Causes of pain in the shoulder joints
There are many reasons for the appearance of painful sensations. Pain in one or both shoulders can be a consequence of inflammation of the tendons, microtrauma of the articular cartilage, inflammatory-degenerative pathologies of the joints and cervicothoracic spine. The discomfort can be either minor or so intense that you cannot move your arm.
Among the causes that cause sharp or aching pain in the shoulder are:
- one-sided intense load for a long time;
- scoliosis, lordosis and other deviations in the normal position of the spine;
- physical inactivity.
In addition, pain can occur due to infections, inflammatory processes, hereditary predisposition, diseases of internal organs, and tumors.
In cases where the right shoulder hurts, the following pathologies may be present:
- Tendonitis is inflammation of tendons and soft tissues due to significant physical activity.
- Myositis - when the muscles of the shoulder joint are involved in the inflammatory process.
- Arthrosis is the destruction of articular cartilage.
- Arthritis is an inflammatory process in a joint due to infection, allergic reaction or autoimmune diseases.
- Osteochondrosis of the cervical spine.
- Bursitis is an inflammation of the joint capsule.
- Capsulitis is a pathological change affecting the joint capsule and synovium.
- Brachial nerve neuritis.
- Tuberculous lesion of the joint on the right.
- Humeroscapular periarthritis.
- Metastasis from a nearby tumor.
- Chondrosarcoma.
- Right-sided pneumonia.
Pain in the left shoulder joint is much less common, especially if the person is right-handed. Still, the load on the left hand is significantly less compared to the right. When your left shoulder hurts, the reasons may be the following:
- sprain;
- biceps tendinitis;
- intervertebral hernia in the cervical spine;
- calcification in the tendon;
- angina pectoris or myocardial infarction.
There are cases when the shoulder hurts when raising your arm. Here we can talk about pathologies such as:
- joint injuries;
- rheumatic lesion;
- rotator cuff tendinitis;
- tenosynovitis;
- tendobursitis and bursitis;
- myositis;
- hernia of the cervical spine.
The appearance of pain in the shoulder when trying to move the arm back indicates the presence of bursitis, radiculitis, tendinitis, spinal overload, arthrosis-arthritic joint damage, myocardial infarction.
Humeroscapular periarthritis: what is it?
Humeral periarthritis is a lesion of soft tissues located in the immediate vicinity of the shoulder joint, i.e. tendons, ligaments, muscles of the joint capsule, etc. The disease is usually preceded by degenerative changes in the muscle tendons, which occur against the background of a decrease in the quality of their blood supply, with subsequent development and spread inflammatory process. After all, ligaments and tendons are located in close proximity to each other, which is why they are usually affected simultaneously. This is accompanied by pain of varying intensity and limited mobility, which can be complicated by nerve damage.
Periarthrosis today occurs in 4-7% of people, and women are more often affected, and with age-related changes, the risk of its development increases.
Thus, periarthrosis is a collective term that can mean a lot of different disorders. Therefore, to clarify the diagnosis and the cause of pain in the shoulder area, it is customary to clarify the type of damage to the periarticular soft tissues. As a result, the following can be diagnosed:
- rotator cuff tendonitis - inflammation of the tendons of the supraspinatus, infraspinatus, teres minor and subscapularis muscles, which are responsible for rotating movements of the shoulder;
- biceps tendonitis - an inflammatory process affecting the biceps tendon;
- calcific tendonitis - inflammation of the tendons of the shoulder muscles, accompanied by the formation of calcium salts in them;
- partial or complete rupture of the tendons of the shoulder muscles;
- retractile capsulitis – degenerative-dystrophic changes in the capsule of the shoulder joint;
- impingement syndrome - infringement of the tendons of the biceps brachii and rotator cuff muscles by the head of the humerus and the end of the scapula.
Often, glenohumeral periarthritis is called not only periarthrosis, but also frozen shoulder syndrome, painful shoulder, cervicobrachial syndrome and shoulder arthropathy.
The development of tendinitis and lack of treatment can cause the joint capsule to become involved in the inflammatory process, which leads to its swelling and accumulation of fluid inside. This is called bursitis, which can turn purulent if bacteria penetrate the inflammatory exudate. If treatment is not started at this stage, the tendon and the wall of the bursa may fuse into a single whole, which will lead to a decrease in the range of motion.
In addition, with glenohumeral periarthritis, the aponeurosis of the shoulder, i.e., a wide tendon strip covering the muscles, can also be affected. As a result, in individual areas or over the entire area, foci of replacement of normal connective tissue can form, which causes significant restrictions on mobility.
The most common complication of the disease is rupture of the affected tendons and ligaments of the shoulder. In some cases they are accompanied by shoulder dislocation.
And the most dangerous consequence of glenohumeral periarthritis is adhesive capsulitis, which after 3-4 months can lead to complete immobility of the shoulder. It is characterized by active growth of connective tissue in the joint capsule and the formation of gross scar changes. As a result, the synovial membrane of the shoulder joint is also deformed, thickening and sticking together in places. Fibrous changes in adhesive capsulitis affect both the muscles and ligaments of the shoulder, which leads to a gradual decrease in the range of motion in it and the development of frozen shoulder syndrome. The disease is dangerous because even with adequate therapy, the full range of motion in the joint may not be restored.
Symptoms of the disease
Shoulder pain manifests itself in different ways depending on the cause. Acute is typical in case of injury. When a bruise, dislocation or sprain occurs, the patient experiences discomfort that increases when moving the upper limb. When a fracture occurs, it becomes impossible to move the arm.
Unbearable pain radiating to the neck and upper back is observed with capsulitis. In addition to pain, there is an inability to move the arm back or raise it. Severe pain also occurs with brachial neuritis and arthritis. The first is characterized by the absence of signs of inflammation in the joint; in the second case, swelling of the soft tissues and limited range of motion are noticeable.
Aching pain in the shoulder may be a sign of osteochondrosis of the cervicothoracic spine. Often the symptom is accompanied by numbness of the hand, burning and tingling sensation in the fingers. Aching pain is also observed with deforming arthrosis, but in this case, along with discomfort, a person notes stiffness of movement and swelling in the shoulder joint in the morning, crunching and clicking when bending/extending the arm. With the gradual destruction of cartilage, lifting heavy objects or active movement provokes increased pain.
Constant pain for several weeks is characteristic of bursitis, when the inflammatory process develops in the periarticular bursa. The disease is accompanied by the formation of a compaction, upon pressing on which a fluid transfusion is felt.
Plexitis - symptoms and treatment
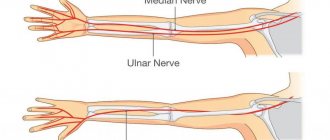
Damage to the roots and nerve plexus leads to pain. Due to gross disturbances of the nerve fibers, loss of sensitivity occurs and restriction of movements of the affected part of the body.
The localization of pain and the manifestation of other symptoms depend on which roots and individual loops of the plexus are affected and in what quantity.
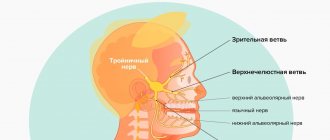
With lesions of the upper cervical roots (C1-C4), pain is observed in the area of distribution of the occipital, auricular, and phrenic nerves. Pain in the scapular region, shoulder girdle and upper limb indicates damage to the lower cervical and upper thoracic roots. Pain in the area of the sacrum, lower back, thigh, buttocks radiating to the groin area indicates damage to the lumbar and sacral roots.
Quite often, with lesions of the cervical and thoracic roots, pain is localized in the neck, in the area of the scapula and spreads throughout the arm or along the cutaneous nerve.[8][10]
Pain can be spontaneous or occur with movement. They are dull in nature, but more often they are sharp, burning and shooting. In most cases they are worse at night. The pain may spread to other parts of the body.
Movement of the arm (raising, abducting, flexing/extending the wrist) increases pain in cervicobrachial plexitis. Tilt of the head back, to the sides, as well as to the affected side (radicular localization), or to the opposite (localization in the plexus) can also be painful.
The presence of pain creates a forced position of the body.[9] The head is tilted slightly down or in the direction opposite to the pain, the hand often takes a pronator and flexion position of the forearm.
Pain points are found in the paravertebral region, above and below the clavicle, with pressure on the radial nerve in the place where it bends around the humerus, pressure on the plexus in the axillary fossa, points in the elbow bend, along the midline of the inner surface of the forearm, on the palmar surface, as well as in the gluteal and groin area, on the surface of the thigh and the outer surface of the lower leg.
With radicular localization of plexitis, Neri's symptom occurs. It manifests itself in the fact that movements of the cervical spine cause pain in the lumbar region, and there is also a return to the shoulder blade and arm.
The pain is sometimes accompanied by paresthesia in the form of numbness. An objective sensitivity disorder is usually absent; less often it is expressed by hyperesthesia (increased sensitivity) or mild hypoesthesia (loss of sensitivity).
Changes in reflexes usually do not occur. The intrinsic excitability of muscles is often increased. Fascicular twitching (contraction) of the muscles is also observed when they are stretched or tapped.
With a long course of the disease, diffuse weight loss of the muscles of the arm and shoulder girdle with flabbiness of the muscles may develop. In this case, tendon and deep reflexes may be reduced.
When cervical disc herniations occur, the C6 or C7 roots are affected. The pain in such cases spreads not only along the arm, but radiates to the neck, back of the head, sometimes to the frontal region and to the corresponding side of the chest. The pain intensifies when the head is tilted to the painful side; the load on the tilted head causes pain in the fingers. In addition to headaches localized in the back of the head and radiating to the temple and face, dizziness in the form of lightheadedness, feelings of uncertainty or true vestibular dizziness, auditory disorders (noise and pain in the ears), visual disorders (a feeling of heaviness and pressure on the eyeball, fatigue of accommodation) are noted - ability to see clearly). Posterior disc displacement may cause symptoms of spinal compression with the development of partial or complete spinal block.[9]
With plexitis, pathologies of blood distribution can sometimes occur. This manifests itself in redness or cyanosis, as well as swelling of the limb and a decrease in its temperature. In some cases, a sweating disorder is observed. Herpes zoster occurs less frequently.[7]
Diagnosis of pathology
Naturally, when there is discomfort, the question inevitably arises: what to do if your shoulder hurts? Don't wait for the symptoms to go away on their own. It is imperative to consult a doctor, whose specialization will depend on the cause of the disease and the general condition of the patient.
If the pain appears after a fall or bruise, then contact a traumatologist. Osteochondrosis and neuritis are treated by a neurologist, a surgeon and a rheumatologist eliminate the consequences of arthrosis, arthritis and tendonitis.
When painful sensations are accompanied by a general deterioration in well-being, it is recommended to consult a therapist, oncologist, cardiologist or gastroenterologist. Indeed, sometimes pain is reflected when there is a discrepancy between the localization of discomfort and the location of damaged organs or tissues. It is very important to diagnose in time, because shoulder pain can appear due to myocardial infarction, pneumonia, pleurisy, pancreatitis, cholecystitis, and neoplasms in the chest.
For diagnostic purposes, the doctor may prescribe the following types of examinations:
- X-ray of the shoulder or entire upper limb;
- Ultrasound of the shoulder joint;
- MRI of the joint and/or spine;
- ECG.
In addition, you may need to take a general blood test, as well as biochemistry and sexually transmitted infections. The patient is also prescribed fluorography and fibrogastroduodenoscopy.
Complications
Over time, most brachial plexus injuries in adults and children heal without permanent damage. However, some injuries can cause temporary or permanent impairment:
Joint stiffness. When an arm or hand is paralyzed, joint stiffness may occur, limiting joint movement even though control of the limb has been restored. To achieve this, doctors usually prescribe physical therapy classes during the recovery period. Pain. The pain occurs due to nerve damage and can become chronic. Loss of sensation. If you lose sensation in your arm or hand, there is a risk of accidentally injuring or burning it and not noticing it. Muscular atrophy. Nerves recover slowly, taking several years. During this time, muscles that are not subjected to sufficient stress can atrophy. Irreversible damage. The extent of recovery from a brachial plexus injury depends on a number of factors, including age, type, location, and severity of the injury. Even after surgery, some patients experience irreversible damage, ranging from weakness in the hand, shoulder or forearm to paralysis.
Treatment for pain in the shoulder joint
When complaining of pain in the shoulder, the specialist prescribes comprehensive treatment. Therapy includes:
- Local and general anesthesia. Can be achieved using medications or physiotherapeutic methods, acupuncture, etc.
- Eliminating the root cause of pain. Manual therapy, osteopathy, PRP therapy and Kinesitherapy help with this.
- Symptomatic therapy. They use products to relieve swelling of soft tissues, hyperemia of the skin, and reduce temperature.
- Rehabilitation treatment. This includes kinesitherapy.
During the rehabilitation period, physical therapy and physiotherapeutic treatment are widely used to restore joint mobility. In advanced cases and in the absence of effect from conservative therapy, surgical treatment is possible.
The article was reviewed by traumatologist-orthopedist V.Yu. Bogdanov.
Cost of treating shoulder pain in our Center
| Services list | Price |
| Initial consultation with a kinesiotherapist | 1600 |
| Interim consultation with a kinesiotherapist | for free |
| Session with a kinesiotherapist (1 patient) | 3900 |
| Individual lessons with a personal trainer | 2700 |
| Subscription for 1 month of training in the gym on simulators | 10 000 |
| Subscription for 6 months of gym training | 45 000 |
| Physiotherapist consultations | 1600 |
| Physiotherapist consultations during the cycle | for free |
| UVT 1 procedure | 2000 |
| HIVAMAT up to 15 min./1 body unit | 2200 |
| HIVAMAT up to 15 min./2 body units | 3200 |
| Appointment with an orthopedist-traumatologist | 1600 |
| Intra-Articular PRP Injection | 6500 |
| Massage of one upper limb (15 min.) | 2200 |
| Massage of two upper limbs (30 min.) | 3000 |
| Kinesio taping | 1100 |
| Complex taping (joints) 1 zone | 1600 |
| Complex taping (joints) 2 zones | 2200 |
Contact us
Call now
8 (495) 803-27-45
Make an appointment through our service
Make an appointment
Treatment process at the Innovation Center
Our Innovative Clinic has created excellent conditions for the diagnosis and treatment of pain in the shoulder joints of various types and origins. After finding out the causes of the pathology, the doctor will select tactics and methods of treatment. We practice using the following techniques:
- Acupuncture.
- Manual therapy.
- Kinesitherapy.
- Osteopathy.
- Massotherapy.
- Physiotherapy.
We achieve excellent results using shock wave therapy and Hiwamat therapy. The course of treatment is carried out under the supervision of a doctor, whose efforts are aimed not only at relieving unpleasant symptoms, but also at eliminating the cause of discomfort. The professionalism of our specialists and an individual approach will help you completely get rid of the problem, and if this is not possible, then avoid complications and achieve stable remission. This is confirmed by a large number of reviews about the work of our center and doctors both on our website in the Reviews section and on other sites on the Internet.
Causes
Periarthrosis is the result of the development of an inflammatory process or degenerative-dystrophic changes in the shoulder joint, which often accompany each other. Therefore, most often it occurs against the background of other pathologies of the musculoskeletal system, which explains the higher incidence of development in older people.
In general, the disease can result from:
- receiving microtrauma to muscles and tendons, which is facilitated by excessive loads on the shoulder, regular performance of repetitive movements (raising/lowering, adduction/abduction of the arm), which is due to the characteristics of work or sports;
- injuries to the soft tissues of the shoulder, leading to the formation of a hematoma, swelling in the area where the blow was received;
- prolonged hypothermia, leading to spasm, i.e. narrowing of the lumen, blood vessels of the skin and reflex spasm of the vessels of the periarticular tissues;
- maintaining a sedentary lifestyle and prolonged stay in a static position, which causes impaired blood circulation, including in the area of the shoulder joint;
- neuroreflex spasms of muscles and small blood vessels, leading to malnutrition of soft tissues (ischemia), which can be observed with myocardial infarction, angina pectoris, as well as osteochondrosis of the cervical spine;
- disturbances in the nutrition of the soft tissues of the shoulder as a result of the inclusion of neurotrophic mechanisms, which is observed in diabetes mellitus, tuberculosis, obesity, Parkinson's disease and leads to the development of ischemia with subsequent death of areas of soft tissue and their replacement with coarse connective tissue;
- congenital anomalies of the shoulder joint, including dysplasia and arthropathy, as well as developmental disorders.