Neurological diseases at the initial stage may pass without pronounced symptoms, but in an advanced stage they can cause irreparable consequences.
Severe pain in the shoulder joint may indicate a pinched brachial nerve, so you should definitely visit a doctor. If you neglect the problem or delay a visit to a neurologist, it can develop into vertebrobasilar insufficiency.
Therefore, at the first pain in the shoulder area, contact the specialists of the Kuntsevo Center. Our diagnostic base allows us to quickly conduct an MRI of the shoulder, ultrasound or electroneuromyography, based on the results of which the doctor will select the optimal treatment for the disease.
In addition, by contacting a rehabilitation center, you will save your precious time: here you can undergo diagnostic procedures, get advice from doctors, and also receive qualified recommendations for recovery.
Dozens of patients have already been able to verify the individual and effective approach of the treating staff to solving the problem of shoulder pain.
Pain by severity
A person can feel pain of varying intensity:
- Aching (also called somatic) - they appear rarely, it is difficult to establish the exact localization, and can last for days. Most often it occurs in bones and joints, causing a person a lot of inconvenience and discomfort.
- Acute - occurs unexpectedly and with high intensity, and can pass just as quickly. It is the first sign that brachial neuralgia is developing.
- Chronic – constant inflammation of tendons and joints causes the formation of chronic pain.
Pain by mechanism of occurrence
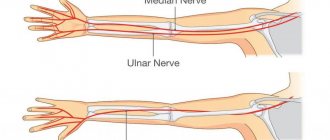
Evidence of problems with the cervical vertebrae is pain that is felt from the shoulder to the fingertips. In some patients, the arm may go numb for some time.
When you raise your arm and at the same time feel discomfort, you can talk about a problem with the supraspinal tendons.
There is another type of pain in the shoulder - when doing loads or physical exercises, the biceps hurts. This indicates a problem in the forearm.
Causes of pain in the collarbone
Traumatic injuries
A bruise in the clavicle area usually occurs with a direct blow to the shoulder girdle and is manifested by moderate, gradually subsiding pain.
The shoulder girdle is slightly or moderately swollen, bruising is possible. Palpation is painful. The function of the limb may be somewhat limited due to increased pain with movement. A clavicle fracture in adults develops when there is a blow to the shoulder girdle area, a fall on the shoulder, elbow, or outstretched arm. Accompanied by a very sharp explosive pain, sometimes with a crunching sound. Subsequently, at rest, the pain subsides somewhat, and with the slightest movements it intensifies, which forces the patient to support the sore arm with a healthy one. The shoulder girdle is swollen and deformed. In some patients, the protruding end of the fragment is visible under the skin or protrudes from the wound. The shoulder is lowered, shifted forward and inward.
In children, the collarbone breaks like a “green stick”, the fragments are connected to each other by the periosteum, the pain is usually mild, reminiscent of the pain syndrome of a bruise. There is a slight or moderate limitation of movements. The presence of a fracture is indicated by deformation of the shoulder girdle, protrusion of the middle part of the clavicle in the form of an obtuse angle.
A dislocated collarbone occurs as a result of a fall on the hand or a direct blow. There is a sharp pain at the time of injury, sometimes in combination with a click. When the acromial end of the clavicle is dislocated, maximum pain is determined just above the shoulder joint. The shoulder girdle is deformed, the end of the clavicle stands upward and backward, easily returns to its place when pressure is applied, but moves again when the pressure stops.
When the sternal end of the clavicle is dislocated, the patient complains of pain in the lower part of the neck on the left or right. The end of the bone is displaced upward, anteriorly or behind the sternum. In the first two cases, its protrusion is noted, in the last - retraction. Movement of patients with all types of clavicle dislocations is limited, but possible.
Degenerative processes
Pain syndrome in the distal part of the clavicle can be caused by arthrosis of the acromioclavicular joint. At stage 1, the pain is weak, dull and appears only when raising the arm up, sometimes accompanied by a click. At stage 2, the pain becomes more intense, aching, and bothers you with normal movements. At stage 3, movements are significantly limited, pain is constant, and ability to work is reduced.
Pain in the proximal part of the clavicle is caused by arthrosis of the sternoclavicular joint. At first they are noted only with sudden movements. Then they are provoked by everyday activity and intensify with deep breaths, but the clinical picture remains less pronounced than with the involvement of the acromioclavicular joint.
The clavicle is often affected by osteitis deformans. The pathology is manifested by continuous dull aching pain, which intensifies at rest, after rest. The collarbone increases in volume, the shoulder girdle is deformed. Possible fractures. Compression of the nerve is accompanied by neurological symptoms; when a nearby joint is involved, the clinical picture of arthrosis is revealed.
Inflammatory diseases
The most common inflammatory cause of pain in the clavicle area is myositis. Occurs during viral and parasitic infections, after injuries, and with some systemic diseases. It is characterized by moderate aching pain on palpation and movement, muscle weakness. The affected muscle is hardened. Slight local hyperemia and low-grade fever are possible.
Purulent periostitis of the clavicle is diagnosed quite rarely, it is manifested by severe pain, which increases over several days, becomes twitching, pulsating, bursting, and deprives you of sleep at night. The shoulder girdle is swollen, hyperemic, palpation is painful, and fluctuation can be detected during the formation of a purulent focus. Body temperature is increased. Subsequently, pus breaks through the skin or spreads to the underlying bone with the development of osteomyelitis.
Hematogenous osteomyelitis is also rare. It is characterized by unbearable acute pain of a drilling, pulsating, twitching nature. The pain is so intense that the patient freezes in bed, avoiding any movement. Local signs of inflammation are revealed. Chills, fever, and severe weakness are observed. Less often, the pain is moderate, the condition remains close to satisfactory.
Post-traumatic and postoperative osteomyelitis of the clavicle occurs with similar symptoms, but the purulent process does not develop as quickly, the pain syndrome is less pronounced, and progresses more slowly. The pathology occurs after open fractures, operations on the collarbone, and is accompanied by the appearance of purulent discharge from the wound and a deterioration in the general condition.
Arthritis of the acromioclavicular and sternoclavicular joints are often purulent in nature and are formed when infection spreads from nearby osteomyelitic foci. They manifest themselves as sharp, jerking pains that intensify with movement. The joint area is swollen, hyperemic, and the local temperature is elevated. General hyperthermia is noted.
Psoriatic arthritis of the sternoclavicular and acromioclavicular joints is rare and is combined with damage to other joints (usually the knees, shoulders, and small joints of the hands). A gradual onset is possible with increasing arthralgia, which reaches a maximum at night and morning hours and decreases with movement. The pain is dull, aching, nagging. Less common is an acute onset with intense pain.
Oncological lesions
Among benign neoplasms of the clavicle, chondromas, osteochondromas, and rarely chondroblastomas are most often detected. Neoplasia can be asymptomatic for a long time. As the tumor enlarges, the patient experiences short-term, vague pain in the collarbone, which intensifies as the tumor grows. When the tumor compresses nearby nerves and vessels, neurological symptoms and the development of trophic disorders may occur.
Primary malignant neoplasia and metastatic lesions of the clavicle are rarely diagnosed. They manifest themselves as rapidly increasing pain, intensifying after physical exertion, at night. Over time, the pain syndrome becomes painful, unbearable, and can only be eliminated by taking narcotic analgesics. Weakness, weight loss, increased fatigue, anemia, and hyperthermia are noted.
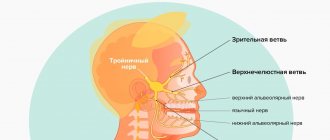
Neurological pathologies
Pain in the projection of the collarbone is quite typical for cervical osteochondrosis, disc herniation, spondyloarthrosis, and other neurological pathologies accompanied by compression of the nerve roots. The pain is pulling, shooting, burning, spreading from the neck to the shoulder, often radiating to the arm. Intensifies when turning the head or moving the hand. May be combined with dizziness and sensory disturbances in the limbs.
Scalenus syndrome occurs with osteochondrosis, poor posture, injuries, intense exercise in strength sports, and constant exposure to an uncomfortable static position. Usually manifests itself with acutely intense pain in the neck and shoulder girdle, radiating to the shoulder. The pain intensifies when moving the head and limbs, taking a deep breath. The strength of the limb muscles is reduced, and circulatory disorders are detected.
Brachial plexitis, which develops against the background of injuries, infectious, and dysmetabolic diseases, is characterized by aching, boring, aching, shooting pain in the clavicle area, spreading throughout the entire limb. The pain syndrome intensifies at night, during periods of physical activity, and is combined with limb weakness, sensory and trophic disorders.
With scapular-costal syndrome, a cerebral aching pain appears in the area of the scapula, then spreads to the collarbone, radiating to the neck, shoulder joint, and less often to the chest. Painful sensations intensify with changes in weather and movement. Sometimes the pain syndrome reaches high intensity, limiting the ability to work and the ability to self-care.
Pain in the shoulder girdle is observed with a cervical rib, accompanied by compression of the nerve trunks. They have a shooting, stabbing nature, occur or intensify with physical activity, sudden movements in the shoulder joint and neck, turning the head, raising the arm. Soreness in the collarbone is combined with pain in the forearm, and sometimes in the shoulder, neck, and head. There are disturbances in the sensitivity of the limb.
Other reasons
Pain in the collarbone in diseases of the internal organs is caused by irritation of the phrenic nerve. Taking into account the location of the pathological focus, the following are distinguished:
- Pain on the right or left
: focal or lobar pneumonia, pleurisy, subphrenic abscess, bleeding into the abdominal cavity, tumors of the diaphragm. - Pain in the left shoulder girdle
: angina pectoris, myocardial infarction, pancreatitis. - Pain in the right shoulder girdle
: biliary dyskinesia, cholecystitis, hepatic colic, biliary peritonitis, viral hepatitis.
Painful sensations in the collarbone and nearby tissues can be observed with mental disorders and depression. Sometimes a quickly transient pain syndrome is provoked by excessively intense training, carrying heavy objects in the hand or in a bag slung over the shoulder.
Causes
Neuralgia of the shoulder joint most often develops due to excessive physical stress on the hands and hypothermia of the joint.
There are often situations when a left-handed person lifts a heavy load with his right hand, which can cause a pinched nerve in the left hand (on the main working muscle group).
According to neurologists, the right shoulder joint is most often susceptible to pinching.
It is worth paying attention to the fact that there are factors that influence the acceleration of the development of neurological problems in a person. Among them:
- smoking and alcohol;
- improper and unbalanced diet;
- frequent colds.
Constant stressful situations are another aggravating factor, since they provoke the development of psychosomatic processes in the body.
Causes and symptoms
Symptoms of a pinched nerve in the spine will depend on where the pain is located and which nerve is pinched. If a sensitive nerve is pinched, your back hurts. And if a motor or autonomic nerve is pinched, there may be more dangerous consequences.
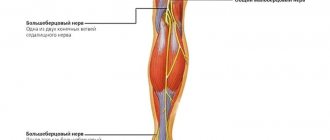
Lumbosacral spine
It is this part of the spine that especially often suffers from pinched nerves. In most cases, the sciatic nerve becomes inflamed. Symptoms of pinched nerves in this part of the spine are as follows:
- piercing acute pain in the lumbar region, radiating to the buttock or thigh; with inflammation of the sciatic nerve, the pain moves to the leg on one side;
- limited motor function;
- weakness in the lower extremities;
- muscle spasms.
The main causes of pinching: heavy physical stress on the spine, including pregnancy or excess weight, malignant or benign tumors, hypothermia.
Cervical region
A pinched nerve in the cervical spine is a rare occurrence. It can be caused mainly by hypothermia or sudden, careless movements of the head. Pain is also possible when staying in an uncomfortable position for a long time (for example, when intoxicated, when a person does not control his movements). Despite its rarity, the consequences of a pinched nerve in this area of the spine can be very dangerous: paralysis, inflammation, neurological problems. The causes of pain in the cervical spine are as follows:
- chronic diseases (osteochondrosis, hernia);
- neoplasms;
- curvature of the back.
Symptoms of a pinched spine are expressed by sharp pain in the neck, radiating to the shoulders and back of the head. It can occur when moving the head. There may be numbness in one or both upper extremities, half of the tongue, or the collarbone. Headaches and tinnitus occur.
Thoracic region
The causes of a pinched nerve in the thoracic spine can be: unsuccessful rotation of the body, heavy lifting, curvature of the spine, age-related changes. Signs of a pinched nerve in the chest can be confused with an attack of angina. Arrhythmia, shortness of breath develop, pain appears in the heart area, and it becomes difficult to breathe. In addition, it causes fever, profuse sweating, redness in the area where the nerve is pinched, difficulty moving, problems and pain in the stomach.
Between the shoulder blades
A pinched nerve between the shoulder blades can occur as a result of various diseases (osteochondrosis, arthritis, arthrosis, intervertebral hernia), tumors, and injuries. Factors in the development of such diseases include: a sedentary lifestyle, too much physical activity, exposure to a draft. Symptoms of a pinched nerve in the spine between the shoulder blades: pain syndrome, pain radiates to the arms, neck, chest, shoulders, and to the heart area. Sometimes possible when breathing or moving. Muscle spasms occur in the area of the shoulder blades. Vertebral pain differs from pain in the heart in that it does not go away in a horizontal position.
Which doctor treats
If painful sensations appear in the joint, we recommend immediately contacting a neurologist or rheumatologist. A traumatologist and orthopedist can also consider such patient requests.
Specialists will carry out diagnostic procedures, including:
- MRI,
- radiography,
- CT.
Additionally, patients may be prescribed an ECG and a blood test so that the doctor has a complete picture of the person’s health status and can consult with doctors of other specializations.
IMPORTANT! Shoulder pain can indicate both neurological problems and injuries to the shoulder joint. In any case, the symptom cannot be ignored, because the consequences of neglect can lead to the development of a serious illness.
Therefore, if you have shoulder pain, make an appointment with our specialist - a neurologist, traumatologist or rheumatologist, who will determine the essence of the problem and prescribe the necessary treatment for you. A consultation with a highly qualified doctor at the Kuntsevo Medical and Rehabilitation Center will help you get rid of shoulder pain and return to your previous high quality of life!
Sign up
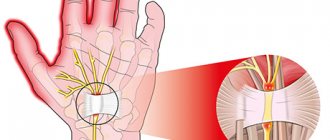
Before treating a pinched nerve in the shoulder joint
Before treating the brachial nerve, it is necessary to find out the cause of its damage. Consistently eliminating all potential causes will result in the compression of the nerve fiber being eliminated. This will lead to a gradual restoration of dystrophically altered fibers. But in some cases, regeneration will require longer treatment.
It is important, before treating a pinched brachial nerve, to conduct a full differential diagnosis. In the case of a traumatic, inflammatory and degenerative process of tissue change, the symptoms will be similar to each other, but treatment methods can differ radically.
Therefore, before treating a pinched nerve in the shoulder joint, you need to consult an experienced doctor. You may also need to take x-rays of your shoulder, elbow, and wrist joints. If this does not allow for an accurate diagnosis, then it is recommended to do an MRI or CT scan. In complex diagnostic cases, as well as in the presence of sufficient indications for surgical intervention, arthroscopy of the shoulder joint is performed. During this endoscopic operation, manipulations can be performed to restore the integrity of damaged tissue.
Treatment methods
To treat shoulder neuralgia, patients are prescribed anti-inflammatory and warming ointments (for example, Finalgon). To enhance the positive effects of ointments, it is imperative to take strengthening B vitamins.
It will not be superfluous to carry out general physical therapy. For these purposes, a person can be prescribed electrophoresis and ultrasound, which help relieve tissue swelling.
Exercise therapy, weights, and acupuncture are other proven options for treating shoulder impingement. In extremely severe cases, the patient may be offered a fixing bandage, which completely eliminates the mobility of the arm.
Please note that the treatment gives a positive result only in initial and moderate severity. Chronic problems with the shoulder joint cannot be treated and the patient can only eliminate and minimize pain syndromes.
Shoulder ligament injuries
Shoulder ligament injuries
A rare group of pathologies. This is the result of great mobility of the joint. It is very difficult to perform movements in the shoulder in a volume that is not provided for by the functionality of the shoulder. In addition, there are many muscles around it that protect the bursal-ligamentous apparatus.
But still, sometimes the ligaments of the shoulder joint are completely or partially torn. Swelling, pain with movement, and deformity appear. Shoulder massage after injury is used to reduce pain, swelling, and also to quickly restore joint function.
In the first days after the injury, the swelling is too pronounced. The pain syndrome is also intense. Therefore, direct impact on the shoulder joint is impossible. Massage the tissue nearby. Preference is given to massage techniques that ensure lymph drainage. As the symptoms decrease, or after the plaster splint is removed, a gentle effect on the shoulder joint itself begins. Gradually the intensity can increase. The massage technique and duration of sessions are determined individually, based on the clinical situation and the patient’s feelings.
Sometimes the acromioclavicular joint is torn or stretched. Most often this is the result of a fall, impact or collision with an object at high speed (hockey, road accident). Complete rupture is very rare; most of the time it is partial. Palpation in the area of the shoulder joint becomes painful. Pain appears or intensifies with every movement.
Purposes of massage:
- relieve pain;
- remove swelling;
- provide good conditions for rapid regeneration of the ligament.
Massage is performed for pain in the shoulder joint already in the acute period of injury. During the procedure, the immobilizing bandage is removed. The impact is on the muscles of the back, chest and forearm. Directly in the problem area, only stroking is used. Over time, it is possible to massage this area more vigorously.
Rehabilitation and recovery
As part of high-quality rehabilitation measures, physical therapy is carried out. It allows you to restore damaged muscle tissue, reduce pain or completely get rid of it when the shoulder joint is pinched.
Patients should engage in therapeutic exercises only under the supervision of a physician in order to achieve the desired result.
It is worth noting that recovery will be positive only with the right combination of exercise therapy, medications and following all the recommendations of the attending physician!
Massage for a dislocated shoulder
Shoulder dislocations account for more than 55% of all dislocations. This is explained by the peculiarities of its anatomical structure. The shoulder joint is very mobile. But such mobility is achieved through its weak stabilization.
Main symptoms of dislocation:
- deformation of the joint as a result of the head of the humerus coming out of the glenoid cavity;
- inability to carry out active movements;
- sharp limitation of passive movements;
- sharp pain that intensifies when trying to move;
- severe swelling.
For the first dislocation, conservative treatment is carried out. It is adjusted and the limb is immobilized. Some patients develop a habitual shoulder dislocation. In this case, surgery is required to improve its stability.
Naturally, massage for a dislocated shoulder joint is not able to either straighten it or prevent repeated dislocations if the articular lip of the scapula is torn off. However, this method allows a person to recover more easily and quickly after reduction. Massage reduces swelling, ensures complete reparative processes, and reduces pain. It is also used after open reduction or surgery performed to treat habitual shoulder dislocation. Gentle effects on nearby tissues begin as early as 3 days after surgery.
Lifestyle
Patients with shoulder neuralgia must necessarily lead an active lifestyle, which allows them to activate metabolic processes in the body. Eat only natural and healthy foods.
Try to give up bad habits and spend more time outdoors. Stressful situations should be kept to a minimum! This will generally strengthen your immune system and get rid of shoulder pain.
You can make an appointment with a neurologist for a fee in one of the following ways:
- calling the clinic,
- order a call back,
- leave a request for an appointment using a convenient form on the website
Preventive actions
As with any pathology, it is much easier to prevent the occurrence of a disease than to treat it. First of all, you should control your weight; you should not allow yourself to become obese. If you have a tendency to be overweight, it is recommended to make an appointment with a nutritionist. He will draw up a sample menu, tell you in detail about the foods that can be consumed and those that are best not to be included in the daily diet.
You should eat foods rich in calcium and potassium. They are involved in cellular metabolism. Their deficiency leads to symptoms of pinched nerves. By introducing foods high in potassium and calcium into the diet, it is possible to restore nerve function. Potassium is found in nuts and fruits (such as bananas), and calcium in greens and dairy products.
It is important to maintain correct posture (keep your back straight). A curved spine leads to back problems and disruption of many internal organs. Experts recommend sleeping on a hard orthopedic mattress (or medium hardness). When working sedentarily, you need to take short breaks - walk around the room for a few minutes.
A sedentary lifestyle negatively affects your health and can lead to pinched nerves. It is important to engage in moderate sports and get into the habit of doing exercises in the morning. Performing exercises aimed at stretching and strengthening muscles and joints is an important preventive measure. The main condition is that they must be selected by the attending physician based on the patient’s physical condition.