Concussion is one of the most common diagnoses in pediatric traumatology. Overall, traumatic brain injury (TBI) ranks first among all childhood injuries requiring hospitalization. Approximately 120 thousand children with concussion are admitted to Russian hospitals every year.
According to the severity, traumatic brain injury is divided into mild (concussion), moderate (mild to moderate brain contusion, with possible fractures of the cranial vault) and severe (severe brain contusions, intracranial hematomas with compression of the brain, fractures of the base of the skull). Fortunately, up to 90% of childhood TBIs are concussions, which is what this article will discuss.
The high level of injuries in children is explained by the child’s increased motor activity, restlessness and curiosity, which is combined with imperfect motor skills and coordination of movements, as well as a reduced sense of danger and fear of heights. In addition, in young children, the head has a relatively large weight, and the skill of belaying with hands has not yet been developed, so small children, as a rule, fall upside down and do not use their hands.
The causes of childhood TBI are very specific to each age group. Newborns in the total mass of victims make up 2%, infants - 25%, toddlers - 8%, preschool children - 20% and school-age children 45%.
Injuries in infants are primarily the result of the inattention and carelessness of their parents. Children under 1 year of age most often (more than 90%!) receive head injuries after falling from changing tables, beds, from parents' arms, from strollers, etc. You should never leave your baby alone in a place where he could fall. If you need to move away from your child at a distance greater than an outstretched hand, do not be lazy, put him in a crib, in a stroller with sides, in a playpen! One or two seconds is enough for the baby to roll to the edge of the changing table and fall.
From 1 year
babies begin to walk. The main cause of TBI is a fall from one’s own height, and a little later - falls from stairs, trees, roofs, windows, slides, etc. The episode of TBI itself is not always possible to identify. It should be borne in mind that if the child remained under the supervision of relatives, neighbors or a nanny, then they can hide from the parents the fact that the baby fell.
Older children
For various reasons, they themselves often hide the trauma.
In addition, children may experience brain damage without direct head trauma. These injuries usually occur when a child's body is subjected to sudden acceleration or deceleration (shaken baby syndrome). “Shaken baby” syndrome is most often observed before the age of 4-5 years
and can occur with rough handling, jumping from heights, and in young children even with excessively intense rocking.
Manifestations of a concussion
With a concussion, there are no gross, irreversible changes in the brain, and such an injury, being the most common, has the best prognosis and very rarely leads to complications.
It should be remembered that the brain of a child (and especially an infant) is significantly different from the brain of an adult. The course of a concussion in adults differs significantly from the course of this injury in a child.
In adulthood, a concussion is manifested by the following main symptoms: an episode of loss of consciousness from a few seconds to 10-15 minutes; nausea and vomiting; headache; amnesia (loss of memory) of events associated with the trauma (before the trauma, the trauma itself and after the trauma). In addition, some specific neurological symptoms are detected, such as nystagmus (twitching of the eyeballs), impaired coordination of movements and some others. The picture of a concussion in a child is completely different.
In children under 1 year
A concussion, as a rule, is asymptomatic. Loss of consciousness often does not occur; single or repeated vomiting, nausea, regurgitation during feeding, pale skin, causeless restlessness and crying, increased drowsiness, lack of appetite, and poor sleep are noted.
In preschool
More often it is possible to establish the fact of loss of consciousness, nausea and vomiting after injury. They experience headaches, increased or slow heart rate, instability of blood pressure, pale skin, and sweating. In this case, moodiness, tearfulness, and sleep disturbance are often noted.
Sometimes children experience a symptom such as post-traumatic blindness. It develops immediately after the injury or a little later, persists for several minutes or hours, and then disappears on its own. The reason for this phenomenon is not completely clear.
The characteristics of a child’s body lead to the fact that a long-term state of compensation can be replaced by a rapid deterioration of the condition. That is, immediately after the fall the child feels satisfactory, but after a while symptoms appear and begin to rapidly increase.
Which doctor should I contact if I have a concussion?
Let's figure out which doctor to go to if you have a concussion. After a concussion, even a mild one, you must see a doctor whose activities are in one way or another related to head injuries.
Surgeon
Sometimes a traumatic brain injury can be accompanied by additional bodily injuries: fractures, dislocations, cracks in the bones of the skull, bleeding. In this case, especially if emergency surgery is required, the traumatologist will send the patient to the general surgery department. In all other cases, consultation with a surgeon is usually not required.
ENT
an otolaryngologist if there is bloody discharge from the ear or tinnitus continues for more than a day .
If you have nosebleeds or suspect a septal injury after a blow or fall, you should also seek advice from an ENT specialist.
Oculist
With a traumatic brain injury, contusion of the eyeball can occur.
If, after a diagnosed injury, you experience pain in the eyes, severe nausea, dizziness, redness of the eye, obvious decreased vision, fog before the eyes, or floaters, you should immediately consult an ophthalmologist. You should not rely on the fact that everything will go away on its own, since with a concussion and contusion of the eyeballs, swelling of the cornea , hemorrhage, and detachment of the iris can occur. All this requires immediate treatment from a specialist.
Traumatologist
The first doctor you should contact after receiving a traumatic brain injury. A traumatologist will examine the victim, provide first aid, give an initial opinion and send him for further treatment to a neurologist, surgeon or other specialized specialists. The traumatologist can also decide on further hospitalization of the victim.
Neurologist
Primary physician in the treatment of concussion. After discharge from the hospital, the injured person must be observed by a neurologist for a year. If the injury is minor and you have not contacted a traumatologist, you should definitely visit a neurologist. He will prescribe the necessary additional studies to exclude post-traumatic effects on the brain and prescribe treatment.
We are taking urgent measures
What should parents do if their child has suffered a traumatic brain injury? There is only one answer: the child should definitely and urgently be shown to a doctor. It is best to immediately call an ambulance, which will definitely take the child to a hospital with pediatric neurosurgeons or neurologists. And this measure is not unnecessary. With minimal symptoms and complaints, the baby may have severe brain damage. The long-term visible well-being of the child, the absence of symptoms, especially with hemorrhages in the brain, often after a few hours and even days is replaced by a progressive deterioration of the condition, which begins with a change in the child’s behavior, his increased excitability, there may be nausea, vomiting, nystagmus, and in infants the fontanelle bulges , then drowsiness appears, depression of consciousness is observed.
What to do first?
Even if the bruise is insignificant at first glance, and the symptoms are almost not expressed, it is better to show the child to the doctor at the first opportunity. Only an examination of the injury by a qualified specialist will help establish an accurate diagnosis and avoid subsequent complications.
The method of providing first aid at home depends on the severity of the injury and the baby’s well-being.
- So, if a child loses consciousness, first of all you need to check your breathing and pulse. In infants, it is recommended to do this in the area of the fontanelle and armpit; in older children, the pulse can easily be determined in the area of the carotid artery.
- If there is a pulse and breathing, you need to lay the child on his side and cover him with a warm blanket.
- If you lose your pulse, you need to perform artificial respiration and chest compressions: 2 breaths and 30 chest compressions.
- If the child did not lose consciousness, then the site of the bruise should be examined, and if the wound is open, bandage it to stop the bleeding. Place a cold compress and ice on the hematoma site.
Attention. You should not let your child fall asleep for an hour or an hour and a half after an injury, because during this period of time deterioration may begin; it is necessary to constantly monitor his condition. Before being examined by a doctor, the baby should be completely at rest and under supervision.
If a child has suffered a concussion, the first thing parents need to do is call an ambulance. Before her arrival, examine the baby’s head, and if there are skin lesions, treat the wound with a non-alcoholic antiseptic (Chlorhexidine, hydrogen peroxide). You can stop the bleeding with a cotton-gauze swab and apply a bandage on top.
Important! If you use an alcohol antiseptic, the child may experience painful shock.
What to do if you lose consciousness?
If a serious injury occurs, accompanied by loss of consciousness, the patient should be placed on a horizontal, flat surface on his right side, his right arm should be placed under his head, and his leg should be slightly bent at the knee joint. Bend your left arm at the elbow and place it along your body. These manipulations will help give the patient an optimal physiological position, and will also protect against choking if vomiting suddenly begins.
What actions are prohibited?
There are a number of actions that are prohibited from doing if a child has a concussion:
Leave the patient unattended, regardless of the severity of symptoms.- In case of fainting, shake the child to bring him to his senses.
- Lay on your back.
- Place in a position in which the head is lower than the body.
- Ignore symptoms and self-medicate.
In addition, you should not make a fuss, panic or make noise around the victim , as this will only worsen his condition.
What to do if there is no way to call a doctor?
If it is not possible to call an ambulance, the child still needs to be taken to the hospital after first aid has been provided.
Diagnosis of concussion
In the hospital, the child is examined by a pediatric neurologist, neurosurgeon or traumatologist. He carefully ascertains complaints, collects anamnesis (history of the disease), and conducts a general and neurological examination. Additional diagnostic methods are prescribed. The main ones are skull radiography, neurosonography (in young children), echo-encephalography (Echo-EG). If necessary, computed tomography of the brain (CT), magnetic resonance imaging (MRI), electroencephalography (EEG), lumbar puncture.
Radiography
skull is performed in most patients. The purpose of this study is to identify skull fractures. The presence of any damage to the bones of the skull automatically transfers the injury to the category of moderate or severe (depending on the condition of the child). Sometimes in young children with a favorable clinical picture, linear fractures of the skull bones are revealed on radiographs. It is impossible to judge the state of the brain substance from radiographs.
Neurosonography
(NSG) is an ultrasound examination of the brain.
Neurosonograms clearly show the substance of the brain and the ventricular system. You can identify signs of cerebral edema, areas of contusion, hemorrhages, and intracranial hematomas. The procedure is simple, painless, quickly performed, and has no contraindications. It can be done multiple times. The only limitation of neurosonography is the presence of so-called “natural ultrasound windows” - a large fontanelle or thin temporal bones. The method is very effective in children under 2 years
. Later, ultrasound becomes difficult to pass through the thick bones of the skull, which dramatically degrades image quality. Equipment for performing neurosonography is available in most children's hospitals.
Echo-encephalography
(Echo-EG) is also an ultrasound research method that allows you to identify displacement of the structures of the midline of the brain, which may indicate the presence of additional space-occupying formations of the brain (hematomas, tumors), and provide indirect information about the state of the brain substance and the ventricular system. This method is simple and fast, but its reliability is low. Previously, it was widely used in neurotraumatology, but with the availability of modern diagnostic tools, such as neurosonography, computed tomography and magnetic resonance imaging, it can be completely abandoned.
The ideal method for diagnosing brain damage and diseases is computed tomography.
(CT). This is an x-ray research method in which high-definition images of the skull bones and brain matter can be obtained. CT can diagnose almost any damage to the bones of the vault and base of the skull, hematomas, bruises, hemorrhages, foreign bodies in the cranial cavity, etc. The accuracy of this study is very high. Its main disadvantage is that the CT machine is expensive, and not every hospital has it.
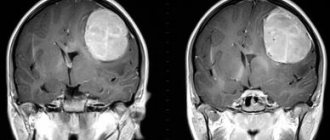
Magnetic resonance imaging
(MRI) is the most accurate, but complex and expensive method of examining the central nervous system. It is rarely used to diagnose acute traumatic brain injury because it does not allow the bones of the skull to be seen, is less accurate for recognizing acute hemorrhages, takes longer than computed tomography, and often requires anesthesia when examining small children - the child must lie absolutely still for 10 -20 minutes, but small children cannot do this; In addition, very few clinics can boast of having magnetic resonance imaging scanners.
Advertising
Electroencephalography
(EEG) allows you to study the bioelectrical activity of the brain. It is used for special indications to assess the severity of traumatic brain injury and identify foci of epileptic activity. A focus of epiactivity is an area of the cerebral cortex with pathologically altered activity of neurons (nerve cells), which can lead to epileptic seizures.
Lumbar puncture
- this is the collection of cerebrospinal fluid (the fluid that bathes the brain and spinal cord) from the spinal canal at the lumbar level. Changes in the cerebrospinal fluid may indicate injury or hemorrhage (the presence of blood) or an inflammatory process, meningitis. Lumbar puncture is performed extremely rarely and only for special indications.
Concussion in children: signs and how to help
Children are little tomboys whose favorite pastimes are running, jumping, fighting, climbing trees... This is why the risk of getting an injury or concussion in childhood is much higher than in adults. How to understand that a child has a concussion and what to do in this case?
What is a concussion?
This is a brain injury caused by a blow to the head. A concussion is a mild form of traumatic brain injury. In childhood, the risk of concussion is higher than in adults, and therefore parents need to know what its manifestations are in children. According to statistics, every fifth teenager has had a concussion at least once in their life.
Signs and symptoms of concussion in children:
- headache;
- drowsiness;
- everything around is as if “in a fog”;
- nausea, vomiting;
- noise and photophobia;
- irritability;
- the child sleeps more or less than usual;
- depression or sadness;
- dizziness or balance problems;
- inability to think or concentrate correctly.
In most cases, the child does not lose consciousness during the injury. Signs of a concussion do not always develop immediately after the impact. Sometimes they occur within hours or even days. Therefore, parents need to closely monitor the child's condition for some time after he hit his head.
How does a concussion manifest in infants and young children?
Babies and very young children cannot tell you what is wrong with them. In addition to the above signs, a small child:
- unable or unwilling to breastfeed or eat;
- loses interest in toys;
- cries for a long time and cannot calm down;
- loses acquired skills, such as potty training.
What to do if you suspect your child has a concussion?
If a child is playing sports or playing and you notice a blow to his head, the game should be stopped immediately. Even if you are not sure that your child has suffered a concussion, returning to play is not recommended. Contact your doctor if your child complains to you or develops any of the above symptoms. This can happen at the time of injury or hours or even days later.
Which doctor should I contact?
If you notice signs of a concussion in your child, you need to contact a neurologist. The pediatric specialist will prescribe the necessary examinations that can reveal how severe the injury was and, depending on this, will give his recommendations.
To establish an accurate diagnosis, a pediatric neurologist can refer the patient to an ophthalmologist, neurosurgeon, otolaryngologist and other specialists.
When is emergency help required?
Sometimes a head injury leads to a hematoma in the child's brain. A hematoma is a collection of blood that forms in the brain and compresses its tissues.
Call an ambulance if your child has the following symptoms:
- loss of consciousness upon impact;
- memory loss;
- convulsions (muscle trembling or twitching);
- slurred speech;
- the child cannot wake up;
- repeated vomiting;
- sharp worsening of the above symptoms of concussion.
Does your child have a concussion?
Make an appointment/Call a doctor
Callback form
Application has been sent, we will contact you soon
Treatment: what can be done at home?
- the first thing to do is to provide the child with peace. Rest helps the brain recover.
- The child should not engage in sports or other physical activity.
- mental rest is equally important. The child should not do anything that requires a lot of concentration, such as completing schoolwork.
- Minimize the time your child spends in front of the TV screen or gadgets.
Many children have trouble sleeping after a concussion: they may sleep longer than usual or have difficulty falling asleep.
How to help?
- remove distractions from the bedroom (TV, gadgets, etc.)
- encourage routine activities (getting your child ready for bed)
- Headaches are the most common problem following a concussion.
Simple painkillers may help, but check with your doctor first. After a few days of rest, the child can gradually return to his normal activities. But sports or other vigorous physical activity should not be resumed until the child has no symptoms at rest.
How long can recovery take?
Most often, improvement occurs within two weeks. But sometimes unpleasant symptoms can bother a child for several months or longer. A study found that one in four children still complain of headaches even one month after the injury! Around a fifth suffer from fatigue, and almost 20% said they take longer to think about issues than before the injury. Check with your pediatrician if your child's symptoms persist or worsen. If your child has been involved in sports, you should also talk to your doctor to develop a plan to safely return to exercise.
Who is at particular risk?
Any child or adult can get a concussion, although for some the risks are higher: - in children under 4 years old - from a fall - from playing certain sports such as football, basketball or ice hockey.
Could there be consequences?
Most children make a full recovery from a concussion. But for some, the consequences can be more serious and long-lasting. The risk of dangerous complications is possible if adults take a child’s concussion lightly. Therefore, do not neglect the seriousness of this injury! Take care of your children and be healthy!
Ultrasound signs of brain injury that exclude a concussion:
- the presence of hyperechoic inclusions in the brain parenchyma against the background of a general decrease in tissue echogenicity - with brain contusions;
- a decrease in the echogenicity of the brain parenchyma in the first few hours after injury and its normalization on days 6-7 - with swelling of the brain parenchyma;
- the presence of an intraventricular hyperechoic zone, a change in the shape of the choroid plexus - with intraventricular hemorrhages;
- a clearly demarcated spindle-shaped area adjacent to the skull bone, with increased or decreased echogenicity, which displaces the structure of the brain - with epidural hematomas;
- areas of the brain parenchyma of an isoechoic nature, which are visible only due to their additional volume - with severe brain contusions;
- areas of additional volume with a clearly defined contour and an intense increase in echogenicity - in case of severe bruises;
- areas of additional volume with a moderate increase in echogenicity and an unclear contour - with severe bruises.
How to avoid head injury?
Parents cannot always control the child’s actions, and therefore, unfortunately, it is also impossible to avoid all injuries. However, there are certain rules that will help reduce the likelihood of injury as much as possible.
So, when playing sports, the child should be dressed in special equipment with appropriate head protection. In cars, remember to place children in child seats and fasten seat belts. Furniture in the house should be as traumatic as possible for small children. In addition, it is necessary to maintain cleanliness in the premises and, if liquids are spilled on the floor, wipe them up immediately to avoid falling and associated injury.
TBIs are divided into 3 degrees of severity
Lightweight
These are minor injuries that are not particularly dangerous. Most often, your health improves after 20-30 minutes.
- In newborns and infants: loss of consciousness is not observed, symptoms are visible in the first 15-20 minutes. Characteristics of TBI are increased body temperature, vomiting and regurgitation. After this time, the babies return to normal and calm down.
- In children from one to two years: a short-term loss of consciousness may occur;
- headache;
- nausea;
- Noticeable damage may appear (bruises, contusions, nosebleeds, etc.).
Average
In newborns and infants: the pulse may slow down or speed up; you should check every 15 minutes. Restless crying, vomiting, disorientation and loss of coordination lasting more than 25 minutes.- In children aged one to two years, loss of consciousness, disorientation in space, inability to give a clear answer, “rumbling” in the head, a feeling of weakness, nausea, the gaze cannot concentrate on a specific object, absent-mindedness, inhibited reaction.
Heavy
- In newborns and infants: severe crying;
- loss of appetite;
- lack of coordination (on the one hand);
- pallor;
- sometimes blueness of the skin;
- possible shortness of breath;
- displacement, curvature, depression of the fontanel;
- vomit;
- sleep disturbance.
- blurred vision;
temporary blindness;
Coordination and regulation in space are impaired, a feeling of squeezing of the head and slurred, meaningless speech may appear.
Methods for diagnosing TBI
An important examination for head trauma in infants is neurosonography - a study of the structure of the brain using an ultrasound machine through the child’s large fontanel (such a study is possible until the large fontanelle closes, up to 1 - 1.5 years). This method is easy to use, does not have a negative effect on the body, and provides enough information to determine treatment tactics for the patient. With its help, you can first of all exclude or determine the presence of intracranial hemorrhages (the most life-threatening). The only limitation to its use may be the absence in the hospital of an ultrasound machine or a specialist who knows how to operate it (for example, not all hospitals in the country that have ultrasound machines can conduct emergency neurosonography at night, since the specialist works during the day).
If intracranial hemorrhage is suspected (especially if for various reasons it is not possible to do neurosonography), a lumbar puncture is performed - a therapeutic and diagnostic procedure in which a hollow needle connected to a syringe is used to puncture the area of the second to fourth lumbar vertebrae of one of the spaces of the spinal cord (subarachnoid space) and taking a portion of cerebrospinal fluid for examination under a microscope. The presence of intracranial hemorrhage is determined by the presence of blood cells in the cerebrospinal fluid.
In addition, there are more complex methods for examining a child’s head: computed tomography (CT) and magnetic resonance imaging (MRI).
Computed tomography (CT) (from the Greek tomos - segment, layer + Greek grapho - to write, depict) is a research method in which images of a certain layer (slice) of the human body (for example, the head) are obtained using X-rays. With CT, the rays hit a special device that transmits information to a computer, which processes the received data on the absorption of X-rays by the human body and displays the image on the monitor screen. In this way, the smallest changes in the absorption of rays are recorded, which in turn allows you to see what is not visible on a regular x-ray. It should be noted that radiation exposure with CT is significantly lower than with conventional X-ray examination.
Magnetic resonance imaging (MRI) is a diagnostic method (not associated with x-rays) that allows you to obtain layer-by-layer images of organs in various planes and construct a three-dimensional reconstruction of the area under study. It is based on the ability of some atomic nuclei, when placed in a magnetic field, to absorb energy in the radio frequency range and emit it after the cessation of exposure to the radio frequency pulse. For MRI, various pulse sequences have been developed to image the structures under study to obtain optimal contrast between normal and altered tissues. This is one of the most informative and harmless diagnostic methods.
But the widespread use of CT and MRI in early childhood is difficult due to the need to conduct this examination in children in a state of immobility (under anesthesia), since an important condition for the successful implementation of the technique is the immobility of the patient, which cannot be achieved from an infant.
Signs of head injuries by age and their complications
Let's look at how to understand that an infant or a child aged 2 years has suffered a concussion after a fall.
In an infant during the first 20 weeks
How does a concussion manifest in an infant in the first months of life? Signs:
Prolonged crying after injury and after a while.- Regurgitation of more than 25 ml of breast milk or formula, more than twice at one meal.
- Vomit.
- Noticeable swelling of the fontanel.
- Pallor.
- Bluishness (the baby’s lips and skin may take on a light blue tint) due to lack of oxygen.
- Your heart rate may slow down significantly.
At this stage, vomiting and regurgitation are the main symptoms. It is difficult to lull the baby to sleep; the baby may refuse to eat and the sucking reflex may be impaired.
Important! If after receiving an injury the baby immediately loses consciousness, you must immediately call an ambulance.
If you do not provide help, you may encounter a number of complications in the future:
- Impaired coordination of movements.
- Developmental retardation (inhibition in motor and speech development).
- Increased sensitivity to various infections.
- In a particularly severe form, hydrocephalus may develop.
In a baby from 6 to 9 months
At this age from six months to 8 or 9 months, the symptoms are very similar , but you should pay attention to:
- Pain when lifting, difficulty supporting the head on your own.
- Uncontrollable crying with temporary delay (swallowing) of air.
- Intermittent sleep.
- Not typical activity for a child.
- Uncontrolled body movements, most often on one side.
- The size of the pupils - if the pupils are of different sizes, this is a sign that the brain is damaged and urgent hospitalization is necessary.
In babies from 9 to 12 months
Signs of a concussion in an infant over 9 months of age and in a one-year-old baby:
- Increased heart rate from 140 beats and above.
- A sharp increase or decrease in pressure.
- Lack of appetite.
- Tearfulness.
- Cold extremities.
- Excessive salivation.
At this age, after an injury, it is necessary to measure the pulse every 20 minutes and note the dynamics .
It is necessary to check the fontanel and the site of the bruise, carefully monitor the child’s condition and well-being. At this age, a concussion carries the same consequences as mentioned above, but epilepsy, seizures and tics can also develop.
How to determine after 1 year?
Let's consider the signs of TBI in a one-year-old child and under the age of 2 years.
- Head pain and dizziness.
- Temporary blindness.
- Noise in ears.
- Temporary disorientation.
- Whims, bad mood.
In addition to these complications, the following may also occur:
- Meteor dependence.
- Depression and frequent mood swings.
- Some people find it difficult to manage their emotions.
- Loss of appetite leads to lack of body weight, as well as a lack of vitamins.
- Frequent fatigue, lethargy, weakness.
- Sleep disturbance.
- Frequent headaches, dizziness.
- Memory and speech disorders.
- Motor and movement function is impaired.
Children over the age of one year often experience increased sweating, weakness and a rapid pulse.
Reference. With a brain injury, a child immediately loses orientation in space, the ability to concentrate and fixate his gaze.