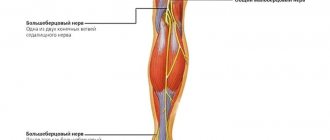
Our clinic is engaged in examination, treatment and rehabilitation measures for pinched, inflammation and injuries of the nerves of the legs (sciatic, tibial, peroneal and their branches). You will need to be examined by a neurologist. if any studies have been previously performed, be sure to take their results for consultation, incl. the x-rays themselves . If the studies have not been performed, we will do everything necessary in our clinic or with our colleagues in other clinics.
- What are the causes of damage to the tibial and peroneal nerves?
- Symptoms of Tibial and Peroneal Nerve Suffering
- Diagnosis of neuropathies of the tibial and peroneal nerves
- Treatment of damage to the tibial and peroneal nerves at the Echinacea clinic
- When is surgery necessary?
How the treatment will be structured:
- Let's establish the location and cause of nerve damage. We perform electromyography of the peroneal, tibial and other leg nerves and ultrasound of the nerves. The potential benefit of non-surgical treatment or strict indications for surgery (risk of complete nerve loss) can be determined using needle myography.
- We will find out and discuss with you the possibility of non-surgical treatment and the prospects for restoring nerve function. Medicines can be used here, incl. administration of anti-inflammatory and absorbable drugs directly to the point of compression or damage to the nerve. For the rehabilitation treatment of the sciatic, tibial and peroneal nerves, magnetic stimulation of the nerves of the legs is very effective: improvement is noticeable immediately or several days after the procedure.
- If the chances of restoring the peroneal or tibial nerve without surgery are low, we recommend surgical treatment . We perform most of the operations on an outpatient basis. You will be able to go home on the day of surgery. The budget for surgery without hospitalization is significantly less. If hospitalization is required, we will refer you to a trusted specialist. After surgical treatment, we will offer a course of rehabilitation treatment.
What are the causes of damage to the tibial and peroneal nerves?
The tibial and peroneal nerves pass through narrow canals formed by bones, ligaments, tendons and muscles. Nerve tissue is very delicate and vulnerable. Often we detect nerve suffering even with slight narrowing or deformation of the nerve canal. Narrowing or deformation of the tibial and peroneal nerve canals occurs:
- In case of injury (bone fracture, bruise, hemorrhage, sprain or wound); Often, when injured, the nerve is pulled into scarred tissue or compressed by a bone fragment; nerve injury can also be represented by a nerve bruise, partial or complete interruption.
- If there is compression in an uncomfortable position (a tucked or compressed leg while wearing uncomfortable shoes, position, unconsciousness or intoxication, under anesthesia);
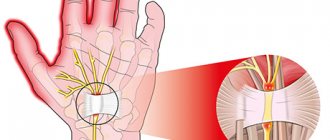
- With thickening and deformation of the knee and ankle joints and ligaments , with chronic injury and overload of the joints, often associated with the type of activity (sports, walking, forced posture, vibration, weight). Very often, such changes are facilitated by diseases and deformities of the spine. These types of neuropathy are called tunnel syndromes of the ulnar, radial and median nerves;
- For foot deformities due to flat feet (tarsal tunnel syndrome, meralgia) .
The function of nerves is to conduct electrical impulses from the brain to muscles and organs, and to the brain from sensory receptors in the body. Any damage to the nerve leads to disruption of the conduction of excitation along the nerve, which means disconnection of the affected part of the body from the brain.
Therefore, if the tibial and peroneal nerves suffer, the following are possible:
- Decreased strength and weight loss of leg muscles, twisting of the foot when walking and even fractures;
- Decreased sensitivity (numbness)
- Pain along the nerve or in the foot, fingers.
Diagnosis of peroneal nerve neuropathy
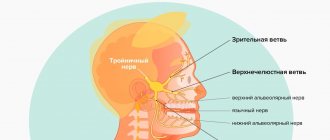
When diagnosing damage to the peroneal nerve (peroneal nerve neuritis), extension (dorsiflexion) of the foot and toes, as well as outward rotation of the foot, is impossible.
The Achilles reflex (from the tibial nerve) is preserved. Sensory disorders with peroneal nerve neuritis occur on the outer surface of the leg and dorsum of the foot. Articular-muscular sensation in the fingers is not impaired (due to the preservation of sensitivity from the tibial nerve). Pain with neuritis of the peroneal nerve is usually significant or absent, the same applies to trophic disorders.
The peroneal nerve is formed from the sciatic nerve.
When affected by neuritis of the peroneal nerve, the foot hangs down, is slightly turned inward, and the toes are slightly bent. There is noticeable wasting of the muscles on the anterior outer surface of the lower leg. The gait of a patient with neuritis of the peroneal nerve becomes very typical (“peroneal, cockerel,” “stepage”): the patient, in order not to touch the floor with the toe of the dangling foot, raises his leg high and first steps with the toe, then with the outer edge of the foot and, finally, with the sole.
The following are the main tests for peroneal nerve neuritis:
- Extension (dorsial flexion) and outward rotation of the foot, as well as extension of the toes, are impossible
- It is impossible to stand on your heels and walk on your heels
Diagnosis of the level of damage to the peroneal nerve during neuritis is made using electroneurography (ENG).
Diagnosis of neuropathies of the tibial and peroneal nerves
The most successful treatment for neuropathy is treatment directly at the point of nerve damage. For successful treatment, your treating doctor will find out:
- At what exact point is the nerve damaged (compressed); this helps us provide targeted treatment;
- What exactly led to the nerve suffering (trauma, scar, compression);
- The degree of nerve suffering (complete or partial damage, the presence of a recovery process, the presence of complete death of the nerve, etc.).
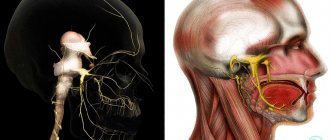
Often, to establish the cause of nerve pain, a detailed neurological examination is sufficient , during which the strength of the muscles controlled by the nerve, the possibility of certain movements, sensitivity, the presence of pain points and seals along the nerve are assessed. Auxiliary diagnostic methods are electroneuromyography, radiography and computed tomography.
Electroneuromyography allows you to assess the speed and volume of impulses along the nerve, detect the location of damage/compression, and determine the prognosis for recovery. Electromyography helps us evaluate the effect of certain types of treatment and choose the most suitable ones. The Echinacea clinic uses a modern computer electroneuromyograph.
X-ray and computed tomography of the joints and feet will provide complete information about the deformation of the joints and bone canals of the nerves, the causes and points of compression of the nerve.
Stimulation electromyography of the lower extremities
Peroneal nerve neuropathy
Neuropathy is the term for any nerve disease or disorder. When it affects nerves outside the brain and spinal cord, it is called peripheral neuropathy. When one nerve is affected, it is called mononeuropathy, and when multiple nerves are affected, it is called polyneuropathy. The most common mononeuropathy of the lower extremity (leg) affects the common peroneal nerve. Because the nerve has both a sensory (sensation) and a motor (muscle movement) component, damage or disease to the peroneal nerve can result in abnormal sensations (paresthesia), pain, muscle weakness, or paralysis.
Damage or disease to the peroneal nerve may be due to trauma or compression, infection, tumors, or inflammatory diseases of the nerves or tissues in general. However, most causes are due to trauma and nerve compression. Depending on the cause, the following may occur:
- demyelination - the insulating layer around the nerve wears away.
- nerve block (neurapraxia) - nerve impulses are not transmitted, despite the absence of damage to the nerve sheath or fibers.
- axonal damage (axonotmesis) - the nerve fibers that make up the axons are damaged, but the nerve sheath is not damaged.
- severed nerve (neurotmesis) - partial or complete rupture of a nerve.
Treatment of damage to the tibial and peroneal nerves at the Echinacea clinic
When it is clear where, how and why nerve compression occurs, local treatment in the form of physiotherapy, therapeutic blockades, massage, and manual therapy becomes much more effective. Therefore, treatment in our clinic begins with finding out the cause and location of nerve damage .
The main goals of treatment for nerve compression:
- Remove nerve compression. To do this, we use powerful resorption therapy: we use enzymes that resolve and soften scar tissue, bone and cartilage growths (Karipazim enzyme, etc.), massage, and injecting medications directly into the site of nerve compression. Sometimes, to release the nerve, manual therapy and massage of the areas of compression of the tibial and peroneal nerves (spine, leg joints, etc.) are sufficient.
- Accelerate healing and restoration of the nerve. To do this, we use modern medications that help restore the nerve that has been released from compression in the scars.
- Restore muscle function and volume. Special exercises, electrical stimulation of muscles, and physiotherapy are used here. The rehabilitator will tell you in detail and show you how to perform rehabilitation procedures at home.
Peroneal nerve damage causes
There is a wide range of causes of peroneal nerve injury or disease. It includes :
- Crossing your legs, which puts constant pressure on the nerve.
- Trauma to the leg, especially around the knee, including blunt force trauma or penetrating trauma.
- Surgery, especially knee surgery, although it can occur with hip surgery where the sciatic nerve may be affected.
- Fracture of the leg bones, especially the fibula.
- Repetitive leg strains while playing certain sports, especially when they involve kicking and dancing.
- Sitting or lying down for a long time, which affects the leg, especially the knee area.
- Knee problems such as dislocation, lenticular injury and osteoarthritis.
- Severe or repeated ankle sprain .
- Plaster casts or braces that cause repeated or prolonged pressure on the leg.
- Growths that cause nerve compression, such as ganglion cysts, schwannomas, or lipomas.
- strain due to prolonged squatting or sudden stretching.
- Compartment syndrome, in which pressure within the compartment due to swelling or bleeding compresses the nerve.
Other causes may affect the sciatic nerve and therefore affect its branches, or some conditions may not be specific to the peroneal nerve, such as generalized neuropathy.
When is surgery necessary?
In case of nerve injury, it is very important to decide in a timely manner whether conservative or surgical treatment is advisable. The answer to this question can be obtained after conducting needle myography, which will answer the question of what is the degree of damage to the nerve and whether it has a tendency to recover. If during this study it turns out that at least partially the nerve is preserved, we carry out active conservative treatment, after which we must repeat the study to make sure that the treatment had an effect . If, during needle myography, it turns out that the nerve is completely damaged and its restoration is impossible, we resort to the help of a neurosurgeon who suturing the nerve or releasing it from significantly narrowed canals. Then we perform the entire range of restoration procedures.
Causes of peroneal nerve neuropathy
The occurrence of peroneal nerve neuropathy can be associated with various situations. It can be:
- injuries (especially often this reason is relevant for injuries of the upper outer part of the leg, where the nerve lies superficially and next to the fibula. A fracture of the fibula in this area can provoke damage to the nerve from bone fragments. And even a plaster cast applied for this reason can cause peroneal nerve neuropathy. Fracture is not the only traumatic cause. Falls and blows to this area can also cause peroneal nerve neuropathy);
- compression of the peroneal nerve along any part of its course. These are the so-called tunnel syndromes - upper and lower. The upper syndrome develops when the common peroneal nerve is compressed as part of the neurovascular bundle with intense approach of the biceps femoris muscle to the head of the fibula. Typically, this situation develops in persons of certain professions who are forced to maintain a certain position for a long time (for example, harvesters of vegetables, berries, parquet and pipe layers - a “squatting” position) or make repeated movements that compress the neurovascular bundle in this area (seamstresses, fashion models). Compression can be caused by the “leg-to-leg” position, favored by many. Inferior tunnel syndrome develops when the deep peroneal nerve is compressed on the back of the ankle joint under the ligament or on the back of the foot at the base of the first metatarsal bone. Compression in this area is possible when wearing uncomfortable (tight) shoes and when applying a plaster cast;
- disturbances in the blood supply to the peroneal nerve (nerve ischemia, as if a “stroke” of the nerve);
- incorrect position of the legs (legs) during a long operation or a serious condition of the patient, accompanied by immobility. In this case, the nerve is compressed at its most superficial location;
- getting into the nerve fibers when performing an intramuscular injection in the gluteal region (where the peroneal nerve is an integral part of the sciatic nerve);
- severe infections accompanied by damage to many nerves, including the peroneal one;
- toxic damage to peripheral nerves (for example, with severe renal failure, severe diabetes mellitus, drug and alcohol use);
- oncological diseases with metastasis and compression of the nerve by tumor nodes.
Of course, the first two groups of reasons are the most common. The rest cause neuropathy of the peroneal nerve very rarely, but they cannot be discounted.
What are the reasons for the development of pathology
There are several factors that contribute to the development of peroneal neuropathy:
- nerve injuries (knee bruises, fractures, dislocations, sprains and tendon injuries, surgeries);
- vascular disorders;
- nerve compression;
- development of infection or toxic lesions.
It is worth mentioning the reasons that can cause compressor neuropathy, which has another name – “tunnel syndrome”. This can happen in connection with a person’s professional activity, when he has to squat for a long time. The development of this type of neuropathy is possible due to sitting for a long time, putting one leg on top of the other, while wearing narrow, uncomfortable shoes, and compression of the nerve occurs with a sedentary lifestyle.
The disease can develop as a secondary pathology against the background of another disease. For example, curvature of the spine or changes in the musculoskeletal system.
Axonal sensory and motor neuropathy of the peroneal nerve
Axonal neuropathy of the peroneal nerve is a lesion of individual axons, resulting in loss of only one innervation function. The fibers of the peroneal nerve contain motor and sensory axons. Depending on which of them are affected, a certain clinical picture develops.
Sensory neuropathy of the peroneal nerve is characterized by preservation of motor activity, but an almost complete absence of skin sensitivity. In this case, paresthesia and a crawling sensation may occur.
Motor neuropathy of the peroneal nerve is a lesion of motor types of axons. It manifests itself in the form of complete or partial immobilization of the foot and part of its toes (from the little toe). The patient cannot bend the foot or straighten the toes. But at the same time sensitivity is completely preserved.
In clinical practice, the most common type of lesion is a mixed type, in which the motor and sensory function of the peroneal nerve is simultaneously affected.
Compression-ischemic neuropathy of the peroneal nerve
Most often, patients are diagnosed with compression-ischemic neuropathy of the peroneal nerve - such cases account for 70%. This is due to anatomical features.
The peroneal nerve is a lateral branch of the sciatic nerve. It contains sensory and motor axons. Primary splitting of the sciatic nerve begins in the lower third of the thigh. The final bifurcation point is in the posterior popliteal fossa. The branches of the roots L4-L5 and S1-S2 participate in the formation of the peroneal nerve, therefore, when they are compressed at the level of the exit from the spinal column, neuropathy phenomena can also be observed.
Compressive neuropathy of the peroneal nerve may be associated with occupational activities. For example, if, while performing his work, a person is forced to spend a long time with his knees bent, then he develops upper tunnel syndrome. It is formed when the peroneal nerve is compressed near the head of the bone of the same name.
Inferior compression tunnel syndrome also occurs when the nerve is pressed at the point where it exits the ankle joint onto the foot. This form of the disease often occurs in people who wear uncomfortable, tight shoes or suffer from flat feet and clubfoot. Deformation of the ankle joint and scar changes in its ligamentous apparatus cause half of such clinical cases.
Ischemic neuropathy of the peroneal nerve may be associated with compression or impaired blood supply of central origin. Compression of the nerve fiber can be triggered by swelling of the surrounding soft tissues against the background of impaired microcirculation of blood and lymphatic fluid. Lymphedema of the lower extremities causes peroneal nerve neuropathy in approximately 10% of clinical cases.