Cavernous vascular malformation of the central nervous system is an empty tumor or a tumor filled with blood clots and thrombi. This pathology is a type of benign vascular neoplasms:
- different sizes;
- predominantly round in shape with clear boundaries;
- bluish color;
- with tubercles on the surface.
Cavernoma is localized in any part of the spinal cord or brain. The tumor does not metastasize and does not degenerate into cancer. Vascular malforation is quite rare and is usually diagnosed accidentally.
Main causes of the disease
The exact reasons for the development of pathology have not been established. Medical experts are inclined to believe that cavernoma is a congenital disease caused by a viral infection in the womb during the formation of the embryo’s circulatory system. Factors that can also provoke vascular malforation in a child include:
- late pregnancy;
- chronic diseases in the mother's body;
- injuries during childbirth;
- mother's bad habits.
It is possible that a cavernoma may form at another period of life. The causes of the tumor may be:
- traumatic brain injuries;
- radiation therapy;
- infections;
- weak immunity;
- brain inflammation;
- heredity.
In some cases, cerebellar cavernoma occurs due to angiomas, hemangiomas, and other tumors of the brain or spinal cord.
Varieties of the disease
Types of pathology are distinguished depending on where the benign formation is located in the frontal (right frontal) or parietal region, left temporal part, cerebellum, as well as thrombotic angioma.
According to histology, there are three types of cavernomas:
1. Classic
- the most common. The formation, in the form of a capsule with caverns, without vessels, fibers and without layers of brain tissue, clearly borders the brain.
2. Mixed
– in addition to caverns, the tumor consists of various vessels with layers of brain tissue.
3. Proliferative
– with the presence of areas of endothelial proliferation.
In addition, cavernomas are divided into subacute and chronic, with and without symptoms indicating hemorrhage. The clinical picture depends on the type of disease. Treatment for different types of cavernoma may also vary. The modern diagnostic complex in our clinic allows us to make the most accurate diagnosis and prescribe the correct treatment for such dangerous ailments as cavernoma, cervical osteochondrosis, intervertebral hernia, etc.
Brain angioma treatment in Germany: radiosurgery
Radiation as a treatment method is used if the tumor is located in hard-to-reach areas or when removing it there is a risk of affecting important areas of the brain. As a rule, the radiosurgical method is used for formations up to 1 centimeter.
A gamma knife is used for radiosurgical treatment. The required effect of treatment may occur in 4-5 months or several years.
The doctor must determine which treatment method is optimal. A qualified neurosurgeon will select a technique based on the situation and health status.
What danger does pathology pose?
The consequences of a cavernoma depend on its location. In addition to headaches, convulsions, nausea and vomiting, the tumor may be accompanied by mental disorders (inability to normally perceive the environment, loss of practical skills, lack of self-criticism). Due to the disease, loss of speech function and the presence of auditory hallucinations are possible. In many cases, there is an inability to swallow normally, epileptic seizures, and vascular ruptures. Particularly dangerous are hemorrhages, oxygen deprivation of the brain and paralysis.
The most terrible consequences of a cavernoma, which is localized in the dominant temporal lobe. If the respiratory or vasomotor system is damaged, death occurs.
Clinical picture
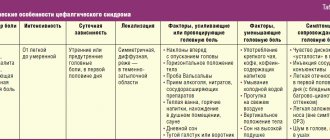
Cavernomas are often asymptomatic.
Symptoms begin to appear with hemorrhages, as well as with growth into the surrounding tissues or their compression.
Focal neurological symptoms are associated with the amount of hemorrhage, epileptic seizures or increased intracranial pressure.
The most common headaches are of various types.
When the cavernoma is located supratentorially, epileptic seizures occur in more than 55%.
After the hematomas resolve, the symptoms decrease significantly.
Complex of signs of pathology
Mostly the disease occurs without pronounced symptoms. Congenital cerebellar cavernoma often manifests itself when the patient reaches the age of twenty to forty years. Clinical picture of the disease:
- epilepsy attacks;
- increasing headaches;
- uncertainty, unsteadiness of gait;
- loss of movement coordination;
- weakening of visual and auditory functions;
- noise in ears;
- nausea, vomiting;
- absent-mindedness, memory lapses;
- decreased intelligence;
- paresis and paralysis;
- loss of sensation;
- hoarseness of voice.
Cavernoma can cause numbness of the limbs, twitching and paralysis of the tongue. Often the headache that accompanies the disease indicates a rupture of the walls of the tumor.
Research methods
First, a survey of the patient’s complaints and an objective medical examination are carried out. The patient is prescribed blood and cerebrospinal fluid tests. If a cavernoma is suspected, the patient is referred to a set of instrumental diagnostic measures:
1. Magnetic resonance imaging.
2. Angiography.
3. Tractography.
4. Computed tomography.
5. Ultrasound scanning.
6. Electroencephalography.
The most accurate method is MRI. Diagnosis and treatment of various tumors of the brain and spinal cord, as well as medical support for spinal lesions such as hernia, are carried out in the neurosurgical department of Zavalishina E.E.
Methods for identifying and treating cerebral angiomas
Among the most informative methods for detecting a vascular tumor is an angiographic study with contrast, which allows one to analyze the course of blood vessels, the direction of blood flow, and the volume of the tumor. Before the examination, the specialist clarifies in detail the patient’s complaints, the presence of other developmental defects, and family history. In addition to X-ray contrast angiography, MR angiography with contrast and computed tomography are performed.
example of angioma on a diagnostic image
The treatment tactics for a patient with cerebral angioma depend on its location, diameter, and blood flow characteristics. Almost always, angiosurgeons recommend surgical removal of the formation, and vascular intracranial neoplasia is considered an absolute indication for intervention. Before excision of the angioma, conservative supportive therapy is prescribed:
- Sedatives, tranquilizers;
- Analgesics;
- Vascular drugs and nootropics.
Small asymptomatic angiomas in some cases are simply observed - with severe concomitant pathology, high risk of surgery, deep localization of the tumor, when it is not possible to remove it due to lack of equipment and other objective reasons.
Modern surgery offers several types of operations on vascular intracranial formations, the main principles of which are not only the elimination of altered vessels and restoration of blood flow, but also minimal tissue trauma with a reduced risk of complications. From open trepanations they move on to minimally invasive endovascular interventions, as well as strictly targeted action of ionizing radiation (radiosurgery).
Classic tumor removal involves opening the skull and dura mater (trepanation), ligating the supply vessels and the actual elimination of the vascular weave with restoration of blood flow. The operation is traumatic, risky and is only possible if the angioma is located at a superficial location accessible to the surgeon.
surgical removal of angioma
Sclerosis of blood vessels means the introduction of sclerosant drugs into their lumens, causing gluing of the vascular walls and scarring, while the formation is turned off from the blood circulation and decreases in volume.
One of the options for minimally invasive treatment is embolization of angioma, when metal or plastic spirals are placed inside the vessels or a liquid drug is injected, causing blockage of the vascular lumens and stopping the movement of blood in them. Some patients undergo surgery more than once.
embolization of angioma
After removal or embolization of the angioma, cerebral angioplasty may be performed to restore adequate levels of blood flow. The vessels are dilated with stents or balloons.
Radiosurgery gives good treatment results not only for malignant tumors, but also for many benign processes. In neurosurgery, the technique is especially relevant, since it does not require incisions and penetration directly into the brain. Exposure to ionizing radiation, strictly focused on the tumor focus, causes its destruction and sclerosis with gradual regression.
Gamma knife and cyber knife are installations for radiosurgical treatment that allow you to direct a beam of radiation of a given power to the exact area of the brain that is occupied by the angioma. For the patient, the procedure is painless; usually one session of radiation is required, but for large formations there may be more.
Radiosurgery is considered one of the most modern methods of treatment, but the possibilities of its use are often limited by the high cost of procedures and the lack of necessary expensive equipment and specialists. Such treatment can only be completed in large oncology clinics, and some patients even go abroad for treatment.
The prognosis for any intracranial vascular formation is always serious, since the tumor grows and its constituent vessels can rupture. With timely diagnosis and proper treatment, it is favorable, the patient quickly recovers and returns to normal life. In the event of a rupture, the prognosis may become unfavorable due to the risk of not only serious neurological abnormalities, but also the death of the patient from cerebral edema.
Methods of treating the disease
Timely treatment of cavernoma guarantees a positive prognosis. The tumor itself is non-cancerous and not life-threatening. A plan for getting rid of the pathology is developed depending on the location of the formation, the patient’s age, symptoms and the presence of other concomitant diseases. The following treatment methods are used:
- regular monitoring of the course of the disease;
- conservative therapy;
- radiosurgical method;
- surgery to remove cavernoma.
Conservative therapy is effective if the disease is detected before complications occur. Timely treatment with medications guarantees a quick restoration of the patient’s health and a return to a normal, full-fledged lifestyle. In almost 100% of cases, surgical intervention allows you to get rid of the disease forever and with a minimal percentage of postoperative risks. Surgery to remove a cavernoma is guaranteed to relieve epileptic seizures, but there is a risk of repeated hemorrhages. Conservative treatment also maintains the risk of hemorrhages, but does not eliminate epilepsy attacks, which forces the patient to take anticolvulsants throughout his life.
There are contraindications to the operation. The size, shape of the tumor, age and general health of the patient must be taken into account. If the cavernoma is located in a hard-to-reach area, radiosurgery is used to extract it. Complications are also possible after radiosurgery, but, in comparison with radiation therapy, ionizing radiation does not have a negative effect on nearby healthy areas. In addition to the listed methods, laser therapy, diathermocoagulation, sclerotherapy, hormonal therapy and cryotherapy are used to treat vascular malforation and remove cavernomas.
Stereotactic radiosurgery of cavernous angiomas of the brain stem
GAMMA KNIFE AND CAVERNOSAL ANGIOMAS OF THE BRAIN
Cavernous angiomas of the brain (cavernomas) are most often congenital vascular anomalies, represented by single, much less often multiple cavities, separated inside by septa (septa) and filled with blood. Despite the supposed congenital nature, they are more often detected in adults than in children, but in children they are more severe. The blood supply to the cavity is carried out from small arterioles and capillaries, and the outflow of blood through venules is of the same order. Due to the small caliber of the feeding vessels, the blood pressure in cavernomas is low, so the draining veins do not hypertrophy and are not visible during SCT/MRI/angiography.
Schematic representation of the structure of cavernous angioma
A special feature of cavernomas is a defective vascular wall, so thin that the cellular elements of the blood - red blood cells - “sweat” through it and settle in the adjacent medulla. This process is called “diapedetic hemorrhage.” The products of the natural breakdown of hemoglobin (hemosiderin), contained in red blood cells, form a zone of chronic, specific and very recognizable changes on MRI around the cavernoma. Cavernomas can be localized in any part of the brain: in the cerebral hemispheres, in the brain stem, cerebellum, subcortical ganglia, in the corpus callosum and in the lateral ventricles. In approximately 30-40% of cases, cavernous angiomas are combined with another type of vascular malformation - venous angiomas. Venous angiomas are an anomaly in the development of venous vessels in the form of a “bundle” of small veins (“Gorgon’s head”) gathering into one large drainage vein.
The incidence of cavernous angiomas is several cases per million population.
WHAT IS THE THREATEN OF THE PRESENCE OF CAVERNOUS ANGIOMA?
Cavernomas can remain asymptomatic throughout life. However, in a number of patients, clinical manifestations can be of two types, both individually and in combination:
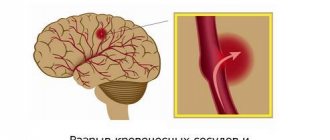
Hemorrhage. Sometimes, an increase in blood pressure inside a cavernoma leads to local destruction of the vascular wall and the formation of intracerebral hemorrhage. Unlike AVMs, hemorrhages from cavernomas are never massive and do not pose a threat to the patient’s life, with the exception of extremely rare cases of cavity localization in the lower parts of the medulla oblongata, where the centers of cardiovascular and respiratory regulation are located. However, when the focus of hemorrhage is located in any functional area, even a small volume of hemorrhage can lead to the appearance of neurological symptoms (for example, the development of weakness in the opposite half of the body, when located in the motor cortex or in the deep structures of the cerebral hemispheres).
Epileptic syndrome. In some cases, due to the chronic presence of hemosiderin in the medulla or with the development of acute hemorrhage, a focus of pathological brain bioactivity may form, clinically manifested by epileptic seizures of various structures (convulsive, non-convulsive, absence seizures, vegetative, polymorphic and others). Thus, cavernomas extremely rarely pose a threat to the patient’s life, but can have a significant impact on the quality of life.
HOW TO DIAGNOSE A CAVERNOMA?
- Magnetic resonance imaging (MRI) is the most informative method for diagnosing cavernomas. In T1 and T2 scanning modes, a cavity surrounded by a black rim of hemosiderin may be visible, with signs of acute and subacute hemorrhages. The most sensitive mode is T2* (“T2 with star”), which allows you to diagnose even small (1-2 mm) cavernomas that are not visible in other scanning modes.
- Computed tomography - its diagnostic value is limited, as a rule, to the acute period of hemorrhage (several days), when a fresh focus of shed blood is visible on the image.
- Angiography is not informative in diagnosing cavernomas
HOW TO GET RID OF A CAVERNOMA?
In the case of asymptomatic cases of incidentally detected cavernous angiomas, the generally accepted tactic is dynamic observation. In case of episyndrome formation and/or hemorrhage, two treatment methods are possible:
- Surgical removal of cavernoma is a highly effective method that allows you to once and for all relieve the patient from the risk of repeated hemorrhages. Surgery is also effective if the patient has epileptic seizures, but its effectiveness is reduced in the case of a long history of epileptic syndrome.
- Radiosurgery is performed on the same principle as for arteriovenous malformations - with the goal of causing complete obstruction of blood flow. However, radiation doses in this case may be significantly less than with AVM. Morphological changes in this case are similar to those in arteriovenous malformations - the walls of the cavernoma and the mouths of the feeding vessels undergo hyalinosis, as a result of which the blood flow decreases, pinpoint hemorrhages stop, and the risk of repeated spontaneous intracerebral hemorrhages is reduced by 50-70%. Episodic attacks also become less frequent or disappear completely, but, as in the situation with surgery, the longer the history of the disease, the less likely it is to completely recover from them.
- A meta-analysis of the literature on the effectiveness of the use of Gamma Knife (World Neurosurg. 2021 Mar; 123: 371-377), conducted by researchers from the University Hospital of Sichuan (PRC), proves that the annual risk of hemorrhage is reduced many times and significantly within the first 2 years after radiosurgical treatment, continuing to decrease in subsequent years. Thus, today, radiosurgery is the method of choice in the treatment of patients with cavernous angiomas.
DO YOU NEED TO IRRADIATE MULTIPLE CAVERNOMAS? As in the case of single cavernomas, radiosurgical treatment is carried out only on the lesion that manifests itself clinically - hemorrhage or epileptic seizures.
WHAT TO DO WITH VENOUS ANGIOMA? The question often arises: how to get rid of venous angioma? Firstly, you should know that venous angiomas never manifest themselves as hemorrhages or epileptic seizures. Secondly, although they represent a venous network that is abnormal in structure, they nevertheless take full part in the local venous circulation of the brain.
The only option for the appearance of clinical symptoms associated with venous angioma is the spontaneous development of thrombosis of the draining vein. This situation is more hypothetical than real. In this case, the patient will experience cerebral venous infarction with severe swelling at the site of impaired venous outflow. And only one way can help cope with such a situation - thrombolytic and anticoagulant therapy. Attempts to surgically or radiosurgically influence venous angiomas not only do not make any sense, but will also lead to gross local disturbances of venous blood flow in a manner similar to spontaneous thrombosis. Thus, diagnosing a patient with venous angioma is not a reason for any treatment.
WHAT IS THE BEST TREATMENT METHOD FOR CAVERNOMAS?
Brainstem hemorrhages caused by cavernous angiomas can cause severe neurological deficits due to destruction of neural tissue, ascending and descending brain pathways, and cranial nerve nuclei.
The natural course of brainstem cavernomas differs from similar manifestations in other localizations, because has a higher risk of hemorrhage and permanent neurological deficit. After the first hemorrhage, cavernomas become unstable and the risk of repeated hemorrhages increases.
From the point of view of preventing recurrent hemorrhages, the effectiveness of surgical treatment is higher. However, when cavernomas are localized in functionally important or hard-to-reach areas of the brain (for example, in the subcortical nuclei, brain stem), surgery itself has a high risk of residual neurological deficit, and radiosurgery can largely avoid or reduce the risk of these complications.
Brain stem cavernoma BEFORE Gamma Knife radiosurgery (left) and 2 years AFTER Gamma Knife (right)
Microsurgical resection is the first choice only for accessible brainstem cavernomas located beneath the arachnoid or ependymal surface, and even then carries a significant risk of complications.
Regarding radiosurgery, the results of a meta-analysis of 5 studies (4 using Gamma Knife and 1 using a linear accelerator) including 178 patients with truncal cavernomas revealed a significant reduction in the rate of recurrent hemorrhages after stereotactic irradiation. Thus, radiosurgery should be considered as the treatment of choice for the treatment of brainstem cavernous angiomas in cases with high surgical risk (J Neurosurg. 2014 Apr;120(4):982-7.)
The decision on the optimal method of influence is made individually, taking into account all possible factors, incl. and taking into account the informed choice of the patient himself.
Preventive measures
The most common type is congenital cavernoma. Modern medicine is not able to eliminate genetic abnormalities. To avoid problems with the central nervous system, it is recommended to take care of blood vessels:
- monitor blood pressure;
- eat properly and balanced;
- get rid of excess weight and bad habits;
- control cholesterol and blood sugar levels;
- avoid lifting heavy objects;
- dilute a sedentary lifestyle with physical activity and going to the gym;
- avoid stress.
If you experience any problems with your health, in particular periodic headaches and dizziness, disturbances in visual and auditory functions, you should immediately seek medical advice.
You can make an appointment at our clinic using the phone number listed on the website.
Brain angioma treatment in Germany: surgery
If the angioma does not manifest itself in any way, it is permissible to simply observe it without using any treatment. However, quite often there is a need to remove it. The operation is prescribed for epileptic seizures, as well as in cases where bleeding has been detected and there is a risk of repeated hemorrhage. Statistics show that on average the risk of hemorrhage with cerebral angiomas is 1-15%, but if one hemorrhage has already occurred, then it can occur again in 35% of cases.
This is a rather complex operation that requires high skill of surgeons and the use of special equipment.
If a brain angioma is diagnosed, surgical treatment in Germany is carried out in the best medical centers by leading German neurosurgeons. This allows us to demonstrate high efficiency and minimal possibility of complications. Today, in standard world practice, microsurgical resection is used to remove brain angiomas, which produces complications in an average of 15% of cases. But in specialized clinics in Germany this percentage is much lower, since the problem is dealt with by top-class specialists.