If your arms aren't strong enough to push up with each step, perform the movement at half the range, bending your arms just a little.
Somersault with a pistol exit
This exercise improves coordination, balance, and leg strength.
Roll forward, step onto one leg and extend the other leg forward. Rise up from the pistol and repeat again, this time getting up on the other leg.
If you don’t know how to do these squats yet, then it’s time to learn. After all, this is another great exercise for developing balance and coordination.
Learn