Causes of piriformis syndrome
The cause of the syndrome can be various pathological changes in the piriformis muscle - damage, inflammation, fibrotic changes, spasms and an increase in muscle volume. Sometimes intramuscular injections lead to the disease, causing abscesses and the formation of infiltrate.
The main etiological factors of SHM: • Trauma. Piriformis syndrome can be associated with muscle overextension, muscle fiber tears, and fibrosis. In the latter case, the piriformis muscle shortens and thickens. • Post-traumatic hematomas and inflammatory processes – myositis, sacroiliitis, cystitis, prostatitis, endometriosis, prostate adenoma. • Vertebrogenic pathologies. This group includes spondyloarthrosis, osteochondrosis, intervertebral hernia in the lumbar region, spinal and vertebral tumors. As a result of irritation of the fibers of the sacral plexus and spinal roots, a reflex spasm occurs. • Muscle overload associated with prolonged forced position of the lumbopelvic segment. Increased loads occur in cases where, with radiculopathy, the patient tries to take an antalgic position (body position in which pain is minimal). Various sports can cause impairment, including weightlifting and running. • Oncological diseases of the tissues of the sacral region and proximal femur. They cause anatomical changes in structures. Neoplasia can cause spasm of the piriformis muscle. • Asymmetry, which occurs with shortened legs or scoliosis. Sometimes a hip amputation can put the muscle into a permanent spastic state that causes phantom pain.
Preventing piriformis muscle spasm
There are no specific methods for preventing pathology. It is recommended to avoid excessive stress on the muscles and injuries.
It is important to contact a specialist in a timely manner. This will help in the initial stages to diagnose and treat pathologies that can provoke piriformis syndrome.
In addition, following these rules will help prevent the development of the disease:
- avoid hypothermia;
- do not engage in heavy physical labor;
- Do not stay in a position for a long time that reduces pain.
Piriformis syndrome is a fairly serious pathology that causes severe pain. It is caused by a whole complex of factors - increased physical activity, injuries, hypothermia.
Mechanism of development of the syndrome
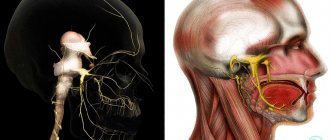
The piriformis muscle (Musculus piriformis) is attached with its narrow end to the greater trochanter of the femur, and its wide end to the sacrum. It is involved in external rotation and during internal hip abduction, passing through the greater sciatic foramen. The inferior gluteal, sciatic, pudendal and posterior cutaneous nerves, gluteal arteries and veins also pass through this opening. This makes piriformis syndrome a disease that requires a comprehensive systemic approach. Persistent contraction of the piriformis muscle reduces the size of the infrapiriformis foramen. This leads to compression of passing vessels and nerves, primarily the sciatic one. Compression impairs the blood supply to the nerve trunk, being an additional pathogenetic component of sciatica.
Osteopathy offers an alternative to classical medicine and complements it, expanding the understanding of the disease. Osteopaths at the Quality of Life clinic can offer a solution to the problem with the piriformis muscle. Painful sensations that do not have a clear localization often arise as a result of spasm of the muscular-ligamentous apparatus, the causes of which are very diverse. When muscles contract, they move internal organs from their place, disrupt their function and cause pain. This is due to tension, compression and twisting of nerve, blood and lymphatic communications.
What it is?
Piriformis syndrome is classified as compression-ischemic tunnel neuropathies . It mainly manifests itself in the form of compression of the trunk of the sciatic nerve, as well as the vessels that are located in it in the region of the infrapiriform space. In this case, the main factor of compression becomes the piriformis muscle itself, which is subjected to spasm.
The infrapiriform foramen is a pair , it is located in the buttocks area and represents the lower part of the larger sciatic foramen of the pelvis. According to its anatomical structure, it has a slit-like shape.
Its boundaries are marked by the sacrotuberous ligament, the lower edge of this muscle and the superior gemellus muscle. Through the infrapiriform opening of the pelvic cavity, the sciatic nerve, posterior cutaneous nerve of the thigh, lower gluteal and pudendal (genital) exit into the deep space of the buttocks.
All of them are located in fascial sheaths, which do not protect against compression under the influence of external factors.
When a muscle is compressed, a spasm is formed , caused by unmotivated tension. It can last from a couple of seconds to several minutes.
If such compression occurs over a long period of time, it leads to a thickening of the muscle belly, and then to a narrowing of the infrapiriform foramen..
When the piriformis muscle spasms, nerves and blood vessels are pinched
The vessels and nerves that are located in it are pressed against the bones and the sacrospinous ligament, which leads to the appearance of adverse symptoms. In this case, compression of the sciatic nerve is manifested to the greatest extent, causing signs of neuropathy that require referral to a specialist.
In a muscle that is in spasm, shortening and thickening are observed, as a result of which the infrapiriform foramen narrows. In addition, other pathological changes occur in the form of multiple microdamages to fibers and accumulation of under-oxidized metabolic products.
These processes stimulate the appearance of a focus of inflammation, lead to increased permeability of small vessels, the development of aseptic inflammation and tissue induration. The aggravation of the pain syndrome is facilitated by the involvement of the pelvic floor muscles, leading to slight dysfunction of the sphincter.
Classification
There are two types of piriformis syndrome in terms of the mechanism of its development:
- primary, arising as an independent phenomenon;
- secondary, in which muscular-tonic syndrome becomes a consequence of the development of other pathologies.
The secondary type of this syndrome occurs in more than 80% of all cases in clinical practice.
Prevalence
Piriformis syndrome is a very common pathology. Almost any person is susceptible to it. The cause may be an unsuccessful injection or the development of pathologies in the pelvic organs. A factor of high prevalence is also the difficulty of diagnosing this disease, which is often not noticed immediately, but at later stages of development.
Classification of piriformis syndrome
Piriformis syndrome has only two forms: • Primary, which occurs due to direct damage. Primary SHM occurs as a result of injuries, myositis, and excess stress. • Secondary. This is the result of prolonged pathological impulses from the sacral or lumbar spine, sacroiliac joint, and small pelvis. Secondary SHM is formed by neoplasms in the spine, pelvic organs and hip joint.
Primary piriformis syndrome is caused by anatomical factors, variations of which may be related to separation of the piriformis muscle or sciatic nerve, as well as abnormal development of this nerve. Among patients with this disorder, less than 15% of cases are due to primary causes. Conventional medicine does not have precise data regarding the prevalence of FMS and does not offer evidence linking the disorder to sciatic nerve abnormalities or other types of sciatica.
The occurrence of secondary piriformis muscle syndrome is associated with the action of aggravating factors, including macro- and microtrauma, long-term accumulation of ischemia and the existence of local ischemia. • The development of piriformis syndrome most often (in about half of all cases) is promoted by trauma to the buttocks, which inflames the soft tissues and causes muscle spasm. This eventually causes compression of the nerve. • Spasms may be associated with muscle shortening caused by changes in leg and lumbosacral biomechanics. This causes compression or irritation of the sciatic nerve. When the piriformis muscle stops contracting normally, it can cause a variety of symptoms in the sciatic nerve area, including pain in the gluteal region and/or the hamstrings, calf, and lateral foot. Microtrauma can be caused by overuse, such as long walking or long distance running, as well as direct compression.
Osteopaths work with the root cause of the disorder, eliminating the problems that caused the development of BMS.
Treatment of pinched piriformis muscle
In most cases, treatment for a pinched piriformis muscle is performed at home on an outpatient basis. This disease extremely rarely requires surgical intervention - only if the canal through which the sciatic nerve passes is completely blocked and its spasm cannot be stopped using conservative methods. In such a situation, it is advisable to perform a surgical operation to restore normal innervation of the lower extremities.
It is advisable to treat pinched piriformis muscle using manual therapy methods. To date, there are no pharmacological drugs that would be able to restore the integrity of damaged muscle tissue, nerve fiber and blood vessels. And with the help of manual therapy, this effect can be achieved.
For example, in our clinic, doctors successfully use various combinations of the following types of effects:
- laser therapy – all scar deformities are eliminated and the elasticity of soft tissues improves;
- osteopathy – enhances microcirculation of blood and lymphatic fluid in the piriformis muscle and improves trophism of all tissues;
- massage – relieves spasm and improves the condition of the sciatic nerve and blood vessels;
- therapeutic exercises and kinesiotherapy allow you to restore the normal structure and performance of the muscle;
- physiotherapy improves metabolic processes at the cellular level;
- acupuncture starts the process of activating the body's hidden reserves for the regeneration of damaged tissues.
If you need treatment for a pinched piriformis muscle, you can make an appointment with a neurologist for free at our manual therapy clinic in Moscow right now.
The role of spasms in the pathogenesis of piriformis syndrome
Spasm is a protective reaction of the body in the form of sustained tension and muscle contraction. It occurs as a response to threats associated with physical influences (blows, pain) or mental stress (fear, anxiety). When the threat passes, the tension gradually subsides, the tone of the muscles and ligaments is restored. However, this does not always happen.
If the muscle is constantly tense, this leads to compression of the vessels of the circulatory and lymphatic systems, because the tissues do not receive the required amount of oxygen and nutrients. As a result, their hypoxia develops and local immunity decreases, which leads to chronic inflammation. With constant stress over several weeks, fibrosis develops - a hardening of the tissue, which is usually accompanied by severe pain. But even at this stage the situation can still be corrected: the osteopath, having worked with the genitourinary system, the lumbopelvic region, and the dura mater, will eliminate spasms of muscles and ligaments and return them to their original tone. However, with very long spasms (more than a year), irreversible tissue scarring processes begin, resulting in ossification (calcification) of the muscle or ligament. Considering that spasm can be caused even by a visit to the gynecologist, not to mention childbirth or abortion, the scale of this problem in women is amazing.
The role of this muscle in ensuring the normal functioning of a woman’s body is great. Spasms and fibrotic phenomena often cause dull aching pain of different localization: • sacral; • lumbar; • gluteal.
They often intensify during squatting. In addition, spasms can be an additional risk factor for the development of a number of other pathologies - in particular, hemorrhoids and arthrosis of the hip joint.
Muscle spasms and fibrosis can also cause difficulties during labor. This is due to the fact that the birth canal fits tightly to the sacrum, so the contractions of the Musculus piriformis play an important role in the birth of the child, pushing and turning the fetal head. If the muscle is fibrotic, the fetal head stands in one position for a long time. This is fraught with damage to soft tissues and a number of other complications.
On the other hand, Musculus piriformis itself is injured during childbirth, which can cause fibrosis in the postpartum period. Therefore, every woman should visit an osteopath before and after childbirth. Voltage is easily determined during examination. Osteopathic techniques gently and painlessly eliminate spasm, and exercise therapy doctors will teach the patient the correct technique of exercises to strengthen the hips, back, buttocks and abs, and normalize the position of the lumbopelvic region.
We have considered only a small part of the situations and problems associated with internal spasms of the piriformis muscle. Each organ is supported by several muscles and ligaments, each of which, in turn, can go into spasm.
Moreover, the consequences are far from limited to pain, but can be much more serious. For example, forced displacement of the uterus during an abortion causes deep spasms of all the ligaments that attach the organ to the skeleton.
Since it does not return to its original anatomical position, sometimes twisting of blood vessels and nerves occurs. In case of a new pregnancy, this can lead to fetal hypoxia and developmental delay.
Osteopathic correction is a soft and delicate effect not only on the source of pain, but also on the true causes of the syndrome. A competent osteopath will help set the body up for self-healing, rehabilitate muscles and internal organs.
Risk factors and causes
Among the factors that provoke the appearance of spasm of the piriformis muscle, there are primary and secondary ones .
| Primary factors include: | Secondary factors in the development of the syndrome are: |
|
|
Among the causes of spasms of the piriformis muscle are::
- vertebrogenic - the development of the syndrome occurs under the influence of damage and tumors on the roots of the spinal cord and spine, as well as lumbar stenosis;
- nonvertebrogenic - the syndrome is provoked by pain caused by pathologies in the internal organs, including myofascial syndrome.
The immediate causes of spasms in the piriformis muscle include:
- staying in one position for a long time, for example, at the workplace, or with unprofessional fixation due to injuries;
The causes of spasm of the piriformis muscle are divided into two types: vertebrogenic and non-vertebrogenic injuries in the lumbar, sacrum or pelvis, which leads to sprains and damage to the piriformis muscle;- sacroiliitis of any origin;
- twisted or obliquely twisted pelvis of various etiologies, developing as a result of different lengths of limbs, scoliosis, pathology in the hip joints;
- overtrained muscles due to irrationally organized and excessive loads, lack of a rest period between workouts;
- myositis ossificans;
- infectious and inflammatory pathologies in the pelvic organs, as well as gynecological pathologies.
Consequences
Due to the fact that spasms of the piriformis muscle are accompanied by overstrain of the pelvic floor muscles, this leads to pinched nerves and blood vessels .
At the same time, the supply of nutrients to this muscle deteriorates, which leads to adverse consequences, in particular increased pain and discomfort during rotational movements of the hips and when bending forward. Excruciating pain also appears in a static position in the hips, groin, lower back, and knee joint.
Video: “Diagnostics of piriformis syndrome”
Symptoms
In approximately 70%, the gluteal-sacral area is affected first. The pain is constant, often nagging and aching. They intensify during walking, squats, and hip adduction. To reduce discomfort, the patient has to spread his legs to the sides. Over time, pain along the sciatic nerve - sciatica - is added to the symptoms. Shooting marks appear running from the foot to the buttocks. In the area where the SGM is located, pain sensitivity decreases and a burning sensation occurs.
Hypotonia of the muscles of the foot and lower leg gradually develops. With total compression of nerve fibers, “dangling foot” may develop. The main manifestations include intermittent claudication, which is a consequence of vascular compression. The same disorder leads to a decrease in leg temperature, pale skin and numbness of the fingers.
Possible risks and complications of piriformis syndrome
Constant debilitating pain reduces the patient's ability to work. It can lead to: • emotional lability; • insomnia; • increased fatigue.
Peripheral paresis of the leg and foot caused by the syndrome develop muscle atrophy. With prolonged progression of the syndrome, the changes become irreversible. Persistent paresis leads to disability. Secondary spasm of the pelvic floor muscles is also possible. This causes discomfort when urinating, dyspareunia (pain during sexual intercourse) in women.
Osteopathic treatment
Osteopathic treatment does not just act on the sore spot, but treats the entire body as a whole; the doctor “listens to the body with his hands.” All organs and systems constantly pulsate, and spasms and tensions distort the picture characteristic of the body of a healthy person. The magnitude of these pulsations is insignificant, but is accessible to the sensitive hands of an osteopath.
Having examined these micropulsations, the doctor determines the cause of the syndrome and eliminates muscle tension. Muscle tissues and ligaments are stretched and relaxed, and the doctor uses gentle movements to move organs and tissues to return them to their normal anatomical position.
Osteopathic correction of the bones, muscles and ligaments of the pelvis, as well as the lumbosacral spine, plays a special role in osteopathic treatment. Soft muscular-fascial relaxation of the Musculus piriformis quickly restores the normal state and eliminates the cause of the syndrome - compression of the sciatic nerve and blood vessels. In especially severe cases, the treatment program is supplemented with drug blockade of the brain.
Symptoms of inflammation of the piriformis muscle on the leg
Clinical symptoms of inflammation of the piriformis muscle are easily recognized. These include the localization of pain in the very center of the buttock, stiffness of movement and the inability to move the leg away from the body in any position (straight, bent, half-bent).
Without timely treatment, inflammation of the piriformis muscle in the leg begins to give a pronounced neurological clinical picture:
- there is a feeling of numbness in certain areas of the skin of the back, side or front surface of the thigh;
- muscle weakness occurs, accompanied by slight twitching;
- at night, cramps may develop in the thigh and calf muscles on the affected side;
- there is a feeling of crawling;
- hyperesthesia occurs;
- characteristic lameness appears.
Then the symptoms of inflammation of the piriformis muscle are aggravated by signs of trophic damage against the background of long-term hemodynamic disturbances. The skin becomes blissful. The skin becomes thinner and is easily injured; scratches and wounds constantly appear, which take a long time and are difficult to heal. The veins become inflamed and blood stagnates in them. Overstretching of the vascular wall and destruction of the venous valves occurs. The development of varicose veins of the lower extremities begins. Against this background, patients develop trophic ulcers.
Impaired blood supply and innervation negatively affects the condition of the muscle fiber. The leg muscles decrease in volume (shrink out) and lose their functionality. Multiple myofascial syndrome may occur, in which absolutely all the muscles on the lower limb on the affected side hurt.
If such clinical symptoms appear, you should immediately consult a doctor. The consequences of untreated inflammation of the piriformis muscle are always negative. If no therapeutic effect is provided, the muscle fibers become deformed and scars form inside them. Due to this, the piriformis muscle completely covers the sciatic foramen. The process of death of the sciatic nerve begins. For the patient, this is fraught with complete loss of ability to work. Degeneration of the cartilage tissue of large joints of the lower limb on the affected side gradually occurs. 2-3 years after suffering and untreated inflammation of the piriformis muscle, a person may develop a severe degree of deforming osteoarthritis of the knee, hip and ankle joint.
Diagnostics includes a number of measures that allow us to determine the cause of inflammation. The patient is prescribed an X-ray of the lumbosacral spine, hip and knee joint. Plantography is performed to exclude the development of flat feet or club feet. It is recommended to do an ultrasound of the internal organs of the abdominal cavity and pelvis. In complex diagnostic cases, CT and MRI examinations are prescribed.
Exercise therapy in the treatment program
After the acute pain syndrome is relieved, the results of osteopathic treatment are consolidated with the help of physical therapy. This allows you to avoid re-exacerbation of the syndrome. Exercises are performed under the guidance of an instructor. The program includes the implementation of special complexes aimed at strengthening: • the muscular corset of the lower back; • buttocks; • lower extremities. Work is also carried out with other parts of the musculoskeletal system.
Treatment of BMS is not aimed at relieving symptoms, but at eliminating the root cause of the syndrome. Therefore, any pain relief without treating the provoking factor is pointless. The exercises that are prescribed to patients are aimed at fully relaxing the muscular-ligamentous system, as well as activating antagonists in the movement of the lumbosacral region
Read also
What is spondylosis deformans? Spondyloarthrosis? Spondylolisthesis?
These questions may arise in a patient's mind after a magnetic resonance imaging (MRI) scan of the spine is performed.
These terms are often used in the MRI report. Are these conditions independent diseases... Read more
Sciatica
Lumboischialgia is pain in the lower back, which is reflected in the buttock, thigh, lower leg, or simultaneously covers the entire lower limb. This is a symptom complex that occurs when there is a disease in the lower back,…
More details
Sacralgia/pain in the sacrum
Sacralgia is pain in the sacrum, which is localized in the lower back. Causes of sacralgia/pain in the sacrum The causes can be varied, to such an extent that the doctor must...
More details
Cervical osteochondrosis
Cervical osteochondrosis is very common in patients aged 25-45 years. With this disease, irritation of the nerve emerging from the intervertebral foramen occurs, which causes pain in the neck muscles,…
More details
Cervicalgia
Many people experience neck pain, or cervicalgia. Everyone has experienced cervical pain at least once in their life, which is pain localized in the neck, not spreading to other areas...
More details