Multiple sclerosis
(MS) is a chronic, incurable autoimmune disease. Pathological processes (demyelination) affect the myelin sheaths of neurons in the brain and spinal cord. Healthy tissue is replaced by dense connective tissue, the scar type. It does not conduct nerve impulses, which leads to various neurological symptoms.
Diagnosis of multiple sclerosis at the initial stage of the disease is difficult. It is important to have complete, regular medical checkups. In this case, it is possible to detect the onset of the disease and begin timely treatment. This will help to significantly slow down pathological changes and prolong the patient’s ability to work for a long time.
tests
Causes of multiple sclerosis
At the moment, the exact cause of the disease has not been established. Some of the most likely factors influencing the development of MS are:
- previous viral or bacterial infections;
- prolonged exposure to increased radiation fields;
- chronic poisoning with toxic substances;
- poor quality, inadequate nutrition;
- unfavorable environmental conditions;
- previous injuries;
- frequent stressful situations.
According to statistics, the disease most often occurs at a young age, under 40 years of age. However, it is rare, but still occurs both in children under 15 years of age and in older people. It is more often diagnosed in females; there are female patients for every male. Not only gender matters, but also race. Caucasians are more prone to multiple sclerosis.
The incidence is higher in large, industrial cities, which may indicate the influence of unfavorable environmental conditions and stress. Russia is a high-risk zone, since more than 30 patients are diagnosed here for every 100 thousand people.
About multiple sclerosis
Pregnancy and multiple sclerosis
Treatment of multiple sclerosis during pregnancy, childbirth and the postpartum period.
According to medical instructions, none of the modern drugs are approved for use during pregnancy. Therefore, a couple who decides to have children should consult with their treating neurologist in advance.
Effect on fertility
Multiple sclerosis does not affect fertility or fertility, the incidence of spontaneous abortions, missed abortions, or congenital anomalies. Data from several large prospective studies showed that complications during pregnancy and childbirth, as well as the incidence of complications in the fetus, did not exceed those for women without the disease.
Effect on exacerbations of MS.
Exacerbations during pregnancy occur less frequently and are usually not serious.
Childbirth and MS
The choice of delivery method depends on a large number of factors, and in many cases MS is not the main one. Women with weakness or increased tone in the legs may have difficulty pushing, which requires increased work of the skeletal muscles. Therefore, the decision on choosing a method of delivery should be made jointly by the patient, the attending physician, obstetrician-gynecologist and neurologist.
Course after the birth period
The frequency of exacerbations increases in the first 3-6 months after pregnancy, which is associated with hormonal changes in the woman’s body. Some studies even report a higher risk of exacerbations during this period than before pregnancy. Overall, research data indicate a 20-40% risk of exacerbations during this period. However, these exacerbations and pregnancy in general do not affect the risk of long-term progression, either for the better or for the worse.
Lactation and MS
Expert opinions on the role of breastfeeding on MS activity differ. However, breastfeeding reduces the risk of various diseases in the newborn. In one study, the risk of MS exacerbations was significantly lower in women who exclusively breastfed their babies for 2-6 months, compared with women who did not breastfeed at all. Disease activity leveled off in these groups after 6 months with the introduction of complementary foods and the resumption of the menstrual cycle.
Oral contraceptives and MS
Taking oral contraceptives does not significantly affect the course of MS.
Treatment of exacerbations during pregnancy and breastfeeding
Corticosteroids can be used to treat exacerbations during pregnancy without significant risk to the fetus. These drugs are metabolized before passing through the placenta.
Manifestation of multiple sclerosis
Symptoms depend on the location of the most severe demyelination.
1. If the pyramidal system is damaged:
- Increased tendon-periosteal reflexes that occur in response to stimuli.
- Decreased muscle strength and increased muscle fatigue while maintaining functionality.
- Tetraparesis is increased tone of a particular muscle group.
2. With damage to the cerebellum:
- Ataxia (impaired coordination of movements) of the trunk and limbs.
- Intention tremor (vibrations of the whole body or its parts due to uncontrolled muscle contractions).
- Muscular hypotonia (decreased muscle tone and strength up to paresis).
3. When neurons are damaged, paralysis of the following nerves may occur:
- facial;
- oculomotor;
- sublingual;
- trigeminal nerve.
4. Other symptoms of MS:
- bulbar and pseudobulbar syndromes;
- nystagmus - involuntary eye movements;
- joint and muscle pain;
- loss of tactile sensitivity;
- a feeling of pressure in the limbs;
- superficial tingling in the fingers;
- incontinence and retention of urine and bowel movements;
- sexual dysfunction;
- decreased visual acuity and quality (loss of brightness, distorted color perception).
Neuropsychological changes are also observed in multiple sclerosis. They consist in changing habits, reducing mental abilities, resulting in specific organic dementia. Patients suffer from depression, alternating with periods of euphoria, and often lose control of their emotions. Emotional instability, i.e. rapid changes in mood, which is considered one of the early symptoms. To assess the severity of symptoms, a scale from 0 to 6 is used, and the degree of disability of a patient with MS is scored from 0 to 10 on the EDSS scale.
Multiple sclerosis
Multiple sclerosis is a disease in which the human immune system destroys the special membrane of nerve cell processes. This disrupts the conduction of nerve impulses in the brain and spinal cord, causing weakening of the arms and legs, deterioration of vision, dizziness, etc.
The disease develops 2 times more often in women than in men. The first signs of the disease appear between the ages of 20 and 40 years. Symptoms of multiple sclerosis gradually intensify, leading to profound disability. At the same time, periods of improvement and deterioration of the patient’s condition alternate. Multiple sclerosis can sometimes be difficult to diagnose, especially in the early stages. Treatment is aimed at reducing the severity of the disease. There are no treatment methods to achieve complete recovery.
Synonyms Russian
Multiple sclerosis.
English synonyms
Multiple sclerosis, disseminated sclerosis, encephalomyelitis disseminate.
Symptoms
- Decreased visual acuity, double vision. Sometimes there is pain when moving the eyes.
- Decreased muscle strength. May occur in one arm or leg and then spread to the opposite side.
- Numbness, tingling in the torso, arms, legs.
- Loss of coordination, balance, dizziness.
- Incontinence or retention of urine and stool.
- Trembling in the arms or legs.
- General fatigue, weakness.
- Decreased memory and attention.
General information about the disease
Multiple sclerosis is one of the causes of profound disability in young and middle-aged people. It occurs as a result of the destruction of the membrane of nerve cell processes, which is called myelin. Myelin helps insulate nerve fibers. If its structure is damaged, the transmission of nerve impulses in the brain and spinal cord is blocked or significantly disrupted, causing manifestations of the disease. The destruction of this membrane occurs when it is exposed to cells of the body's immune system. There are theories according to which the disease develops mainly in people who have defects in the functioning of the immune system. When the human body is exposed to certain infections, immune cells not only begin to destroy the causative agent of this infection, but also have a damaging effect on their own nerve cells, destroying their membrane. Multiple sclerosis lesions form in the brain and spinal cord. Such areas of the brain cannot function normally, which leads to the disease.
During the course of the disease, there are episodes of significant improvement, so-called remissions. Symptoms of the disease weaken or disappear altogether, and this allows patients to return to a normal lifestyle for a while. Exacerbations of multiple sclerosis are also observed, when the manifestations of the disease can significantly intensify.
One of the factors that negatively affects the condition of patients is an increase in body temperature. With multiple sclerosis, even a hot bath can cause increased weakness in an arm or leg. This occurs because the conduction of nerve impulses along damaged nerve cell processes deteriorates as the temperature rises.
Over time, the disease progresses.
Among the factors that cause multiple sclerosis are:
- genetic factors – predisposition to the disease is inherited;
- infections of the brain and spinal cord.
Scientists have found that multiple sclerosis is more common in countries with temperate and cold climates; in countries with hot climates, the incidence is lower.
Who is at risk?
- Persons whose close relatives suffer from multiple sclerosis.
- Women.
- Persons aged 20 to 40 years.
- Patients with infectious diseases.
- Living in countries with temperate and cold climates.
Diagnostics
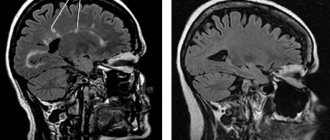
Diagnosis of multiple sclerosis is based on identifying the characteristic manifestations of the disease and excluding diseases that have similar symptoms. An important role is played by magnetic resonance imaging of the brain and spinal cord, which allows one to obtain images of the internal structures of the body. In multiple sclerosis, brain scans show multiple areas of brain damage (although they can also be caused by other diseases).
To clarify the diagnosis, laboratory tests are performed.
- Diagnosis of multiple sclerosis (isoelectric focusing of oligoclonal IgG in cerebrospinal fluid and serum). Liquor washes the brain and spinal cord. In multiple sclerosis, oligoclonal immunoglobulin G is detected in it, which indicates the effect of the immune system on the brain. Immunoglobulins arise in response to exposure to infections. Accordingly, the detection of this type of immunoglobulin in blood serum indicates the action of the immune system against its own cells.
- Complete blood count (without leukocyte formula and ESR). An increase in the number of leukocytes in the blood and erythrocyte sedimentation rate indicates an inflammatory process (multiple sclerosis can develop when the body is exposed to infections).
- Analysis of cerebrospinal fluid for protein, glucose - changes in these indicators are observed in diseases of the brain and spinal cord.
Additional Research
- The evoked potential method is based on the study of electrical reactions of the brain and spinal cord in response to irritation of the muscles of the arms, legs, torso, eyes, and hearing organs. This makes it possible to measure the speed of propagation of nerve impulses and assess the safety of signal transmission along nerve endings.
Treatment
Treatment of multiple sclerosis consists of reducing the severity of existing symptoms and achieving a stable condition of patients in the periods between exacerbations of the disease.
There are no methods to achieve a complete cure.
Adrenal hormones (corticosteroids) are used. They help reduce inflammation in lesions of the brain and spinal cord. Various drugs are also used that reduce the activity of the human immune system - this slows down the destruction of the membrane of nerve endings.
In addition, there are many medications available to treat specific symptoms of multiple sclerosis.
Prevention
There is no prevention for multiple sclerosis. When already in
Diagnosis of multiple sclerosis
The disease does not have characteristic symptoms unique to it. Therefore, differential diagnosis is always carried out. The doctor needs to rule out a large number of congenital pathologies and diseases of the nervous system. Systemic lupus, stroke, Sjogren's syndrome, Parkinson's and Behçet's diseases have similar changes.
1.
Laboratory diagnostics
When conducting a general blood test, changes in indicators allow one to suspect the development of multiple sclerosis. These include:
- Concentration of lymphocytes - increased content up to 40% or more.
- The number of leukocytes is less than normal.
- Erythrocyte sedimentation rate is increased.
A cerebrospinal fluid puncture will help check for an autoimmune disorder. In MS, a high percentage of immunoglobulins and oligoclonal antibodies (IgG antibodies) will be detected in it.
You can analyze the state of the immune system by doing an immunogram. To do this, it is necessary to donate venous blood for a comprehensive study. It is aimed at identifying the concentration of lymphocytes and immunoglobulins of various types. As a rule, with RSV, the concentration of immune cells is increased, indicating an autoimmune process, and other parameters are decreased, as a result of weakened body defenses.
2. Instrumental diagnostics
The most effective at the moment is considered to be an electromagnetic superposition scan of brain structures (SEMS) or an electroencephalogram. The scan allows you to diagnose multiple sclerosis at an early stage of development, when neurological signs are absent or mild. However, SPEMS has a high error; changes are detected in one case out of three.
The essence of the method is to identify focal losses of myelin. In the presence of pathological changes, the conduction of nerve impulses is disrupted. It is carried out by placing several sensors that monitor bioelectric impulses on the patient’s head. The result is an electroencephalogram - a graphic image of an oscillatory electrical process.
3. Magnetic resonance and computed tomography
Computer and magnetic resonance diagnostics make it possible to assess the state of the nervous system and diagnose MS. The use of a contrast solution helps to increase the efficiency of the study. The drug is administered intravenously and does not cause any sensations or discomfort.
The sensitivity of tomography is extremely high, reaching an accuracy of 95%. Allows you to accurately diagnose multiple sclerosis in the following cases:
- detection of 4 or more foci of demyelination;
- diameter of damage to nerve fibers from 3 mm;
- the lesions are located in the nerve fibers, in the cranial fossa, adjacent to the lateral stomachs.
A contrast solution not only helps to increase visibility, but is itself a marker of the presence of pathology. Its accumulation in the lesions indicates an active inflammatory process. A tomogram of the spinal cord is performed in the same way.
Early diagnosis of multiple sclerosis
About the article
32882
0
Regular issues of "RMZh" No. 5 dated March 10, 2010 p. 224
Category: Neurology
Author: Schmidt T.E.
For quotation:
Schmidt T.E. Early diagnosis of multiple sclerosis. RMJ. 2010;5:224.
Multiple sclerosis (MS) is the most common disease of the central nervous system in young people. In the vast majority of cases, at the onset of the disease, the course of MS is remitting, when periods of manifestation of various symptoms are replaced by phases of complete well-being or significant improvement in condition. However, over time, the disease begins to steadily progress and almost inevitably leads to significant disability in patients. Until recently, there were no medications that could significantly affect the course of MS. The last two decades have changed the idea of this disease as incurable. This happened in connection with the introduction into clinical practice of immunomodulatory drugs - beta interferons (Betaferon, Rebif, Avonex) and glatiramer acetate. Immunomodulatory therapy can significantly reduce the number of exacerbations of MS and slow down the increase in disability in patients. Currently, it is customary to prescribe immunomodulatory therapy immediately after diagnosis, since delayed administration of treatment reduces its effectiveness. In this regard, it is obvious that correct diagnosis at the earliest stages of the disease is important. Despite the fact that there are now additional research methods such as MRI (magnetic resonance imaging) and evoked potentials (EP) studies, approximately half of patients are correctly diagnosed only 5 years after the onset of the disease, and this time for treatment is missed. In addition, approximately every 10th patient is misdiagnosed with MS, and vice versa - in 4-5% of cases, MS patients first receive a different diagnosis. Diagnosis of MS remains primarily clinical, which requires “dispersal of symptoms in space and time.” In other words, in the classical version, reliable MS is characterized by the development of various manifestations over different periods of time. In this case, a new exacerbation may repeat the clinical picture of the previous one, but may also occur with completely different symptoms. In such cases, diagnosis (taking into account these additional examination methods) is usually not difficult. However, at the onset, the disease can manifest itself with the appearance of only one symptom or syndrome - the so-called monofocal clinically isolated syndrome (CIS).
A classic example of such a syndrome is retrobulbar neuritis (RBN). It is manifested by subacute, usually unilateral and incomplete loss of vision, which is often preceded by pain, which can be localized in the eye itself, above the orbit or in the face, and intensifies with pressure on the eyeball. Naturally, a patient with similar symptoms turns to an ophthalmologist. It is important to remember that RBN in MS is accompanied by pain during eye movements, disturbances in pupillary reactions (in the affected eye, the friendly reaction to light is more pronounced than the direct one) and partial loss of the visual field. Patients describe it as a “spot in front of the eye.” With RBN, patients complain of blurred vision, a feeling of fog before the eyes, impaired color vision (objects appear paler), and impaired three-dimensional vision. Subsequently, complete or partial restoration of vision occurs. Factors that increase the risk of developing MS after RBN are: young age, repeated attacks of RBN, female gender. Every patient with RBI should be referred for an MRI of the brain. The risk of developing MS after isolated RBN if characteristic changes are detected during MRI is 70–80%. Isolated bilateral RBI as a manifestation of MS is very rare. In these cases, one should keep in mind Leber's disease - a hereditary optic neuropathy, transmitted through the maternal line, but affecting exclusively men. MRI reveals intraocular optic nerve damage rather than retrobulbar damage as in MS. In all cases of optic neuritis, the lack of effect of corticosteroid therapy requires differential diagnosis with Leber's disease. Electroretinography is required to confirm the diagnosis of Leber's disease. Acute bilateral RPN should also be differentiated from toxic and drug-induced optic neuropathy. The first is most often caused by methyl alcohol poisoning, and in this case the diagnosis usually does not cause difficulties, since visual disturbances are combined with damage to internal organs, and there are corresponding anamnestic data. With timely and adequate treatment, complete restoration of vision is possible. Medications, in case of overdose, long-term use or increased individual sensitivity, can also cause various visual impairments - loss of the central visual field (tranquilizers, antibiotics, digoxin) or narrowing of visual fields (acetylsalicylic acid, quinine). When the drug is discontinued, vision is quickly and completely restored. RBN can also be observed in systemic lupus erythematosus, neuroborreliosis, sarcoidosis, Sjogren's syndrome, neurosyphilis, AIDS, which must be taken into account in differential diagnosis. This requires a thorough somatic and laboratory examination. Another common onset symptom of MS is urinary disturbance, which forces patients to consult a urologist. Since among all the causes of urinary disorders, the most common is a urinary tract infection, first of all, to exclude it, it is necessary to conduct a urine test. In MS, the most common symptoms are urinary urgency—a sudden urge to empty the bladder that the patient cannot control for any length of time—and urinary incontinence. In more advanced stages of MS, such manifestations are often combined with difficulties emptying the bladder. When assessing urinary disorders, it should be remembered that in patients with MS, especially in middle and old age, they can be caused by prostatic hyperplasia in men, stress and menopausal urinary incontinence in women, etc. The patient should be asked about the frequency of daytime and nighttime urination, the degree of bladder emptying, and the ease of urination. Many patients with urinary urgency limit fluid intake, which leads to increased urine concentration and can cause symptoms of urinary tract irritation. Possible iatrogenic causes should also be excluded - in particular, the influence of drugs that have an anticholinergic effect and, therefore, can cause urinary retention. If all these causes are excluded, the patient should be referred to a neurologist. The first manifestation of MS can be such a very nonspecific syndrome as general fatigue. This syndrome is often underestimated by both others and doctors and is often mistaken for a “whim” or a manifestation of “neurosis.” Fatigue in MS differs from normal fatigue in healthy people in that it is inadequate to physical activity and disrupts normal daily activities. Patients describe it as a constant feeling of fatigue, loss of energy, and exhaustion. Fatigue in MS is significantly worsened in the heat, when taking a hot bath, while cold brings relief. Such a dependence on temperature influences is a characteristic feature of fatigue in MS; it is not observed in the presence of this symptom in systemic lupus erythematosus or neuroborreliosis. Pain, sleep disturbances, depression, as well as concomitant infectious diseases can increase fatigue and accompany it. On the other hand, constant fatigue itself can lead to the emergence of new symptoms - the development of depression and sexual dysfunction. To objectify fatigue, there are special tests and various questionnaires that allow patients themselves to evaluate this symptom. As a rule, even at this stage of the disease, a neurological examination can reveal some focal symptoms - nystagmus (involuntary twitching of the eyeballs when looking straight or with tracking eye movements), loss of superficial abdominal or plantar reflexes. It should be noted, however, that the disappearance of superficial abdominal reflexes is sometimes given unjustifiably great importance. It must be remembered that these reflexes are not evoked in 20–30% of healthy people, as well as in cases of various damage to the abdominal wall (stretching after repeated childbirth, postoperative scars). It is important to note that deep abdominal reflexes, in the absence of spinal cord involvement at the corresponding level, are preserved in MS. Babinski's symptom - a pathological foot reflex - in contrast to the “loss of” superficial abdominal reflexes, is an undoubted evidence of involvement of the pyramidal tract in the process and often, especially in the early stages of MS, serves as an important diagnostic sign. At the onset of MS, oculomotor disturbances are also common. Eye movement disorders leading to double vision occur in every 10th patient at the onset of MS. If double vision is accompanied by nystagmus, especially in one eye, one should first think about MS, since monocular nystagmus is an almost pathognomonic symptom of this disease. Sensory impairment is one of the most common symptoms at the onset of MS. In the early stages of the disease, sensitivity disorders are short-lived, lasting from several hours to several days. As a rule, they are manifested by a transient feeling of numbness, tingling, or “pins and needles” in various parts of the body. Especially often, these sensations occur in the tips of the toes or hands, then spreading proximally. This often gives rise to the erroneous diagnosis of polyneuropathy. However, in contrast to it, where sensitivity is impaired in a “socks” or “gloves” manner, in MS, sensitivity disorders are “spotty”; areas of impaired tactile and pain sensitivity appear. Sensory disorders can also be conductive in nature, but a clear boundary of sensory disorders and complete loss of sensitivity, so characteristic of spinal tumors, are rare. Quite often with MS, patients report that a feeling of numbness, starting in the legs, has risen to the level of the chest, and they have a feeling of tightness or “wearing a corset.” If sensory disturbances are the only symptom, they usually go away on their own within 1–2 months. MS should also be suspected if the patient complains that when he tilts his head, he has a sensation of electric current passing through the spine with irradiation to the legs or arms (Lhermitte's symptom). Usually this symptom disappears on its own after a few months, is not accompanied by pain and does not require treatment. It is so characteristic of MS that it was previously considered pathognomonic for it. The same sensations can occur with cervical myelopathy, however, in this case, Lhermitte’s symptom more often occurs when throwing the head back. In 11% of cases, the first symptom of MS is pain; it is more common when the disease begins at a later age and in women. Pain syndromes in MS can be divided into neuropathic, somatogenic, viscerogenic and psychogenic. For the onset of MS, neuropathic pain is most common, and among them is dysesthesia. They are described by patients as constant discomfort, a symmetrical or asymmetrical burning sensation, most often in the distal parts of the legs. Some MS patients suffer from paroxysmal facial pain called trigeminal neuralgia. About 2% of all patients with trigeminal neuralgia are patients with MS. This type of pain syndrome is 300 times more common in MS than in the general population. Unlike idiopathic trigeminal neuralgia, it can be bilateral and be accompanied by decreased sensitivity in the area of innervation of the nerve (trigeminal neuropathy). If trigeminal neuralgia develops in a patient under 40 years of age, it is necessary to exclude MS, among other diseases. Occasionally, with MS, very intense, short-duration pseudoradicular pain in the extremities may occur, which prompts one to look for the cause in damage to the spine and compression of the spinal cord roots. However, the localization of these pains does not correspond to the zones of innervation of the roots. They may represent a partial variant of Lhermitte's sign. Headaches in MS are a special subgroup: they are very common, although their cause remains unclear, and in MS they occur 3 times more often than in other neurological diseases. Rarely, headache may be the first sign of a developing disease. Usually such pains have the character of tension headaches. MS can also begin with motor impairments, which is a poor prognostic sign, as it predicts a more severe course of the disease in the future. Typically, muscle weakness occurs first in both legs. Less commonly, weakness develops in one leg or in a leg and arm on the same side. Affection of only one arm in MS is extremely rare. Very characteristic of MS is a noticeable worsening of weakness when exposed to temperature - taking a hot bath, prolonged exposure to the sun, fever (Utgoff's symptom). The “hot bath sign” is an important diagnostic criterion for MS. Motor disturbances in MS increase gradually; rapid development of motor dysfunction is not typical for the onset of the disease. The sudden development of paresis forces differential diagnosis with vascular disorders. As a rule, patients with MS initially feel only increased fatigue, which over time transforms into permanent muscle weakness. Isolated systemic dizziness (without brainstem symptoms) as the first manifestation of MS is rare. In such cases, it is mistaken for banal vestibulopathy. Meanwhile, an indication of the presence of an episode of systemic dizziness in the anamnesis can help in establishing the diagnosis of MS and determining the time of onset of the disease. The onset of MS with dizziness is a relative sign of a fairly favorable course of the disease in the future. It should be noted that dizziness in idiopathic vestibulopathy is usually much more pronounced than in cases where it is a manifestation of MS. The combination of systemic dizziness with other signs of involvement of the brain stem often gives rise to incorrect diagnosis of circulatory disorders in the vertebrobasilar system. In MS, emotional and personal disturbances are also common. The most common affective syndrome in MS is depression. Confirmation that depression can be an independent symptom of MS is its significantly higher frequency in this disease than in the population and in other severe neurological diseases. For example, with amyotrophic lateral sclerosis, depression is observed 3 times less often, and with myodystrophies - 4 times less often than with MS. Manifestations of depression in MS consist predominantly of irritability and frustration, in contrast to the feelings of guilt and hopelessness characteristic of depression in patients without MS. In some cases, the debut manifestations of MS may be anxiety disorders and manic states. Acute psychotic disorders in MS are rare. However, in 5–7% of cases, the onset or exacerbation of MS can manifest as psychosis. Their variations are possible from short episodes to long-term disorders with productive symptoms, which in some cases necessitates a differential diagnosis with schizophrenia. Epileptic seizures are much more common among people with MS than in the general population, where their frequency is only 0.4–2%. In the general population, the peak incidence of epilepsy occurs in childhood, adolescence, and then old age, and in patients with MS, seizures develop more often at the age of about 30 years. Epileptic seizures are usually partial (in 2/3 of cases), with possible secondary generalization. In some cases, MS debuts with the development of seizures. In half of the cases, however, epileptic seizures in MS are a manifestation of epilepsy as a separate concomitant disease. Thus, the initial manifestations of MS are very diverse, which forces patients in its debut stage to consult doctors of different specialties - ophthalmologists, urologists, psychiatrists, etc. Often, turning to neurologists does not lead to a correct diagnosis. It is important to remember all the possible first symptoms of MS and, if there is the slightest doubt about the diagnosis, refer patients to a neurologist for additional research methods - MRI and evoked potentials - in order to identify subclinical signs of the disease. The presence of multiple hyperintense foci on MR tomograms in T2 mode and changes in several modalities of evoked potentials serve as confirmation of “dispersion of the pathological process in space,” and the accumulation of contrast agent only in some foci during MRI in T1 mode is confirmation of “dispersal in time.” After this, the patient should be referred to a neurologist who specializes in MS or to an MS center (similar centers have now been created in almost all regional cities) to prescribe adequate treatment. The treatment of MS can include relief of exacerbations, symptomatic therapy and treatment aimed at reducing the frequency of exacerbations (immunomodulatory therapy). The latter is currently receiving a lot of attention, since each subsequent exacerbation leads to a deterioration in the patient’s condition and the “accumulation” of irreparable changes in the central nervous system. All immunomodulators that exist today are very expensive, but thanks to the state program for providing medications to MS patients, most of those in need today have the opportunity to receive them. The use of immunomodulators should be long-term, almost lifelong and continuous. All currently registered drugs are injectable and are administered subcutaneously or intramuscularly with varying frequencies (depending on the prescribed drug), from 1 time/week. before daily administration. Immunomodulatory treatment may be accompanied by various adverse events. Local reactions in the form of redness and thickening at the injection sites are common. To avoid this, rotation of injection sites should be used. For beta interferons, the most common side effect is the development of a flu-like syndrome in the form of general malaise, fever, headache, muscle pain, which usually occurs at the beginning of treatment, and decreases and disappears over time. To level them out at the beginning of treatment, it is recommended to carry out injections at night and take ibuprofen or paracetamol an hour before administering the drug. When treated with glatiramer, in addition to local ones, general post-injection reactions are possible in the form of general hyperemia, a feeling of lack of air, chest tightness, and palpitations. These phenomena are essentially a vegetative crisis and do not require any drug correction. However, patients should be warned about the possibility of developing such symptoms. The use of beta interferons also requires monitoring of liver enzymes and thyroid hormones. The key to the effectiveness of immunomodulating therapy is its continuity. That is why it is very important at the initial stage of its use to explain to the patient that this treatment is not aimed at stopping a particular symptoms, but at a decrease in exacerbations and slowing down the development of the disease, as well as help him cope with unwanted phenomena. In the future, several new drugs are expected to treat RS. Thanks to the appearance of tablet drugs, the possibility of a more comfortable treatment for RS that is not associated with injections will be possible. Timely and accurate diagnostics of the RS allows you to start preventive therapy in time, which, along with the patient’s understanding of the complexity of his disease, accurately fulfilling the doctor’s prescription and overcoming the possible side effects of therapy, can significantly inhibit the development of severe neurological disease, which is the RS. Help in this complex process is the duty of doctors of all specialties that such a patient can potentially contact.
Content is licensed under a Creative Commons Attribution 4.0 International License.
Share the article on social networks
Recommend the article to your colleagues
Treatment
Multiple sclerosis
This is a chronic disease, the complete cure of which is impossible. All measures are aimed at slowing the progression of the disease, relieving symptoms and reducing the frequency of exacerbations. There is no single treatment plan; each patient requires an individual approach.
The remitting nature of the disease, characterized by periods of weakening and intensification of symptoms, requires symptomatic treatment, prevention of exacerbations, and inhibition of the transition to the active stage. In the secondary, progressive form, the main goal of therapy is to slow the development of sclerosis. The doctor must understand what stage the patient is in. to correct his condition. To do this, the patient regularly undergoes prescribed tests, undergoes research, most often an MRI and an immunological blood test.
Do not forget that in addition to physiological symptoms, the patient undergoes a psychological personality change. May become depressed, experience chronic fatigue, anxiety and depressive disorders. Multiple sclerosis is associated with a wide range of mental disorders: from personality disorders to altered psychotic states. This also requires attention from a doctor.
Main objectives of treatment:
- Prevent exacerbations.
- Slow down the course of the disease.
- Prevent the development of new symptoms and reduce their severity.
- To alleviate the current symptoms, to help the patient lead his usual lifestyle.
An important role is played by the patient’s social adaptation and timely psychological assistance. Despite the fact that the diagnosis of multiple sclerosis is made by a neurologist, a number of specialists are involved in the treatment: an immunologist, an electrophysiologist, a neuro-ophthalmologist, a neuropsychologist, and a urologist.
TOP 8 signs of multiple sclerosis
Tingling in the fingers is one of the symptoms of multiple sclerosis
Multiple sclerosis is increasingly being diagnosed in people in their 20s and 30s. To detect this problem in a timely manner, take note of its first signs:
Bad memory: what to do to get rid of the problem?
- Vision problems.
It would seem, what is the connection between vision and memory?! The most direct! Therefore, if you notice that one eye sees worse than the other (and this has never happened before), immediately sound the alarm!
- Unpleasant sensations in the limbs.
A burning sensation in the legs and arms, strange “goosebumps” that occur for no particular reason, tingling and tightening of the skin - all this may indicate multiple sclerosis. Although most people don't pay any attention to it at all.
- Problems with urination.
You seem to be drinking the same amount of water as before, but for some reason you are going to the toilet less often. 80% of people who suffer from multiple sclerosis have problems urinating.
- Problems with movement coordination.
You used to ride the most extreme roller coasters and feel great afterwards, but now even a light jog can throw you off track? If you often experience loss of balance, blurred vision, or strange sensations while walking, you may have multiple sclerosis.
- Emotional condition.
If your mood changes a hundred times a day, you constantly think about bad things, feel emotional stress, it’s worth thinking about. It also often indicates multiple sclerosis.
- Speech problems.
Previously, you were one of the best speakers in your work team, but now you can’t put two words together? Or do you have difficulty swallowing? All this speaks about the problem of sclerosis.
- Tremor.
Trembling in your arms, legs, and other parts of your body may indicate that you are in the early stages of multiple sclerosis.
- Loss of sensation.
People who are faced with the disease often experience a strange loss of sensitivity. They can pick up snow in their hands, but not feel the cold. And next time, on the contrary, they will say that they are very cold.
Advantages of taking tests at JSC SZTsDM
- All types of laboratory tests, including those for diagnosing MS.
- Data accuracy thanks to modern equipment and qualified employees.
- Quick availability of results, several options for obtaining.
- Friendly staff, confidentiality, no queues.
- Convenient location of terminals.
The laboratories of the Northwestern Center for Evidence-Based Medicine are represented in Pskov, Veliky Novgorod, Kaliningrad, St. Petersburg and other cities of the Leningrad region.
Test: signs of multiple sclerosis
Prepared by: MedWeb
This serious disease, unlike the well-known sclerosis, affects the brain and spinal cord at a fairly early age (most often from 20 to 40 years). And therefore, in order not to join the ranks of the disabled so early, it is best to know and remember about the possibility of its occurrence. And the proposed test will just help you figure out whether you have already developed signs of this very “multiple sclerosis.”
multiple sclerosis, self-examination, diagnosis
For each “yes” answer you get 1 point, and for each “no” answer you get 0. So:
1. Are you worried about weakness in your limbs?
2. Are you increasingly experiencing dizziness when your blood pressure is normal?
3. Have you started to experience occasional blurred vision and double vision?
4. Do you feel tingling in your body?
5. Do you occasionally feel unsure when walking?
6. Have you started to notice tremor (shaking) of your limbs?
7. Do you have any speech difficulties?
8. Do you notice a loss of sensitivity in the limbs?
9. Do tests reveal that you have anemia?
10. Have you started to experience any sexual problems (weakness, decreased desire...)?
11. Have you noticed that you speak as if in syllables?
12. Do you start to sway when walking?
13. Have you started to worry about false urges to urinate?
- If you scored only from 2 to 4 points, and besides, your age is more than 45 or less than 18 years old, then, of course, you can and should be wary and even try to figure out why you have the symptoms you noted, however, it is unlikely that they will be the first signs of multiple sclerosis.
- If you have a score of 5 to 10, then this may indicate that, unfortunately, you already have quite obvious manifestations of the onset of multiple sclerosis. Urgently contact a neurologist and undergo the examinations prescribed by him. If, for some reason, you cannot do this at the moment, then at least start by excluding spicy foods and smoked foods from your diet; your food should be rich in trace elements of copper, zinc and manganese, which means it should include celery, spinach, peas, red beets, blueberries, lingonberries, black currants, oats and mushrooms. Follow the work and rest schedule. Take massage courses. Drink medicinal herbal mixtures: they should include St. John's wort, calendula flowers, juniper and rose hips, and hemp herb. In addition, you are shown the so-called phytoimmunocorrectors: aloe, kalanchoe, arnica, plantain, coltsfoot, skullcap, tricolor violet and string.
- Well, a score exceeding 10 clearly indicates that you have this serious, but, fortunately, practically non-fatal disease. If you have not yet consulted a specialist about this disease that is tormenting you, then under no circumstances should you put off this important matter! You already need active treatment with steroid hormones, beta-interferon, or (which is better) non-steroidal anti-inflammatory drugs such as biopolymer.
Author: Evgeniy Aleksandrovich TARASOV, Ph.D., psychotherapist of the highest category.