May 25, 2016
Rehabilitation massage after a stroke is one of the most important components of effective therapeutic interventions to restore full mobility and prevent some of the negative consequences of the disease. The need to use massage techniques, their frequency, beginning and duration of implementation is determined by the attending physician. In addition, he checks for contraindications and the general condition of the patient. To get high-quality and complete advice, it is better to turn to foreign specialists.
Medicine in Turkey is distinguished by its affordable pricing policy and high level of treatment for oncology, stroke and other complex diseases.
When can you start massage after a stroke?
It is advisable to start massage after a stroke as early as a person’s health allows. If the patient is in normal condition, then the procedure begins on the second day. They start with segmental and point massage. The flexion groups are massaged on the lower extremities, and the extensor groups are massaged on the upper extremities. In muscle fibers with higher tone (examples include flexors, fingers, hands, forearms and leg extensors), only light and slow stroking can be done. For antagonistic muscle fibers with unchanged tone, gentle kneading and rubbing at increased speed are used. The first massage sessions last for 5-10 minutes, with a gradual increase in time up to half an hour.
The treatment program includes at least 20-30 sessions, which are performed every day. After the first course is completed, a break of one and a half to 2 months is required, followed by the resumption of massage procedures. The massage should be done by an experienced physical therapy instructor, rehabilitation therapist or experienced massage therapist whose specialization includes this pathology.
Massage for spastic paralysis
Massage for spastic paralysis (as a result of spinal cord injury, acute cerebrovascular accident)
Objectives
1. Reducing the reflex excitability of muscles in a spastic state.
2. Strengthening paretic muscles.
3. Restoration of impaired motor functions.
4. Prevention of contracture formation.
5. Increase in general psychophysiological tone.
Starting points
1. Lying on your back, a cushion under the knee joints.
2. Lying on your stomach, a bolster under your ankle joints, a pillow under your stomach.
Procedure plan
1. Massage of the anterior surface of the lower limb.
2. Massage the anterior chest on the affected side.
3. Massage of the upper limb.
4. Massage of the back surface of the lower limb.
5. Massage the back area.
Methodological features of the technique
In the method of selective massage on muscles with increased or increasing tone, continuous planar and grasping stroking and rubbing are used, when massaging antagonists (hypotonic muscles) - plane deep, pincer-like and grasping intermittent stroking, as well as gentle transverse and longitudinal rubbing, light shallow longitudinal, transverse and forceps kneading. Vibration, patting, and tapping are contraindicated. When massaging muscles with increased tone, a slow pace should be used, and with decreased tone, a much faster pace should be used.
During a general massage, massage is first performed on the healthy side, and then on the affected side.
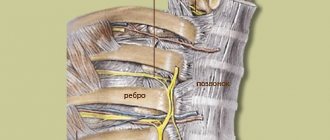
Massage of the extremities begins from the proximal parts and is carried out in the direction from the center to the periphery. First, spastic muscles are massaged, then hypotonic ones. Typically, increased tone is observed in the anti-gravity muscles: arm flexors (shoulder adduction, elbow and wrist flexion) and leg extensors (hip adduction, knee extension and ankle plantar flexion).
Before starting massage techniques, it is necessary to achieve a maximum reduction in muscle tone, their relaxation through shaking techniques, passive movements, warming the limb, rubbing the heel (Achilles) tendon, hamstring tendons, biceps brachii tendon.
In case of spastic paralysis due to significant muscle fatigue, the massage should not be long (initially from 5 to 10 and then from 15 to 20 minutes).
It is recommended to include passive movements for paretic limbs and basic breathing exercises in the massage procedure, as well as combine massage with therapeutic exercises, positional treatment and physiotherapeutic procedures. In combination with the “classical” massage technique, techniques and methods of acupressure and segmental reflex massage can be actively used.
Massage after a stroke: main tasks
The main goals for achieving massage after a stroke are:
- reduction of pain;
- improvement of well-being and mood;
- improving blood flow to all tissues, and therefore their supply with oxygen and nutrients;
- increased lymph flow in paralyzed parts of the body and throughout the body;
- preventing the development of congestive pneumonia in older people;
- preventing the formation of contractures;
- preventing the formation of bedsores;
- accelerating the process of restoring the functionality of the affected limbs.
Find out about check-up
2.1. Goals and objectives of massage
Peripheral paralysis is characterized by deeper functional disorders of the motor system than spastic ones.
For flaccid paralysis, a deep and moderately hard massage is performed. Objectives of massage for flaccid paralysis:
- improve blood and lymph circulation;
- reduce pain;
- help accelerate the regeneration processes of affected nerve fibers;
- strengthen paretic muscles;
- counteract the formation of contractures and deformities;
- increase muscle tone and strength;
- reduce their atrophy;
- promote movement restoration;
- improve and strengthen the general condition of the patient.
How to do a massage after a stroke?
For a full recovery of health, it is very important to know how to massage after a stroke correctly. In the first couple of months, you can perform exclusively local massage for paretic (partially paralyzed) and paralyzed (completely immobile) limbs, chest, lumbar area and other parts of the back.
General massage is performed only at the late rehabilitation stage. Long-term tissue stimulation in the early post-stroke period leads to fatigue, which only worsens the patient’s condition. During sessions, each zone is massaged several times (2-5). Massage begins with small areas of influence, without turning the patient onto his stomach. Often, stimulation begins with the thigh and shoulder area, after four procedures, if the patient’s health allows, the legs, forearms, hands, chest and feet are added.
By the 8th procedure, you can stimulate the lumbar area and back in the affected areas. The patient should lie on his healthy side. He is allowed to lie on his stomach only in the later stages of the massage, if there are no contraindications from the doctor due to cardiac pathologies. To increase the beneficial effect of massage and rehabilitation warm-ups, it is recommended to first warm the paralyzed limbs. To do this, you can use a reusable salt heating pad, compresses with ozokerite and paraffin. Increasing the intensity and expanding the impact zone are individual and are carried out strictly according to the decision of the attending physician, who monitors the general health indicators of the patient. In case of hemorrhagic stroke, massage begins no earlier than 5-7 days.
1.1. Etiology and pathogenesis
Peripheral paralysis is always a consequence of damage to peripheral motor neurons and occurs both with damage to the bodies of these neurons located in the motor nuclei of cranial nerves or in the anterior horns of the spinal cord segments, and their axons that are part of various structures of the peripheral nervous system, as well as during blockade neuromuscular synapses.
Selective damage to the bodies of peripheral motor neurons is characteristic, in particular, of epidemic poliomyelitis and amyotrophic lateral sclerosis. Damage to the structures of the peripheral nervous system can be a consequence of trauma, compression, infectious-allergic lesions, etc., leading to the development of radiculopathies, plexopathies, neuropathies, mono- or polyneuropathies. Failure of neuromuscular synapses, which transmit nerve impulses from the nerve ending to the muscle using the mediator acetylcholine-H, occurs with myasthenia gravis and botulinum toxin poisoning.
1.2. Clinic
Peripheral paralysis is characterized by the following main symptoms:
- muscle atony or hypotonia;
- areflexia or hyporeflexia (decreased tendon, periosteal, skin reflexes);
- amyotrophy;
- qualitative changes in electrical excitability of muscles (reaction of degeneration, or degeneration);
- fibrillar (rapid contractions of individual muscle fibers when irritating SC motor neurons) and fascicular (rapid contractions of muscle fiber bundles when irritating the anterior roots or motor fibers of nerve trunks) muscle twitching.
In addition, changes in electrical excitability, called the degeneration reaction, develop in paralyzed muscles and affected nerves. The depth of changes in electrical excitability allows one to judge the severity of the lesion in peripheral paralysis and the prognosis. Loss of reflexes and atony are explained by interruption of the reflex arc; such a break in the arc leads to loss of muscle tone. For the same reason, the corresponding reflex cannot be evoked. Muscle atrophy, or sudden weight loss, develops due to the disconnection of the muscle from the neurons of the spinal cord; from these neurons, impulses flow through the peripheral nerve to the muscle, stimulating normal metabolism in muscle tissue. With peripheral paralysis, fibrillar twitching may be observed in atrophied muscles in the form of rapid contractions of individual muscle fibers or bundles of muscle fibers (fascicular twitching). They are observed in chronic progressive pathological processes in the cells of peripheral motor neurons.
Damage to a peripheral nerve leads to peripheral paralysis of the muscles innervated by this nerve. In this case, sensory disturbances and autonomic disorders are also observed in the same area, since the peripheral nerve is mixed - motor and sensory fibers pass through it. As a result of damage to the anterior roots, peripheral paralysis of the muscles innervated by this root occurs. Damage to the anterior horns of the spinal cord causes peripheral paralysis of the muscles in the areas of innervation by this segment.
Thus, damage to the anterior horns of the spinal cord in the area of the cervical thickening (the fifth - eighth cervical segments and the first thoracic) leads to peripheral paralysis of the arm. Damage to the anterior horns of the spinal cord at the level of the lumbar enlargement causes peripheral paralysis of the leg. If the cervical or lumbar thickening is affected on both sides, then upper or lower paraplegia develops.
An example of peripheral limb paralysis is the paralysis that occurs due to polio. With polio, paralysis of the legs, arms, and respiratory muscles can develop. When the cervical and thoracic segments of the spinal cord are affected, peripheral paralysis of the diaphragm and intercostal muscles is observed, leading to respiratory failure. Damage to the upper thickening of the spinal cord leads to peripheral paralysis of the arms, and the lower (lumbar thickening) leads to paralysis of the legs.
Manifestations of peripheral paralysis in various syndromes:
Facial nerve syndrome: In children, inflammatory lesions of the facial nerve often occur, leading to peripheral paralysis of the facial muscles. On the side of the lesion of the facial nerve, the folds in the forehead are smoothed, the eyebrow is slightly lowered, the palpebral fissure does not close, the cheek hangs down, the nasolabial fold is smoothed, and the corner of the mouth is lowered. The patient cannot stretch his lips forward, blow out a burning match, or puff out his cheeks. When eating, liquid food pours out through the lowered corner of the mouth. Paresis of the facial muscles is most pronounced when crying and laughing. These disorders can sometimes be accompanied by lacrimation, increased sensitivity to auditory stimuli (hyperacusis), and taste disturbance in the anterior two-thirds of the tongue.
Less commonly, peripheral paralysis of the facial muscles is caused by underdevelopment of the nuclei of the facial nerve. In such cases, the lesion is usually bilateral and symmetrical; symptoms are observed from birth and are often combined with other developmental defects.
Bilateral damage to the facial nerve, most often its roots, can also be observed with multiple neuritis (polyneuritis), inflammation of the meninges (meningitis), fractures of the bones of the base of the skull and other skull injuries.
Oculomotor nerve syndrome: damage to the oculomotor and abducens nerves leads to paralysis of the muscles they innervate and the occurrence of strabismus.
in patients with damage to the oculomotor nerve, divergent strabismus occurs, since the healthy external rectus muscle, innervated by the abducens nerve, pulls the eyeball in its direction. When the abducens nerve is damaged, convergent strabismus develops for the same reason. When the trochlear nerve is damaged, strabismus, as a rule, does not occur. There may be a slight convergent squint when looking down. If the oculomotor nerve is damaged, drooping of the upper eyelid (ptosis) may occur due to paralysis of the muscle that lifts the upper eyelid, as well as dilation of the pupil (mydriasis) due to paralysis of the muscle that constricts the pupil, and impaired accommodation (deterioration of near vision).
With paralysis of the extraocular muscles, the eyeball may protrude from the orbit due to a decrease in their tone (exophthalmos). When looking to the side with a paralyzed muscle, double vision (diplopia) occurs.
Hypoglossal nerve syndrome: Damage to the hypoglossal nerve or its nucleus in the brainstem causes peripheral paralysis of the corresponding half of the tongue. Atrophy of the tongue muscles (thinning of the paralyzed half of the tongue), hypotonia (the tongue is thin, spread out, elongated), deviation of the tongue when it protrudes towards the paralysis, and fibrillary twitching are observed. Movement of the tongue in the affected direction is limited or impossible. Possible disturbance of sound pronunciation - dysarthria.
Accessory nerve syndrome: When the accessory nerve or its nucleus is damaged in the brain stem, peripheral paralysis of the sternocleidomastoid and trapezius muscles develops. As a result, the patient experiences difficulty turning his head to the healthy side and, if necessary, raising his shoulder. Lifting the arm above the horizontal line is limited. Shoulder drooping is observed on the affected side. The lower angle of the scapula extends from the spine.
Syndrome of combined damage to the glossopharyngeal, vagus and hypoglossal nerves (bulbar syndrome): with damage to the glossopharyngeal and vagus nerves, motor disorders are characterized by peripheral paralysis of the muscles of the pharynx, larynx, soft palate, trachea, tongue. This condition is called bulbar palsy. Paralysis of the muscles of the pharynx leads to difficulty swallowing. When swallowing, patients choke. Paralysis of the muscles of the epiglottis leads to the entry of liquid food into the larynx and trachea, and paralysis of the soft palate leads to the flow of food into the nasal cavity. Paralysis of the mouse larynx leads to sagging of the ligaments and to aphonia or hypophonia (the voice becomes silent). Due to the sagging of the soft palate, the voice may take on a nasal tone. The tongue deviates to the healthy side. Due to tongue paralysis, chewing is impaired. The tongue deviates to the affected side, its movements are difficult. Atrophy and hypotonia of the tongue are observed. There is a violation of sound pronunciation: bulbar dysarthria develops. The palatal and pharyngeal reflexes disappear. The vagus nerve provides autonomic innervation to blood vessels and internal organs (including the heart). Its bilateral defeat causes death due to cardiac and respiratory arrest.
In what sequence is massage performed after a stroke?
Massage after a stroke begins with stimulation of the anterior part of the affected lower limb, since with hemiparesis the legs suffer differently than the arms. After this, they move on to the pectoralis major muscle. The upper limbs are massaged in the following sequence: the shoulder, then the forearm, the tissues of the hand and only then the fingers. Back of the leg: thigh, lower leg, foot. Next, begin the back massage. Movements are performed in accordance with the flow of lymph. There are several types of massage techniques: gentle rubbing, superficial stroking and weak continuous vibration for spastic muscle fibers (shaking, shaking).
Spastic muscles include:
- chest;
- the inner (front) surface of the shoulder, hand (palm) and forearm;
- muscle fibers responsible for extension of the knee joint (quadriceps), as well as for unfolding the hip;
- muscle fibers located on the sole;
- back of the lower leg (long flexor, gastrocnemius and tibial muscle fibers).
Rubbing these muscles can only be used in the later stages of therapy. The remaining areas are stimulated by deep stroking, light kneading and more intense rubbing. No sudden or strong movements should be made (tapping, slapping, etc.).