TG Therapeutics disclosed the results of two pivotal clinical trials testing experimental ublituximab in the treatment of relapsing forms of multiple sclerosis.
Everything went more than successfully, and TG intends to send the registration dossier of ublituximab to regulators in the third quarter of 2021.
Ublituximab, if approved, would compete directly with two existing disease-modifying multiple sclerosis drugs (MDTs), Ocrevus (ocrelizumab) and Kesimpta (ofatumumab), promoted by Roche and Novartis - because it has a similar mechanism of action.
Ublituximab: effectiveness of treatment of multiple sclerosis
The ULTIMATE I (NCT03277261) and ULTIMATE II (NCT03277248) phase III clinical trials (randomized, double-blind, active comparator, multicenter, international), identical in design, tested ublituximab in the treatment of relapsing forms of multiple sclerosis in adults (18–55 years). ) patients (n=1094).
Among the main criteria for inclusion in the trial:
Serious adverse reactions were reported in 9.5% of patients prescribed ublituximab, and the most common were infections (4.0%) and nervous system disorders (0.9%). Two cases of malignant neoplasms (endometrial cancer, uterine cancer) and three deaths were recorded, one of which was caused by treatment (pneumonia). There were no cases of progressive multifocal leukoencephalopathy (PML).
"Kesimpta" for the treatment of multiple sclerosis: what next
Novartis continues to conduct numerous clinical trials testing the usefulness of ofatumumab in the treatment of relapsing forms of multiple sclerosis:
- ALITHIOS (NCT03650114) phase III. Study of the safety and effectiveness of ofatumumab in the long-term treatment period (up to 5 years). In parallel, the effects of ofatumumab on the antibody response after administration of vaccines against tetanus, pneumonia, and influenza are being assessed. Such testing is needed because in the phase III VELOCE clinical trial (NCT02545868), Roche found that patients with multiple sclerosis treated with ocrelizumab had a weakened humoral response to non-live vaccines, although it could still be expected to be protective. .
- STHENOS (NCT04788615) phase III. Comparison of ofatumumab with first-line platform drugs that previously untreated multiple sclerosis patients can self-administer: Copaxone (glatiramer acetate), Tecfidera (dimethyl fumarate), Aubagio (teriflunomide) or interferon.
- ARTIOS (NCT04353492) phase III. To evaluate the effectiveness of ofatumumab among patients with multiple sclerosis who are receiving oral DMTs, Gilenya (fingolimod) or Tecfidera (dimethyl fumarate), but decide to discontinue them due to relapse of multiple sclerosis.
- OLIKOS (NCT04486716) phase III. To evaluate treatment in patients previously treated with anti-CD20 therapy with intravenous ocrelizumab or rituximab who then switched to subcutaneous ofatumumab.
- KYRIOS (NCT04869358) phase IV. To study the immune response among patients who received an mRNA COVID-19 vaccine and who have not yet started or are on ofatumumab therapy for multiple sclerosis. Two more trials, NCT04878211 and NCT04847596, are being organized in parallel to understand the immune response to vaccination against SARS-CoV-2.
- NCT04667117 phase IV. It is necessary to determine whether patients considering or already adhering to ofatumumab therapy for multiple sclerosis have an adequate humoral immune response to the seasonal influenza vaccine.
- TIMIOS (NCT04676555). The task was set to clarify the economic picture of the costs of Kesimpta and Ocrevus. To do this, it will identify the direct costs borne by the US, UK and Australian healthcare systems associated with the time required to prepare and administer these drugs and follow up with patients, as well as the resources required to manage side effects. Indirect costs attributable to patient disability will be identified.
Ublituximab: mechanism of action in multiple sclerosis
Ublituximab is a chimeric monoclonal IgG1 antibody that targets a specific epitope of the CD20 surface antigen that is expressed on B cells at all stages of their development (except the first and last).
Ublituximab binds to CD20, thereby activating the immune system to lyse B cells through complement-dependent cytotoxicity (CDC), antibody-dependent cell-mediated cytotoxicity (ADCC), and phagocytosis. The resulting depletion of the B cell pool has a beneficial therapeutic effect in multiple sclerosis.
The molecule (LFB-R603), developed by the French LFB Biotechnologies and initially focused on the treatment of chronic lymphocytic leukemia, belongs to the third generation of medicinal compounds of this class. In early March 2012, TG acquired a worldwide license for ublituximab.
Thanks to the modified glycolysis scheme due to the crystallizing fragment (Fc) with a low fucose content, increased affinity for all variants of Fc-gamma receptor IIIA (FcγRIIIA, CD16a) is realized. As a result of enhanced binding to the latter on effector cells such as macrophages, T helper cells and natural killer (NK) cells, ublituximab is characterized by significantly increased ADCC, directly affecting B-lymphocyte depletion. Such engineering solves one of the problems of monoclonal antibodies, when they have insufficient therapeutic efficacy, despite their high specificity for target cells. This is true for ublituximab when compared to other CD20-targeted drugs already approved for multiple sclerosis, such as Ocrevus (ocrelizumab), which is developed by Roche, and Kesimpta (ofatumumab). , which is promoted by Novartis.
Thus, in vitro on donor cells from healthy people and patients with chronic lymphocytic leukemia (CLL), ublituximab demonstrated 100 times greater ADCC activity mediated by natural killer (NK) cells than rituximab. In vitro, ocrelizumab showed two to five times greater ADCC activity against CD20-expressing cells compared to rituximab.
New treatment strategies for multiple sclerosis
There are a number of other possible immunotherapies that could potentially have a beneficial effect in multiple sclerosis. In the future, this series is likely to expand as knowledge of the immunopathogenesis of the disease increases. Some drugs have undergone preliminary clinical trials (eg, transformed growth factor P, T-cell vaccine, anti-α4 integrin antibodies, phosphodiesterase inhibitors, anti-CD4 antibodies, T-cell antagonist peptides).
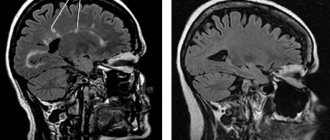
Sometimes the results of these studies are inconsistent with expectations, reflecting an incomplete understanding of the pathogenesis of multiple sclerosis. For example, treatment with anti-TNF antibodies in two patients with rapidly progressive multiple sclerosis had no effect on clinical status but did cause a transient increase in the number of active, contrast-enhancing lesions on MPT.
Medicines for the treatment of this disease began to be imported to Russia only in 2006, but the cost of these drugs was so high that they made treatment inaccessible. After the inclusion of the disease in the federal-scale program “Seven Nosologies” in 2008, there was a guarantee of providing patients with medicines at the expense of the state.
Nowadays, new drugs are increasingly appearing in the treatment of multiple sclerosis.
The emergence of Russian-made analogues was a great success and victory.
When the patent protection period for original drugs expires, they are allowed to be reproduced in our country. Generic companies are ready for this. All work on developing a copy is usually carried out in advance, since the formula of any original medicine is known. Registration of an analogue can also be done in advance, since this process is quite long.
As a rule, generics are registered according to a simplified scheme, which is a worldwide practice. Manufacturers of the analogue do not need to conduct long-term clinical trials; they only need to prove how accurately the compositions of the active substance of the original and the analogue match. Based on this, we get a more affordable price.
According to statistics, Russian medicines cause wariness and mistrust among both doctors and patients. This is explained by the fact that for them treatment with proven drugs is more reliable. So, let's look at new drugs for the treatment of multiple sclerosis.
Many new drugs for treatment are in the clinical research phase.
- "Mitoxantrone" is a cytotoxic drug that suppresses the immune system, the number of relapses is reduced.
- "Cladribine" - normal lymphocyte function will be restored, structural changes in the brain will be reduced. But during experimental trials, side effects were discovered: exacerbation of brain diseases, malignant tumors. The drug was deregistered. A repeat application will be made after revision.
- "Laquinimod" - the lymphocytic function of the immune system is restored, the number of exacerbations decreases, and there are no destructive neurological processes.
Ublituximab versus Ocrevus and Kesimpta
Overall, minor discrepancies aside, the therapeutic efficacy and safety of ublituximab are similar to those of ocrelizumab and ofatumumab.
TG desperately needs marketing leverage to challenge the Swiss giants Roche and Novartis. Ublituximab will be promoted among doctors and patients, obviously promoting the following provisions.
- Ublituximab provided a stronger reduction in annualized relapse rate (ARR) for multiple sclerosis. In absolute terms, ublituximab reduced the ARR to 0.076–0.091 after 2 years of administration. Ocrevus reduced this figure to 0.155–0.156, and Kesimpta to 0.10–0.11.
- Ublituximab was more successful than ocrelizumab and ofatumumab in containing documented progression of disability in multiple sclerosis. Thus, 3mCDP and 6mCDP status was true for 5.2% and 3.3% of patients who adhered to ublituximab treatment. During the clinical trial of Ocrevus, more patients reached these indicators - 9.8% and 7.6%. Testing of "Kesimpta" showed 3mCDP and 6mCDP in an even larger proportion of patients - 10.9% and 8.1%.
- In the maintenance regimen, ublituximab is administered intravenously once every six months; infusions last 1 hour. Ocrevus, similarly prescribed once every six months, is infused over 3.5–4 hours, or 2 hours if the patient has not experienced any serious adverse reactions to previous infusions of the drug. Ublituximab and ocrelizumab require premedication to reduce the risk of adverse reactions to drug infusions: 30 minutes before the administration of the first, patients receive an oral antihistamine and a corticosteroid, 30 minutes before the administration of the second, patients are prescribed an oral antihistamine and paracetamol and an intravenous corticosteroid, "Kesimpta", sold in in the form of an auto-injector for subcutaneous injections, used by patients independently once a month; no premedication is needed.
- TG has repeatedly said that it plans to make ublituximab more affordable than Ocrevus. This is understandable: since ublituximab is effective in lower doses than ocrelizumab (450 mg versus 600 mg), its cost is lower. Currently, an annual course of maintenance therapy for multiple sclerosis with Ocrevus costs American patients 70 thousand dollars, and Kesimpta costs 87 thousand dollars.
If we ignore T.G.'s understandable desire to highlight its drug from a favorable angle, the picture is not so rosy. Yes, in the first couple of years of therapy, ublituximab did reduce ARR more than rival anti-CD20 drugs did. But T.G. did not report any change in ARR during follow-up treatment. It is known that Ocrevus continued to lower its ARR to 0.103 as its continued use continued; 0.080; 0.065; 0.044; 0.040 - after 3, 4, 5, 6 and 7 years of treatment, respectively.
Ublituximab more effectively protected patients from the risk of progression of multiple sclerosis: a relatively smaller proportion of patients than those taking Ocrevus or Kesimpta experienced worsening of the disease. This is due, it is believed, to the peculiarities of the mechanism of action of ublituximab, which allows it to maximally deplete the pool of B-lymphocytes (in this case pathogenic) and maintain the proper level of depletion for a long time (until the next infusion of the drug).
Roche understands this and has launched the Phase III MUSETTE clinical trial, which will test doubling and tripling doses of ocrelizumab (1200 and 2400 mg for patients weighing less than 75 kg or more) to ensure a more potent B-cell deprivation will have a beneficial effect on the course of multiple sclerosis, without compromising the safety of treatment.
Ublituximab infusions are faster, but Ocrevus is no slouch. Thus, the ENSEMBLE PLUS substudy of the phase III clinical trial ENSEMBLE (NCT03085810) among patients with early relapsing-remitting multiple sclerosis confirmed the possibility of accelerated infusion of ocrelizumab over 2 hours. As a result, in mid-December 2021, a new dosage regimen was included in the instructions for medical use of Ocrevus. To be fair, plus or minus a few hours makes absolutely no difference considering the need for just one dose every six months.
To summarize, the only thing that ublituximab can do for its successful start and decent life cycle is to sharply reduce the cost of treating multiple sclerosis with highly effective DMTs. But the future is never optimistic: a few players in the global pharmaceutical industry are able to curb the greed of their investors who want to get rich quickly.
Anti-CD20 therapy and COVID-19: some nuances
In the context of the ongoing pandemic of coronavirus infection COVID-19, caused by the new coronavirus SARS-CoV-2, the issue of both maintaining immunity after suffering from Covid and vaccination to protect against it is urgent. The fact is that the administration of anti-CD20 drugs depletes the pool of B cells, and in the case of ublituximab and ocrelizumab, B cell depletion continues for many months. In other words, the body is faced with a clear deficiency of humoral immunity. This is confirmed by the increased risk of infection (not SARS-CoV-2) and cancer among those on chronic anti-CD20 therapy.
Roche demonstrated that among patients treated with Ocrevus who were infected with SARS-CoV-2, levels of neutralizing antibodies and IgG antibodies against the S protein of the novel coronavirus were statistically significantly lower than in patients who had recovered from Covid but were not treated with ocrelizumab. However, the administration of Ocrevus had no effect on the T-cell population.
According to an Italian retrospective study, patients with multiple sclerosis treated with ocrelizumab or rituximab more than doubled their chances of developing severe COVID-19. American experts made similar conclusions.
Pharmacodynamic data suggest that restoration of the B-cell pool to levels at least above the lower limit of normal requires a median of 18 months (27–175 weeks) after the last infusion for Ocrevus and a median of 10 months for Kesimpta. Data for ublituximab are unknown, but they are likely to be similar to ocrelizumab.
Since the current anti-Covid vaccines are not live, they do not carry the risk of contracting COVID-19 against the background of immunosuppressive anti-CD20 therapy, however, the latter can still negatively affect the formation of reliable immunity against Covid. In any case, you will have to pause therapy before and after vaccination.
"Xemus"
Our scientists have developed the first domestically produced drug for the treatment of patients suffering from multiple sclerosis. The drug, called Xemus, must still undergo final clinical trials and then enter the pharmaceutical market. They promise that this medicine will be provided to patients with multiple sclerosis free of charge. According to data provided by the Ministry of Health, the number of patients with multiple sclerosis is increasing.
A new drug developed in Russia for the treatment of multiple sclerosis is an analogue of one of the most expensive lots of the state program “7 nosologies”. Registration of this medicine may mean that import substitution has become real; residents of our country will no longer be dependent on foreign supplies of original medicines. More than 5 billion rubles are spent annually on their purchase. According to the developers of the Russian drug, they promise to sell it cheaper.
A trial batch of the developed drug was released back in 2012 in order to conduct clinical trials. The tests went well. The company's site where these tests are carried out is one of the most modern in the country. The company's management spares no expense on personnel training or equipment. This can be confirmed by three certificates that meet international GMP standards.
The latest developments in the treatment of multiple sclerosis have been awaited for a very long time. The drug should have been registered last year, but the procedure dragged on for more than one month. showed its readiness to participate in government procurement, but the auction was postponed by decision of the FAS in order not to violate antimonopoly legislation.
Experts predict that the price will fall due to a competitor not coming to the auction. The company's management stated that the introduction of a Russian analogue to the market will help reduce the cost of purchases by at least 20%.