Reasons for the development of neuralgia
The development of neuralgia in certain nerve fibers is due to their anatomical features. Thus, pathological lesions often develop in nerves that pass through narrow channels and openings.
Essential (primary) neuralgia develops for no apparent reason; clinical examination in this case does not reveal other diseases. It is believed that the cause of essential neuralgia may lie in the pressure that is exerted on the nerve fibers by the vascular arteriovenous connections.
Symptomatic (secondary) neuralgia is caused by systemic pathological processes, such as multiple sclerosis. In multiple sclerosis, the myelin sheath surrounding the nerve fiber is destroyed. The myelin sheath ensures the conduction of nerve impulses and protects the nerve fiber. Further destruction of the nerve fiber occurs. Neuralgia can also be caused by a growing tumor compressing the nerve fiber or a traumatic lesion.
Symptoms of neuralgia
Pain associated with nerve damage is characterized as shooting, burning, piercing.
With neuralgia, sensations are one-sided (trigeminal neuralgia, intercostal neuralgia, etc.)
The pain is paroxysmal, severe, always directional (from one area to another). Sudden pain forces the patient to freeze in one position and remain in it until the pain subsides (from several seconds to minutes).
Disorders of tactile, thermal and other types of sensitivity along the affected nerve: severe pain can occur at the slightest touch, “goosebumps” and unpleasant sensations on the skin without any influence, etc.
Muscle weakness in the area of the affected nerve (facial nerve neuropathy).
Spasms and painful tics (with trigeminal neuralgia).
Symptoms of neuralgia
Neuralgia is characterized by sudden, paroxysmal, piercing, “shooting” pain. Pain syndrome may be accompanied by changes in the color and temperature of the skin in the affected area, as well as local muscle cramps.
Most often, patients suffer from trigeminal neuralgia and intercostal neuralgia.
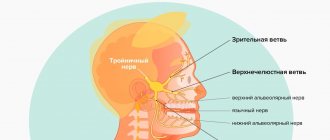
Trigeminal neuralgia is characterized by unbearable pain in the face, gums, and lacrimation. Painful attacks are provoked by talking, chewing, brushing teeth, shaving, and low ambient temperatures. At the same time, redness of the face and spasm of facial muscles occur. Trigeminal neuralgia is characterized by the presence of trigger zones - areas of the skin, touching which can provoke a painful attack.
When examining patients, it is important to exclude all possible secondary variants of trigeminal neuralgia.
With the development of intercostal neuralgia, patients complain of severe pain in the ribs, aggravated by coughing or sneezing. It has been noted that intercostal neuralgia often accompanies osteochondrosis of the thoracic spine.
Postherpetic neuralgia
Chicken pox
Herpes
2422 September 17
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Postherpetic neuralgia: causes, symptoms, diagnosis and treatment methods.
Definition
Postherpetic neuralgia is pain or abnormal sensory sensations associated with damage to the nervous system by the varicella zoster virus.
Causes of postherpetic neuralgia
After suffering from chickenpox (chickenpox), the human herpes virus type 3 - Varicella zoster virus
-
from rashes on the skin and mucous membranes can move to the sensory ganglia (nodes consisting of a cluster of neurons) of the spinal nerves of the thoracic, lumbar or trigeminal levels nerve.
There, the virus is able to remain in a latent (inactive) state for decades. When immunity is reduced (for example, against the background of viral diseases, chemotherapy, cancer, therapy with glucocorticosteroid hormones for systemic connective tissue diseases (rheumatic diseases)), the virus can be activated and cause the development of herpes zoster (herpes zoster )
or trigeminal neuralgia.
The disease begins with one-sided pain, a burning sensation, increased skin sensitivity, after which, sometimes after 1-2 weeks, redness appears, and then blistering rashes on the skin. In 50% of patients, the rashes are localized on the torso (usually along the intercostal spaces at the level of the thoracic spine, sometimes in the lumbar region, sacrum), in 20% - on the head (if the trigeminal nerve is damaged, damage to the eyes and ears is possible), in 15% - on the arms, and 15% - on the legs. In most cases, over time, the pain goes away on its own - recovery occurs after 2-3 weeks, but sometimes (in about 20% of patients) a complication of herpes zoster develops - postherpetic neuralgia.
Postherpetic neuralgia is rarely seen in children and young adults, but its incidence increases significantly in old age.
The real prevalence of postherpetic neuralgia is unknown, since there is no consensus on the time interval between rashes, the onset of pain and the duration of the pain syndrome.
Classification of postherpetic neuralgia
A number of authors propose to distinguish three temporary phases of pain associated with Herpes zoster
.
- Acute herpetic neuralgia, in which pain lasts up to 30 days from the onset of the rash.
- Subacute herpetic neuralgia, lasting 30-120 days after the onset of the rash.
- Postherpetic neuralgia, in which pain persists more than 120 days after the onset of the rash.
Most patients recover completely within one year after the onset of pain, but for some, pain persists for years.
Symptoms of postherpetic neuralgia
The main complaint of patients is pain. It is characterized by varying intensity and frequency - from mild to extremely painful, from short-term to permanent. With herpes zoster, pain can spread beyond the localization of the rash. In the clinical picture of postherpetic neuralgia, the following types of pain can be distinguished:
- constant pain, which patients describe as dull, pressing or burning;
- paroxysmal (paroxysmal) pain that occurs suddenly, sharp, shooting, piercing;
- Allodynia is pain that occurs in response to even very mild stimuli that under normal circumstances do not cause pain, for example, a light touch with a cold hand.
Patients often report constant fatigue, lack of appetite, decreased mood, and sleep disturbances.
Some patients complain of intense itching, which is usually localized in the head and neck area.
Diagnosis of postherpetic neuralgia
At the onset of herpes zoster, when patients are only concerned about pain, the doctor may suspect heart disease, intercostal neuralgia, or osteochondrosis. However, with the appearance of rashes, the diagnosis becomes obvious.
The persistence of pain after the rash resolves indicates postherpetic neuralgia.
Instrumental and laboratory diagnostics, as a rule, are not carried out.
In atypical cases, a serological test 256 may be prescribed in combination with test No. 257 (IgM antibodies) to diagnose chickenpox. In addition, these studies may be needed to assess immunity to the virus.
Treatment of neuralgia
For primary neuralgia, the administration of B vitamins, novocaine injections, and vascular drugs is indicated.
Treatment of secondary neuralgia should be aimed at eliminating the cause that caused the damage to the nerve fibers.
Anticonvulsants are used in the treatment of trigeminal neuralgia. This group of drugs has a pronounced analgesic effect.
In some cases, if indicated, it is possible to perform neurosurgical intervention - vascular decompression.
Symptoms of intercostal neuralgia
The main symptom of intercostal neuralgia is pain along the intercostal space. The intensity of pain can vary: from sharp, acute, severe, shooting (more often) to constant, medium intensity. The pain intensifies when the patient moves, when coughing and sneezing, and even when breathing. Often a person takes a forced position: leans towards the affected side in order to minimize the range of movements in it. Some patients, when coughing, laughing or sneezing, press their palm firmly against the affected intercostal space for the same purpose: to reduce the range of movements in this area so that it hurts less.
When the intercostal nerve on the left is damaged, the pain often imitates the sensations of angina pectoris: patients evaluate the pain as burning, with irradiation (spread) to the left arm, scapula, and spine. However, angina pain still does not depend on movements, coughing, laughter, etc., and, moreover, decreases after the patient takes nitroglycerin tablets or its analogues. However, in order not to miss such an important cardiac pathology, in doubtful cases the doctor prescribes an ECG for the patient. It is important not to confuse intercostal neuralgia with myocardial infarction, because the pain with it is also not reduced by nitroglycerin. Therefore, if pain suddenly arises in the heart area, you should not tempt fate, hoping for the best, but you need to play it safe: call an ambulance and undergo an electrocardiogram.
Differential diagnosis based on clinical manifestations is an important step in the treatment of patients. First of all, it is necessary to exclude heart pathology, since the treatment of intercostal neuralgia and heart diseases require different methods of therapy, and incorrect diagnosis and lost time in case of cardiac pathology can be decisive for the patient’s condition. The differences are primarily that:
- with neuralgia, chest pain persists for a long time, both day and night;
- the pain intensifies when changing the position of the body in space, coughing and sneezing, deep inhalation and exhalation, sudden movements, when palpating or squeezing the chest.
In case of heart disease, in particular angina pectoris, the resulting pain quickly passes after 5-10 minutes or is relieved by taking nitroglycerin. Movements and changes in body position, coughing and deep breathing do not cause increased heart pain, but may be accompanied by disturbances in heart rhythm and changes in blood pressure. To exclude the possibility of cardiac pathology in the presence of pain in the chest or under the left shoulder blade, it is necessary to urgently perform an electrocardiogram, and sometimes an x-ray.
Neuralgia: symptoms, treatment
Neuralgia is a lesion of a certain nerve, which is a structural unit of the peripheral nervous system. There are several types of neuralgia, but they are all united by the nature of the pain syndrome when affected. The pain is “shooting”, “burning” in nature and spreads along the anatomical course of the nerve.
The most common causes of neuralgia are injuries, inflammatory diseases, poisoning with alcohol, drugs, medications, and circulatory disorders at the location of the nerve.
Neuralgia symptoms:
The main symptom of neuralgia is pain, which can be paroxysmal or constant. Most common:
- Trigeminal neuralgia is a paroxysmal unbearable pain in the face along one of the branches of the trigeminal nerve (there are 3 of them). Simultaneously with the pain, it manifests itself as thyroid movements of the facial muscles, profuse lacrimation, redness of the facial skin;
- Intercostal neuralgia is pain in the chest area along the ribs. Intensifies with movement, breathing, sneezing. The cause of its appearance is Dorsopathy of the thoracic spine, spinal injuries, cancer, pneumonia;
- Neuralgia of the external cutaneous nerve of the thigh - pain is localized along the outer surface of the thigh, intensifies when touching clothing;
- Neuralgia of the glossopharyngeal nerve (the nerve that innervates the tongue and pharynx). Attacks of pain occur in the throat, radiating to the ear and lower jaw. Intensifies when swallowing, chewing;
- Occipital neuralgia is the most common neuralgia. It is characterized by a headache in the back of the head, radiating to the temporal region. Considering the anatomical location of the vessels of the neck, when turning the head to the sides, it is accompanied by dizziness and nausea;
- Neuralgia of the sciatic nerve is characterized by pain, limitation of movements, decreased sensitivity along the back of the leg. The reason is the presence of protrusions and hernias in the lumbar spine.
Treatment:
Treatment of neuralgia of any localization should be prescribed by a doctor. Treatment will only be effective when the entire range of drugs is prescribed, aimed at eliminating the cause of pain and taking into account concomitant diseases. The course of treatment is prescribed individually to each patient. In severe cases of neuralgia, surgical treatment is recommended.
Take care of your health!
Make an appointment with a neurologist
Neurologist - Skvortsova Zinaida Nikolaevna
You can make an appointment by calling (391) 205−00−48 or through your personal account
Symptom of proctalgia
Proctalgia (pain in the rectum) is characterized by an unexpected appearance, usually at night, lasting about 15-30 minutes, after which a period of relief begins. There may be quite long intervals between such attacks. In some cases, the pain is accompanied by cramps in the intestines. Pain in the perineum in men can provoke the development of priapism (pathological persistent painful erection). Sometimes sexual intercourse provokes an attack of anorectal pain. Often the acute period of anococcygeus pain syndrome is associated with the presence of general neurovegetative symptoms - sweating and pallor of the skin.
The location of coccydynia is the coccyx area, the severity of pain increases when pressing on it or when walking. Often, determining the location of pain is quite problematic and difficult to diagnose, while patients complain of pain in the rectum, discomfort, burning sensation and heaviness in the coccyx area.