Stroke, or apoplexy, is a condition associated with disruption of the normal functioning of the vascular system of the human body. It is also called a disease, although, in fact, a stroke is precisely an acute condition, a pathological disturbance of blood circulation in the brain. This pathology is characterized by the sudden appearance of certain neurological symptoms, which may have a focal distribution or affect the entire organ. The clinical picture of symptoms lasts up to several days, gradually disappearing, or causes the death of the patient in a short time if he was not provided with medical assistance.
Stroke is a disease that is in second place as a cause of mortality among all pathologies of the cardiovascular system, immediately after coronary heart disease.
Causes of formation and mechanism of development of pathology
Content:
- Causes of formation and mechanism of development of pathology
- Types of brain strokes
- Symptoms and signs of stroke: clinical picture
- Stroke: how to recognize and determine brain damage
- First aid for stroke: algorithm of actions
Brain damage due to stroke, today, is one of the most common causes of disability in the population - this is evidenced by data from the World Health Organization. Approximately 70-80% of people who have suffered a stroke become disabled, of which 20-30% require constant outside care.
Men and women are susceptible to the development of pathology approximately equally, and the likelihood of a stroke increases as a person reaches the age of 30-35 years and older.
Why might a stroke develop? The general principle of the development of pathology is the presence of disturbances in the functioning of the vascular system, which directly affect blood circulation in the brain. A significant role in the development of stroke is played by factors such as arterial hypertension, vascular atherosclerosis, coronary heart disease - against the background of these diseases, apoplexy can develop if this is facilitated by poor nutrition, smoking, alcohol consumption, frequent stress, taking hormonal contraceptives, and dyslipidemia. Moreover, stress and the use of contraceptives negatively affect the female body. Obesity is also dangerous for women; for men, the problem of alcoholism is more pressing. Family members with a history of strokes also increase the likelihood of brain damage.
As for the mechanism of development of strokes, each of the types of pathology known to medicine is formed differently. Thus, ischemic and hemorrhagic stroke are characterized by fundamentally different mechanisms of occurrence. The ischemic type of damage occurs approximately 4 times more often than hemorrhagic.
Ischemic stroke is also called cerebral infarction - it develops as a result of obstruction of the patency of the cerebral arteries. Due to insufficient blood supply, a person experiences prolonged cerebral ischemia, after which irreversible changes begin in the tissues of the organ, affecting the blood exchange zone of the affected artery.
A hemorrhagic stroke is formed according to a slightly different pattern - as a result of an atraumatic rupture of a cerebral vessel, hemorrhage occurs in the brain tissue.
Ischemic strokes are more common in people over the age of 55, while the hemorrhagic type of pathology also occurs in younger people.
Types of brain strokes
All manifestations of pathology, its characteristic signs, pathogenesis and etiology determine the division of the concept of “stroke” into several types:
- ischemic;
- hemorrhagic;
- lacunar;
- extensive;
- spinal;
- spicy;
- repeated.
What is ischemic stroke
This type of lesion is formed as a result of an obstruction in the flow of blood through the blood vessels in the brain. In this case, the intracranial and extracranial vascular subsystems may be affected. So, in 30% of cases of ischemic stroke, it develops due to occlusion of the carotid arteries.
A sharp deterioration in blood supply can occur due to the presence of vascular spasm and thromboembolism. The formation of emboli occurs against the background of pathologies in the heart:
- after a heart attack;
- with atrial fibrillation;
- due to acquired or congenital heart valve defects;
- with myocarditis, endocarditis;
- for rheumatism.
Blood clots that form in the heart area, due to the blood flow, move into the cavity of the cerebral vessels, clogging them. In this case, a part of an atherosclerotic plaque that breaks away from the vascular wall can act as an embolus. Getting into a narrow cerebral vessel, it provokes its occlusion.
What pathogenetic types can an ischemic stroke have? Doctors highlight:
- cardioembolic, which is formed due to cardiac arrhythmia, the presence of valve disease, or a previous heart attack;
- atherothrombotic: its root causes are atherosclerosis of large arteries and arterio-arterial embolism;
- lacunar: develops due to occlusion of small arteries;
- of unknown origin, which include pathologies with an unknown cause of occurrence, when an accurate diagnosis cannot be established.
More rarely, another type of ischemic apoplexy occurs, caused by hypercoagulation of the blood, non-atherosclerotic vasculopathies, and dissection of the arterial wall.
Periods of development of ischemic type of brain damage
Ischemic stroke can occur due to the following diseases:
- atherosclerosis;
- amyloidosis;
- collagenoses;
- systemic vasculitis;
- angiitis;
- drug addiction.
The normal course of the disease involves a person going through several periods:
- acute, which is observed in the patient during the first three days. In this case, the first five hours are considered the so-called “therapeutic window”, during which it is advisable to use thrombolytic drugs;
- acute, which lasts up to 4 weeks after the attack;
- early recovery – up to 6 months;
- late recovery – about 2 years after the onset of pathology.
After the rehabilitation period ends, the residual effects of a stroke can manifest themselves throughout the rest of their lives.
Hemorrhagic stroke: what is it, why does it appear?
This type of brain damage is associated with diffuse or isolated cerebral vascular pathology. The vascular wall becomes thinner and loses elasticity.
Often hemorrhagic stroke occurs against the background of uncorrectable arterial hypertension, hypertensive crisis. With a sharp increase in pressure, the pressure on the wall of the vessel increases - it bursts. Blood flows into surrounding tissues.
Provoking moments are:
- stress;
- lack of sleep;
- hyperthyroidism;
- pathology of the adrenal glands.
Other factors that provoke the appearance of pathology are developmental anomalies and arteriovenous malformation of the brain. This process leads to the formation of an aneurysm, that is, a protrusion of the arterial wall. At this point, the vascular wall becomes very thin and therefore easily ruptures due to increased blood pressure.
Hemorrhagic strokes can occur due to blood clotting disorders, as well as with inadequate drug therapy, which affects coagulation parameters.
It is considered the most severe form of stroke - death occurs in approximately 70% of all cases.
The following stages of formation of hemorrhagic strokes are distinguished:
- ruptures in the walls of blood vessels lead to the accumulation of a blood clot and the formation of necrosis in the tissues;
- a hematoma forms, which mechanically compresses the brain tissue;
- an ischemic zone is formed in the compressed area;
- the combination of hematoma and ischemia triggers a chain of irreversible processes of brain damage in the organ;
- under the pressure of a hematoma, areas of the brain can shift, which is a life-threatening condition.
Characteristics of other types of strokes
Extensive
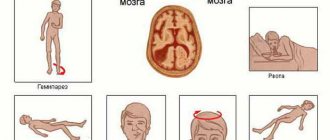
This category characterizes the so-called massive strokes - severe lesions with pronounced cerebral manifestations:
- depressed state of consciousness;
- swelling of the brain;
- paresis of gaze towards the paralyzed side of the body;
- hemiparesis;
- speech disorder;
- loss of part of the visual field;
- vegetative disorders;
- trophic disorders that occur after a year or two on the affected side;
- changes in pupil size, weakening of the pupil's reaction to light;
- squint.
In addition, the patient experiences spasms of the tonic muscles. The extensor muscles may experience a marked increase in tone.
A major stroke is a lesion that often leads to a person’s death or complete disability.
Lacunar
It is classified as a separate variety. During the process of life and development, a person develops a limited lesion of the perforating arteries of the brain - small vessels (up to 2 millimeters in diameter, no more than 10 centimeters in length). They connect larger vessels to each other. At the site of the infarction, a round-shaped cavity appears, which contains cerebrospinal fluid. The lacunar variety represents approximately 30% of all ischemic strokes. It is characterized by:
- impaired body coordination on one side;
- impaired clarity and intelligibility of speech;
- disappearance or impairment of motor activity of one arm or leg.
The most common cause of this type of lesion is a combination of atherosclerosis and high blood pressure. In addition, a lacunar stroke can be of an embolic nature - such a pathology is more difficult for the patient, since a significant area of the brain is involved in the damage mechanism.
Spinal
It is a circulatory disorder in the spinal cord, which is formed against the background of a typical cerebral stroke or an infectious process, tumor, metastases, or autoimmune diseases. Spinal stroke is usually localized in the cervical or lumbar enlargement, namely in the large-diameter arteries, as well as in the small reticulomedullary arteries. This type of damage most often occurs in older people, whose body has difficulty coping with the condition of impaired blood supply to the brain.
How to determine the formation of a spinal type of pathology in a person? Doctors pay attention to the presence of such signs:
- unexplained pain in different parts of the body;
- chronic spinal insufficiency;
- severe pain in the head that is constant;
- the presence of noise and a feeling of heaviness in the head;
- loss of consciousness when trying to get up;
- feelings of dizziness;
- memory loss;
- increased fatigue;
- sleep disorders.
A person feels numbness in his legs due to long walking, but there is no pain in his limbs. The discomfort disappears after rest.
Spicy
Acute stroke is the initial period of development of a pathological condition. On average, it lasts for three weeks. The patient experiences an increase in the pathogenetic process in the brain, especially in the first 6 hours.
Acute stroke goes through several stages:
- after damage to organ cells, the nucleus of a brain infarction is formed;
- the area of metabolic changes around it increases (by about 80% in 6 hours);
- the beginning of the death of organ cells (necrosis);
- spread of neurological disorder in the form of generalized and focal manifestations.
Repeated
Appears due to cerebrovascular diseases, dementia disorders, against the background of impaired heart rhythm, arterial hypertension, diabetes mellitus, after a previously diagnosed stroke of the brain.
Emergency help
The stable functioning of brain structures is ensured by metabolic processes characterized by high speed. Irreversible changes in the affected area during a stroke occur due to a violation of their mechanism. The area affected by a stroke is outlined by a penumbra formed by cells that can be restored with adequate and modern therapeutic measures. The patient’s quality of life and the effectiveness of rehabilitation measures depend on how successfully first aid is provided.
It is possible to restore the functioning of some cells within 4 hours after the first signs of an acute disorder appear. At the moment, the support of loved ones and relatives is of particular importance, since patients often do not realize the events happening to them. When symptoms of a stroke appear, loved ones should not only call an ambulance, but also provide first aid, regardless of where the person is: at home or on the street.
First aid for hemorrhagic and ischemic stroke involves performing the same actions. After calling an ambulance, it is important to understand whether the person is conscious, since with severe lesions, patients fall into a coma; epileptic seizures and stupor are also possible. If there is no response, it is important to periodically bring the patient to consciousness, as well as ensure his safe placement.
Another vital point is to check the person's heartbeat and breathing. In some cases, the patient’s life can be saved by resuscitation measures carried out before the doctors arrive. If a person breathes on his own and his heart is beating, then he should be laid on his back or side, to ensure air flow, his neck and chest should be freed from constricting clothing and accessories.
When a patient wears removable dentures, they should be removed from the oral cavity. Vomiting during stroke is common and can obstruct the airway, so it is important to remove the vomit while the patient is unconscious.
The next step in first aid is to check the blood pressure level, if it is elevated, you should not give the person water or any medications. Before doctors arrive, paralyzed limbs should be massaged and the person covered with a blanket.
The participation and care of people around you can save a person’s life. The adequacy and efficiency of first aid provided determine the effectiveness of subsequent treatment and rehabilitation measures. After the ambulance arrives, the patient is hospitalized in a medical facility equipped to combat the consequences of a stroke.
Symptoms and signs of stroke: clinical picture
All clinical manifestations of pathology are divided into several groups:
- general cerebral;
- meningeal;
- focal.
The hemorrhagic variant of the pathology has a characteristic manifestation, rapidly progressing course. The ischemic type of lesion develops somewhat more slowly.
The first thing that can be noticed in a victim with ischemic pathology is focal manifestations, while general cerebral symptoms are less pronounced, and meningeal symptoms are often absent. In hemorrhagic stroke, it develops according to a different pattern - general cerebral manifestations debut, then focal symptoms increase. Meningeal syndrome is characteristic of subarachnoid hemorrhage, localized between the pia and arachnoid membranes of the brain.
Typical manifestations of cerebral damage in hemorrhagic stroke:
- headache;
- nausea and vomiting;
- state of stupor, clouding of consciousness;
- coma.
10% of those affected may develop an epileptic attack. Due to increasing swelling of the brain, a person develops severe intracranial hypertension, dislocation syndrome and compression of the brain stem may develop.
Focal symptoms manifest themselves in different ways, depending on the location of the lesion. If hemorrhage occurs in the carotid arteries, a person experiences a complete loss of muscle tone on one half of the body and the appearance of pathological foot signs.
The facial muscles in the half that corresponds to the immobilized half of the body are paralyzed. A person develops a distorted facial expression, the corner of the mouth droops, and the nasolabial fold smoothes out. An attempt to smile will immediately reveal that the damaged side lags behind the healthy one, or it may remain motionless, resulting in a lopsided grin. It is also impossible to raise both eyebrows.
Limbs with reduced muscle tone lose sensitivity. Both eyes lose half of the visual field. The patient may experience visual hallucinations and photopsia, visuospatial agnosia. It should be noted that the half of the body and face in which such signs are noted is often opposite the damaged half of the brain.
A stroke in the vertebrobasilar region of the cerebral vascular system is accompanied by dizziness, vestibular ataxia, diplopia, visual field defect of the eyes, cerebellar ataxia, hearing impairment, dysphagia, and dysarthria. The patient cannot move his eyeballs normally.
Stroke: how to recognize and determine brain damage
Doctors emphasize that in the first three to six hours after the onset of hemorrhage, the most effective treatment and removal of a person from a fatal condition is possible. Every second counts, and this is not an exaggeration - this is why it is very important to know and be able to determine whether a person is having a stroke in order to immediately take him to the hospital or call an ambulance.
The following sensations and complaints should raise suspicion:
- sudden weakness in the limbs;
- numbness in the arm and leg on one side;
- severe speech impairment;
- confusion or loss of consciousness;
- impaired perception of the speech of people around;
- loss of coordination, balance;
- feeling dizzy;
- sharp and sudden headache after a stressful condition or severe physical exertion;
- numbness of the lips, half of the face, distortion of the facial muscles;
- violation of pressure indicators - a sharp decrease or increase.
What should you do if the person next to you becomes ill, and how can you tell if he is having a stroke? There are 4 tips that help to almost accurately determine that a deterioration in well-being occurred precisely against the background of this pathology:
- Ask him to smile - if he has been struck by a stroke, the patient will not be able to do this or he will have a crooked grin on one side, while the second corner of his mouth will remain motionless or will react inhibited.
- Ask to answer a simple question - what day is it today or what is his name. A person will not be able to pronounce a simple sentence of several words, his speech will be slowed down, words and letters will change places. Or there will be no response to the request at all.
- The patient is asked to raise both arms up - he will also not be able to do this, his arms will only rise partially. There is muscle weakness on the affected side.
- Ask to stick out your tongue. If it is curved, then this may be a sign of pathology.
If a person suspected of having a stroke has problems performing at least one of the simple tasks listed, he urgently needs to be taken to the hospital, or call an ambulance.
Other obvious symptoms that the victim complains about are severe headaches, the appearance of flashing “spots” before the eyes, numbness of the limbs and loss of sensitivity. The person should be asked to move their left and right limbs together; they will likely find it extremely difficult to do so.
Nausea, vomiting and dizziness are common; vision disappears, coordination of movements is impaired. The patient cannot stand on his feet, falls, and loses consciousness.
What to do before the ambulance arrives?
Don't just stand there until the ambulance arrives. First of all, you need to put the person on a flat surface in a horizontal position. If a person has fallen, then you just need to give him a more comfortable position. It is important to control your breathing. If it is completely absent, place the person on his side, clean the oral cavity of food debris, vomit or dentures. They can be a barrier to normal breathing. To make breathing easier, you also need to unbutton your blouse or other tight items. It is advisable to loosen the belt. Open a window and allow fresh air to flow.
what to do before the ambulance arrives
If you have a tonometer at hand, you should immediately measure your blood pressure and record the readings. With high pressure, you need to raise your head, and with low pressure, you need to raise your legs. If a person has convulsions, under no circumstances should you try to restrain the person. Just put something soft under your head to avoid injuring your head. The only thing worth doing at the end of a seizure is to turn the person on his side.
It is strictly forbidden to unclench your jaw, try to insert any objects into your mouth, or fix your tongue. Such actions will only lead to harm to the person providing assistance. You should not worry about asphyxia through tongue swallowing; this is not possible during a convulsion.
If breathing and heartbeat stop, CPR should be started immediately. All resuscitation actions must be performed until the ambulance arrives.