Neurologist
SEMENOVA
Olga
5 years experience
neurologist, head of the office for diagnostics and treatment of cognitive disorders
Make an appointment
Polyneuropathies (polyneuropathies) are a group of pathologies affecting peripheral nerves. The clinical picture is determined by the form of the disease diagnosed in the patient. Specific signs are muscle weakness and atrophy, decreased tendon reflexes, sensory disturbances, and autonomic disorders. Treatment of polyneuropathy is carried out by a neurologist. The main task of the doctor is to determine the cause of the disease. Therapy is symptomatic.
Causes
The reasons leading to the development of polyneuropathy in patients are varied. Often, damage to nerve cells develops against the background of severe poisoning with methyl alcohol, arsenic or carbon monoxide. Similarly, axonal health can be affected by volatile compounds high in phosphorus.
In some cases, the symptoms of the pathology appear against the background of chronic intoxication of the human body, diphtheria, vitamin deficiency or diabetes mellitus. The disease can develop with uremia, liver cirrhosis, kidney damage, hypothyroidism or cancer. Long-term use by the patient of amiodarone, isoniazid or metronidazole can lead to the manifestation of polyneuropathy.
Forecast
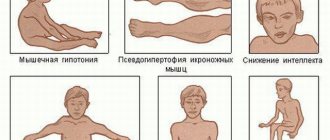
Polyneuropathy is a dangerous disease for humans. In the absence of adequate therapy, the disease progresses and leads to serious consequences. Patients may develop muscle weakness, decreased muscle tone, and then complete muscle atrophy.
Patients are forced to change their usual lifestyle. They lose the ability to move independently and take care of themselves in everyday life. As a result, the level of anxiety increases and chronic depressive syndrome develops. To avoid undesirable consequences and improve your quality of life, if you have signs of polyneuropathy, make an appointment with a neurologist at the Yusupov Hospital by calling. Contact center specialists will offer a convenient time for consultation with a doctor specializing in the treatment of polyneuropathies.
Make an appointment
Kinds
Neurologists distinguish two types of polyneuropathies based on pathogenetic signs of damage to peripheral nerves - axonal and demyelinating. The first form of the disease affects the long, cylindrical extensions of nerve cells called axons. The second provokes the loss of myelin in myelinated nerve fibers. Late stages of axonal disorders are accompanied by demyelination. Primary demyelinating polyneuropathies are complicated by secondary damage to the cylindrical processes of nerve cells.
In the process of diagnosing and treating polyneuropathies, doctors may use other classifications of the disease. Based on the clinical picture, neurologists distinguish motor, sensory and autonomic polyneuropathies. In their pure form, these types of pathology are rare: most patients are diagnosed with damage to two or three types of nerve fibers (motor-sensory, sensory-vegetative, etc.).
Studying the etiology of the disease allows neurologists to identify hereditary, autoimmune, metabolic, nutritional, toxic and infectious-toxic polyneuropathies.
Polyneuropathy
Polyneuropathies, or multiple lesions of peripheral nerves , are widespread diseases. The high susceptibility of the distal sections of nerves to various pathological factors is easily explained by the structural features of nerve cells. Nutrition and other metabolic processes in the processes of peripheral nerves are carried out due to the axoplasmic flow of substances from the cell body through a special transport system. And since the length of the processes is many thousand times greater than the size of the neuron body itself, the terminal sections of the nerves are an extremely vulnerable area. In this case, the main pathogenetic processes are most often axonopathy or demyelination of nerve fibers.
The many nosological forms of polyneuropathies are explained by the fact that, in essence, this disease is a manifestation of systemic suffering of the peripheral nervous system under various unfavorable conditions. At the same time, despite the variety of clinical manifestations, syndromic diagnosis of polyneuropathies does not cause difficulties. Polyneuropathy syndrome is characterized by the presence of:
- muscle weakness and/or atrophy;
- decrease or loss of tendon reflexes;
- decreased sensitivity of the polyneuropathic type;
- pain syndrome in the distal extremities;
- autonomic disorders in the form of disorders of the cardiovascular, urinary systems, gastrointestinal tract (GIT), sweating and sexual function.
One of the key criteria that allows us to distinguish polyneuropathies from the entire spectrum of lesions of the peripheral nervous system are predominantly distal lesions and the relative symmetry of the pathological process.
Diagnosis and causes of the disease
But if the diagnosis of polyneuropathy as a syndrome, in the opinion of most neurologists, does not cause significant clinical difficulty, then identifying the etiological factor that caused the development of this process, on the contrary, is a relatively difficult task. In some cases, the nosological affiliation of polyneuropathy remains unclear. Many studies claim that in non-specialized clinics the number of polyneuropathies of unspecified etiology reaches 50%, and in specialized clinics - 25% of cases.
At the same time, the search for the cause of polyneuropathy cannot be considered redundant. An indisputable fact is the need to identify the etiological factor as the main determining point for developing a therapeutic strategy. The algorithm for diagnosing polyneuropathies may be as follows:
- Anamnesis collection.
- Neurological examination.
- General inspection.
- Electroneuromyography (ENMG).
- Laboratory research methods.
- Instrumental research methods.
- Cerebrospinal fluid examination.
- Nerve biopsy.
When collecting anamnesis, first of all, it is necessary to pay attention to recent infectious diseases, long-term use of medications, working and living conditions, in particular, contact with toxic substances. Family history, the presence of known somatic diseases and dietary habits are also determining factors in the diagnostic search. Due to the high prevalence of alcoholic polyneuropathy, special attention should be paid to evidence of chronic alcohol intoxication. Important diagnostic signs are the rate of development of polyneuropathy , the course of the disease and their connection with life events that have occurred.
Examination of the patient and methods of studying the disease
A neurological examination of the patient involves both identifying symptoms characteristic of polyneuropathies and identifying the leading form of this pathology. Among the manifestations of polyneuropathies, it is customary to distinguish motor, sensory and autonomic groups of symptoms. Moreover, each of these groups can manifest itself with both negative and positive symptoms (Table 1).
During a neurological examination, if the nature of the polyneuropathy is unclear, palpation of the accessible nerve trunks is necessary. Their thickening may be evidence of specific types of polyneuropathies (leprosy, sarcoidosis, Refsum's disease, etc.). Examination of other systems and functions of the nervous system can also make it possible to make a nosological diagnosis.
A general examination of a patient with polyneuropathy in a neurological appointment mostly involves examination of the skin and mucous membranes, examination of the lymph nodes, palpation of the abdomen and measurement of blood pressure and pulse. The presence of deviations in the examination data, indicating somatic pathology or intoxication, requires the involvement of specialists of the appropriate profile. ENMG is one of the most sensitive methods for diagnosing polyneuropathies and helps to identify even subclinical forms. At the same time, this research method determines nonspecific changes and cannot be the only one when making a nosological diagnosis. Stimulation ENMG allows you to assess the speed and quality of impulses along sensory and motor fibers of peripheral nerves , which is necessary to determine the level and nature (axonopathy or demyelination) of the lesion.
Laboratory research methods are aimed at identifying, first of all, metabolic and toxic disorders in the patient. In addition to a clinical blood test, it is advisable to recommend studying the level of urea, creatinine, glycated hemoglobin, liver tests, and rheumatic tests. If intoxication is suspected, toxicological screening is necessary. If there are indications, instrumental methods for studying the somatic status are used, which include radiography, ultrasound, etc. Separately, it should be noted the methods of studying the autonomic nervous system, of which the most accessible and informative is cardiointervalography. It allows one to judge both the state of autonomic innervation and the effectiveness of its regulatory influence.
The study of cerebrospinal fluid is included as a separate item in the examination algorithm, since it is indicated for suspected demyelinating polyneuropathy , acute or chronic, as well as when searching for infectious agents or a neoplastic process.
The last point of the proposed algorithm – nerve biopsy is also inappropriate to recommend as a routine research method. However, it is included in the list of general clinical criteria for the diagnosis of peripheral neuropathies and can be used if necessary to confirm the diagnosis of certain forms of hereditary polyneuropathies, damage to the peripheral nervous system due to amyloidosis, leprosy, sarcoidosis, etc. Invasiveness, the number of complications and side effects during biopsy are significant limiting factors for this procedure.
As a result of the diagnostic process, as a rule, it is possible to identify one or another type of polyneuropathy according to one of the proposed classification methods. Thus, the following types of polyneuropathies are most often distinguished in prisomatic pathology:
- Metabolic: uremic, hepatic, amyloid.
- Endocrine: diabetic, hypothyroid, hyperthyroid.
- Toxic: alcohol, medicinal, lead, arsenic.
- Infectious: diphtheria, leprosy, AIDS, etc.
- Systemic: for systemic lupus erythematosus, periarteritis nodosa, scleroderma.
- Paraneoplastic.
Brief clinical characteristics of the most common forms of polyneuropathies
Uremic polyneuropathy occurs in almost half of patients with chronic renal failure. Characterized by predominantly sensory or sensorimotor symmetrical distal disorders. The disease may begin with cramps (painful cramps) and restless legs syndrome. Then dysesthesia, burning and numbness of the feet occur. Hemodialysis performed for this pathology has an ambiguous effect. On the one hand, its positive effect on the course of polyneuropathy , on the other hand, up to a quarter of patients note an increase in sensory symptoms after starting this type of therapy. In addition, the formation of an arteriovenous fistula associated with dialysis leads to an increase in ischemic mechanisms of damage to peripheral nerves . Hepatic polyneuropathy occurs in both chronic and acute liver damage. The most common causes are primary biliary cirrhosis, alcoholic cirrhosis, hepatitis C. The clinical picture is most often represented by mixed sensorimotor polyneuropathy, which is combined with encephalopathy. Signs of involvement of the autonomic nervous system - orthostatic hypotension, impaired gastrointestinal motility - lead to a worse prognosis in this category of patients.
Amyloid polyneuropathy develops in patients with primary hereditary amyloidosis. It most often manifests itself as pain syndromes in combination with disturbances of pain and temperature sensitivity in the distal parts of the extremities. Motor and trophic disorders occur in the later stages of the disease.
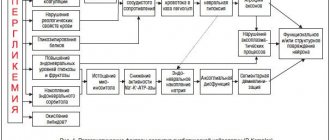
Diabetic polyneuropathy is the most common and studied form of somatic polyneuropathy. Most often presented in the form of a distal symmetrical sensory form, which is characterized by a slowly progressive course, beginning with the loss of vibration sensitivity and loss of the knee and Achilles reflexes. At the same time, it can manifest itself in the form of a fairly intense pain syndrome, with an increase in algia in the evening and at night. The variety of forms of damage to the peripheral nervous system in diabetes mellitus (DM) does not allow us to exclude the predominantly autonomic form with minimal sensory and motor impairment from the list of polyneuropathies under consideration. It manifests itself as peripheral autonomic failure and, in addition to reducing the quality of life of patients, significantly worsens the prognosis due to the development of autonomic cardiac failure. Proximal motor polyneuropathy in diabetes is less common and is characterized by amyotrophy, accompanied by algic disorders.
Types of polyneuropathy
- Alcoholic polyneuropathy
Often develops subacutely. Characteristic symptoms are paresthesia in the distal extremities, pain in the calf muscles during palpation, neuropathic pain, and sensory ataxia. Subsequently, weakness and paresis of the limbs develop, in particular when the peroneal nerve is damaged with the development of a peroneal gait. Hypotension and atrophy of paralyzed muscles develop rapidly. Tendon reflexes may initially be elevated, but later decrease or disappear. Vasomotor, trophic and secretory disorders are very often observed: hyperhidrosis, swelling of the distal parts of the extremities, disruption of their normal coloring, changes in skin temperature. In the differential diagnosis of this form of polyneuropathy , its combination with Korsakoff syndrome plays an important role.
- Drug-induced polyneuropathy
It develops against the background of long-term use of a number of medications. Polyneuropathy most often occurs when taking isoniazid, metronidazole, gold drugs, cardiological (amiodarone, hydralazine, perhexiline, novocainamide), oncological (vincristine, procarbazine, cisplatin) drugs. The main differential diagnostic signs of this type of polyneuropathy , with all the diversity of the clinical picture, are an improvement in the condition after discontinuation of the drug and an increase in symptoms after the resumption of therapy.
- Lead polyneuropathy
It develops mainly subacutely, over several weeks. The disease is preceded by the phenomena of general asthenia, which are manifested by headache, dizziness, increased fatigue, irritability, sleep disturbance, and memory loss. The clinical pattern of dysfunction of peripheral nerves in this form of polyneuropathy is characterized by its originality: damage to the motor fibers of the radial nerves precedes other types of disorders. If the process spreads to the lower extremities, the extensors of the foot are paralyzed first of all. Along with paralysis of the distal limbs, pain in the limbs occurs and sensitivity is impaired according to the polyneuritic type. The course of the disease is usually long - months and sometimes years, even with adequate treatment, since lead is removed from the body slowly.
- Arsenic polyneuropathy
With repeated exposure to small amounts of arsenic, distal symmetrical sensorimotor polyneuropathy develops, in which pain and sensory disturbances dominate. In the case of acute poisoning, the development of clinical polyneuropathy follows a latent period of 2–3 weeks. In this case, muscle weakness develops mainly in the lower extremities. There are pronounced vegetative-trophic disorders: hyperkeratosis, dryness and impaired skin pigmentation, vasomotor disorders, edema. A thickening in the form of a white transverse stripe (Mess stripe) is detected on the nails. Hair loss, trophic disorders of the gums and palate are observed (ulcers form). Recovery of lost functions may continue for many months. Diagnosis is based on detecting arsenic in urine, hair and nails.
- Diphtheria polyneuropathy
It is caused not by an inflammatory process, but by the toxic effects of Corynebacterium diphtheria and autoimmune changes. The destruction of myelin with subsequent degeneration of nerve fibers begins from the terminal branches of the nerves in the muscles. The generalized form of post-diphtheria polyneuropathy develops in the 4th–7th week, during the period of extinction of the infection. It manifests itself as peripheral paresis of the limbs with areflexia, then disturbances of superficial and deep sensitivity are added with the development of sensitive ataxia.
Polyneuropathy in AIDS occurs in almost 30% of patients. It manifests itself, as a rule, in a distal symmetrical, predominantly sensory form. Caused mainly by axonopathy. It begins with loss of vibration sensitivity and is characterized by hyperalgesia with a pronounced pain component. This condition may be aggravated by treatment of infectious or neoplastic pathology due to the development of drug-induced polyneuropathy , to which this category of patients is especially predisposed.
Polyneuropathies in systemic diseases can be either caused by the pathological process itself or be the result of damage to the hepatic and renal systems and the treatment carried out as a result (gold preparations, etc.). Single nerve lesions, multiple mononeuropathy, and symmetrical sensory or sensorimotor polyneuropathy may occur. Paraneoplastic polyneuropathies are not specific and are quite rare. They manifest themselves predominantly as motor, sensory or sensorimotor symptoms. This type of damage to the peripheral nervous system is characterized by subacute development of pronounced neurological deficit with subsequent stabilization of the condition, accompanied by inflammatory changes in the cerebrospinal fluid.
Principles of treatment of polyneuropathies in somatic pathology
Therapeutic measures for this pathology should be carried out taking into account the traditional directions of therapy: etiological, pathogenetic, symptomatic.
Etiological treatment, as the name suggests, will take into account the leading etiological factor that caused the development of this type of polyneuropathy . It should be noted that in some cases, eliminating the cause of the disease is an essential condition for cure (as with drug-induced polyneuropathy). But, unfortunately, this is not always achievable - for example, with diabetes or a systemic autoimmune disease, only complete control of symptoms is possible. And sometimes, as in the case of arsenic intoxication or diphtheria polyneuropathy , the leading pathological factor has already played its negative role, and further influence on it is meaningless. One should also not lose attention to the fact that a fairly large percentage of polyneuropathies remains unsystematized. Therefore, the etiological treatment of polyneuropathies is a desirable, but not obligatory component of the treatment process, in contrast to pathogenetic therapy.
For pathogenetic treatment, it is necessary to influence the main mechanism that caused the development of polyneuropathy . In the case of demyelination and axonopathy, preference is given to vitamin therapy, antioxidants and vasoactive drugs.
Among the wide range of antioxidants in the treatment of diseases of peripheral nerves in somatic pathologies of various origins, α-lipoic acid preparations have proven themselves to be effective. A study of the mechanism of action of this type of therapy in patients with polyneuropathy showed a complex effect on the normalization of endoneurial blood flow, reduction of oxidative stress and improvement of vascular dysfunction.
- In the treatment of polyneuropathies , preference is given to B vitamins. They have a metabolic effect on axonal transport and myelination processes in peripheral nerve fibers.
- In addition, the effect of B vitamins, primarily thiamine, on the central nervous system is mediated through the metabolism of γ-aminobutyric acid and serotonin and causes an analgesic effect.
- It is known that thiamine, localized in the membranes of nerve cells, has a significant effect on the processes of regeneration of damaged nerve fibers, and is also involved in ensuring energy processes in nerve cells and the normal function of axoplasmic current.
- Pyridoxine supports the synthesis of transport proteins in the axial cylinders; in addition, in recent years it has been proven that vitamin B6 has an antioxidant effect.
- Cyanocobalamin affects membrane lipids and is involved in biochemical processes that ensure normal myelin synthesis; necessary for normal hematopoiesis and maturation of red blood cells, has an analgesic effect.
The coenzyme forms of cyanocobalamin - methylcobalamin and adenosylcobalamin - are necessary for cell replication and growth. In this regard, these B vitamins are often called neurotropic. The combination of these vitamins also has a positive effect on the vascular system: for example, a combination of various pyridoxine vitamers inhibits platelet aggregation, realizing its effect indirectly through the activation of prostaglandin E receptors.
In addition, the lack of each of the B vitamins can play a negative role in the formation of clinical manifestations of polyneuropathy in somatic pathology. polyneuropathy develops , reminiscent of alcoholic and diabetic polyneuropathy. Pyridoxine deficiency leads to the development of distal symmetrical, predominantly sensory polyneuropathy, manifested by a feeling of numbness and paresthesia in the form of “pins and needles”. Cyanocobalamin deficiency is manifested primarily by pernicious anemia. Many patients with vitamin B12 deficiency develop subacute degeneration of the spinal cord with damage to the posterior cord, and a relatively small number of patients develop distal sensory peripheral polyneuropathy, characterized by numbness and loss of tendon reflexes.
Thus, the use of B complex vitamins has found a place in many clinical recommendations for the treatment of polyneuropathies . And one of the representatives of well-formulated multivitamin preparations is Neuromultivit. The combined use of thiamine hydrochloride at a dose of 100 mg, pyridoxine hydrochloride - 200 mg, cyanocobalamin - 200 mcg allows to achieve a significant neurotropic effect, leading to favorable changes in the metabolism of nerve fibers. For polyneuropathies of various origins, the use of Neuromultivit can improve both the structural and functional state of the peripheral nervous system .
The dosage form of Neuromultivit, a film-coated tablet, also has a certain advantage. For patients with complex somatic pathology, the use of injection drugs is often associated with an increase in post-injection complications, pain and, as a result, chronic stress, which significantly reduces their adherence to therapy. Taking Neuromultivit 2–3 times a day with meals is a fairly convenient form of therapy.
The third direction of the therapeutic strategy is symptomatic treatment of polyneuropathies . In this case, among the whole range of problems, disorders of autonomic function and pain syndromes come to the fore. In some cases, pain therapy is supported even at the stage of pathogenetic treatment. Thus, the complex use of B vitamins has a proven positive effect on the antinociceptive system, which is extremely important in the treatment of neuropathic pain. Correction of neuropathic pain syndrome requires the use of specific analgesics - antidepressants and anticonvulsants. But the combined effect of B vitamins and non-steroidal anti-inflammatory drugs can significantly reduce the range of unpleasant sensations. Thus, the use of the drug Neurodiclovit, in which the B complex of vitamins is combined with diclofenac (50 mg), successfully leads to a decrease in pain in patients with various types of polyneuropathies .
The most difficult clinical task is the treatment of autonomic disorders in patients with various types of polyneuropathies. At the same time, their prognosis is significantly worsened due to a violation of autonomic regulation - due to its negative impact on the functioning of the cardiovascular system. There are currently no unified recommendations for the correction of these pathological conditions. In general, preference is given to non-drug methods of treating orthostatic hypotension. Thus, the diagnosis and treatment of polyneuropathies in somatic diseases are the immediate task of a neurologist, the solution of which can influence both the state of peripheral nervous system and the prognosis of the leading disease and the quality of life of this category of patients as a whole.
Literature
- Barantsevich E.R., Melnikova E.V., Skoromets A.A. Pathogenetic aspects of neurological disorders in diabetes mellitus // Scientific notes of St. Petersburg State Medical University named after. I.P. Pavlova. 1998. T. 5. No. 2. P. 26.
- Boyko A.N., Batysheva T.T., Kostenko E.V., Pivovarchik E.M., Ganzhula P.A., Ismailov A.M., Lisinker L.N., Khozova A.A., Otcheskaya O .V., Kamchatnov P.R. Neurodiclovit: possibility of use in patients with back pain // Farmateka. 2010. No. 7. pp. 63–68.
- Batueva E.A., Kaygorodova N.B., Karakulova Yu.V. The influence of neurotrophic therapy on neuropathic pain and the psycho-vegetative status of patients with diabetic neuropathy // Russian Journal of Pain. 2011. No. 2. P. 46.
- Vorobyova O.V. Polyneuropathy . Possibilities of alpha-lipoic acid in the treatment of polyneuropathies associated with somatic diseases // Health of Ukraine. 2007. No. 6/1. pp. 52–53.
- Kurushina O.V., Rybak V.A., Barulin A.E., Saranov A.A. Psychophysiological aspects of the formation of chronic pain syndromes // Bulletin of the Volgograd State Medical University. 2010. No. 02. pp. 52–54.
- Levin O.S. Polyneuropathy . M.: MIA, 2005. 496 p.
- Morozova O.G. Polyneuropathy in somatic practice // Internal medicine. 2007. No. 4 (4). pp. 37–39.
- Brownlee M. Biochemistry and molecular cell biology of diabetic complication // Nature. 2007. Vol. 414 (6865). R. 613–820.
- Granados-Soto V., Sanchez-Ramirez G., La-Torre MR et al. Effect of diclofenac on the antiallodinic activity of vitamin B12 in a neuropathic pain model in the rat // Proc West Pharmacol Soc. 2004. Vol. 47. P. 92–94.
- Zambelis T., Karandreas N., Tzavellas E. et al. Large and small fiber neuropathy in chronic alcohol-dependent subject // J Periph Nerv Sys. 2005. Vol. 10. P. 375–338.
Symptoms of pathology
During the examination of the patient, the neurologist identifies signs of damage to motor, sensory and autonomic fibers. The degree of involvement of these structures in the pathological process determines the clinical picture of the disease. Thus, when occupational polyneuropathy is detected in men and women, neurologists record sensory-vegetative symptoms (which are associated with regular fixation of muscles in a state of static tension).
The predominance of motor signs of pathology becomes the cause of the development of paresis of the upper and lower extremities. In the absence of treatment, the patient's individual muscle groups atrophy, including the respiratory ones (against the background of Guillain-Barré syndrome). Later, tendon reflexes decrease, and the person has difficulty performing basic tasks such as fastening buttons or tying shoelaces.
Sensory symptoms develop symmetrically, affecting the feet and hands of patients in the early stages. Sensitivity disorder manifests itself in different ways. Patients may experience tingling, burning, numbness, and pain. In the later stages of the disease, adults and children experience disturbances in the pain and temperature sensitivity of the skin.
Autonomic disorders are accompanied by dry skin and dysregulation of vascular tone. Over time, patients develop signs of tachycardia and unstable functioning of the gastrointestinal tract. Men may experience erectile dysfunction.
Treatment of polyneuropathy
A patient who has been diagnosed with polyneuropathy of the upper or lower extremities needs to prepare for long-term complex treatment, since the matter is not limited to the fight against symptoms that are not visible in the photo. When the disease occurs, nerve fibers are destroyed. It will take a lot of time and effort to restore them.
Initially, therapy begins with an impact on the cause that caused the disease, that is, with treatment of the main disease or stabilization of the patient’s condition. For example, if the cause is diabetes, then it is first important to reduce the sugar level in the body, and with an infectious-allergic cause of polyneuropathy, you should first fight the infection, and only then relieve the symptoms. If there is a deficiency of B vitamins, doctors first compensate for the deficiency, then treat polyneuropathy. If the cause of the disease is disturbances in the proper functioning of the endocrine system, hormone therapy is indicated. If the disease is accompanied by severe pain, then an anesthetic is prescribed orally and locally.
The most common treatment for polyneuropathy is vitamin therapy. A positive result is given by medications that improve blood microcirculation, thereby affecting the quality of nutrition of nerve fibers. Physiotherapeutic techniques, including electrophoresis, are widely used during treatment.
If the treatment is successful and the nerve fibers are restored in full, it is too early to relax and return to your normal lifestyle. It is necessary to conduct a course of rehabilitation therapy, since the disease affects the muscles, because lack of movement leads to a rapid weakening of muscle tissue. To regain your former mobility, you need to spend a long time and put in a lot of effort, and use the help of several specialists at once.
During rehabilitation, therapeutic massage is indicated. It may last 30, 40 or 60 minutes, depending on the severity of the problem and the need. A high-quality massage improves elasticity and tone of muscle and other tissues, reduces tension, has a positive effect on joint mobility, improves metabolic processes and lymph circulation, reduces stress levels and improves immunity.
Various physiotherapeutic methods also provide good results. They also improve microcirculation, relieve pain and restore muscle cells. For serious injuries, when full restoration of the upper or lower extremity is impossible, sessions with an occupational therapist will help. Occupational therapy is treatment by action. The specialist helps the patient adapt to the new condition, develop a new movement algorithm for performing everyday activities. The scheme of rehabilitation measures is prescribed individually for each patient. It may also include vitamin therapy, work with a psychologist, diet therapy and other methods.
When treating acute polyneuropathy, it is important to maintain joint mobility in the patient, even if he has already developed bedsores. Therefore, passive or active therapeutic exercises aimed at increasing the range of motion should be performed several times a day. It is important to pay attention to replacement therapy in bed and stretching. During the acute phase, it is necessary to control pain and relieve it with painkillers.
Patients with Guillain-Barré syndrome should receive respiratory support if necessary. You should also take time to learn how to use various aids.
Treatment of chronic polyneuropathy consists of walking support and progressive training. A special place in therapy is occupied by the elimination of complications. With the help of a physiotherapist, special exercises are performed to strengthen the muscles and prevent overexertion. Additionally, the following treatment methods are used:
- manual;
- isokinetic;
- isotonic;
- isometric.
During active therapy, it is necessary to learn the correct use of aids, including prostheses that compensate for weak muscle function. The therapist also teaches proper behavior at home, which reduces the risk of falls and household injuries and allows you to safely cope with everyday activities.
Diagnostics
The primary symptoms of polyneuropathy are identified by a neurologist during the examination of the patient. The next stage of diagnosis is laboratory tests. A child or adult is prescribed general clinical and biochemical blood tests, genetic and immunological tests. In some cases, a biopsy specimen is taken from a peripheral nerve. Histological analysis of the obtained material will allow doctors to determine the nature of damage to the nerve fibers.
Electromyography remains the key hardware method for diagnosing polyneuropathy. During the procedure, doctors examine the bioelectric potentials of the patient's muscles. EMG allows you to assess the intensity of the pathological process and exclude other neurological diseases from the history of a child or adult.
Treatment
Therapy for hereditary forms of polyneuropathy is symptomatic. Autoimmune disorders are brought into remission. Diabetic, alcoholic and uremic types of pathology require a combination of drug therapy and exercise therapy. Against the background of diphtheria polyneuropathy, patients are prescribed artificial ventilation.
Modern pharmacology cannot offer people suffering from polyneuropathies drugs that effectively eliminate damage to the cylindrical processes of nerve cells or myelinated nerve fibers. Palliative therapy includes vitamin complexes and neurotrophic agents.
Treatment of porphyritic polyneuropathies involves the use of glucose and painkillers. In the demyelinating form of the disease, patients are prescribed membrane plasmapheresis, supplemented by immunoglobulin injections. If they are insufficiently effective, doctors use glucocorticosteroids - prednisolone or its analogues.
Treatment of diabetic polyneuropathy of the lower extremities is carried out not only by a neurologist - the patient needs to consult an endocrinologist. For severe pain, men and women receive tricyclic antidepressants, pregabalin and gabanetin.
The symptoms of toxic polyneuropathies become less obvious when contact of a child or adult with the toxin is excluded. In case of drug intoxication, the doctor adjusts the daily dose received by the patient.
Surgical intervention against the background of polyneuropathy is performed when there is deformation of the feet and the development of joint contractures. In this case, the patient will face a long period of rehabilitation. To treat uremic polyneuropathy, a child or adult may require a kidney transplant.
Symptoms of toxic polyneuropathy
Depending on the conditions of exposure, the structure of the toxic substance, and its neurotoxic potential, pathological processes in polyneuropathy occur acutely, subacutely or chronically. A manifestation of an acute neurotoxic effect is a violation of the conduction of nerve impulses along motor and autonomic fibers and blockade or distortion of incoming sensory information.
In polyneuropathies - clinical syndromes characterized by diffuse damage to peripheral nerve fibers, the unit of damage is the fibers that are part of various nerves. The likelihood of damage depends on their length, caliber, and metabolic rate. Clinical manifestations of polyneuropathies - widespread, symmetrical, usually distal and progressive lesions - vary widely. They differ in the rate of progression, severity of symptoms, the ratio of sensory and motor disorders, and the presence of irritation symptoms.
Toxic polyneuropathy of the lower extremities begins with paresthesia (a crawling sensation) and pain in the feet, then in the hands. The intensity of the pain quickly becomes unbearable. In some patients, the tip of the nose and ears are involved in the process. They are worried about pain in the teeth and itching of the gums in the upper jaw, and short-term nasal congestion.
The process of polyneuropathy spreads from bottom to top: on the lower extremities - to the knee joints, on the upper extremities - to the shoulder girdle. First, damage to the lower extremities is detected. Neurologists diagnose the extinction of the Achilles reflex and sensory disturbances in the form of “socks”. Then flaccid paralysis develops with gradual extinction of reflexes. Knee and abdominal reflexes are preserved, sometimes strengthened, and symmetrical. Patients develop a fear of pain from touching objects, which leads to a forced position of their legs and arms. The following symptoms are noted:
- pain upon palpation of the skin of the extremities and upon pressing on the exit points of the second branch of the trigeminal nerve;
- hyperesthesia (increased sensitivity of the skin) like high socks and stockings;
- impairment of proprioceptive sensitivity (sense of the position of parts of one’s own body relative to each other and in space);
- decreased muscle tone and strength;
- hypotrophy (loss of mass) of the muscles of the limbs.
As the disease progresses, swelling of the feet and lower third of the legs and hands appears. Some patients with toxic polyneuropathy develop trophic ulcers and skin irritation due to the fact that, in an attempt to relieve pain, they take cold water baths for the extremities. Other patients experience atrophic changes in the skin of the hands. Sometimes the epidermis of the hands and feet exfoliates, hyperkeratosis (excessive growth of the stratum corneum of the epidermis) and mosaic pigmentation. Appetite decreases, sleep is disturbed, and severe neurosis develops. There is pallor of the skin of the face and moderate tachycardia (increased heart rate).
Peripheral neuropathy is sometimes caused by drugs:
- chloramphenicol;
- colistin;
- phenelzine;
- ergotamine.
Mixed sensory-motor polyneuropathy develops as a result of uncontrolled intake of ethambutol, isoniazid, metronidazole, streptomycin, chlorpropamide. Motor polyneuropathy is mainly caused by amphotericin B, sulfonamides, amitriptyline, cimetidine, and tetanus toxoid. Neurotoxicity is one of the side effects of drugs for the treatment of malignant neoplasms and immunosuppressants. Polyneuropathies often occur in acute and chronic intoxication with metals and salts of arsenic, tin, thallium, and zinc vapor.
Neurologists at the Yusupov Hospital make a diagnosis of toxic polyneuropathy based on a characteristic medical history, clarification of the cause of chronic intoxication, and neurological examination data. An electroencephalogram, ECG, Doppler study of cerebral vessels are performed and the diagnosis is confirmed by the results of electroneuromyography.