Drooping eyelid or ptosis is a condition that can be congenital or acquired. The main danger is that drooping eyelids can be not only an unpleasant cosmetic defect, but also be a symptom of a serious illness.
Normally, the edge of the upper eyelid overlaps the eyeball and iris by about 1/3. But this is not so important for determining the presence of ptosis, since drooping of the eyelid, as a rule, is immediately noticeable to both the patient and others, in comparison with a healthy eye.
A condition such as drooping of the upper eyelid can limit visibility due to a narrowing of the palpebral fissure, thus leading to excessive stress on the organs of vision, “overstraining” them. For this reason, prolapse is considered to be an ophthalmological pathology, which can cause visual impairment. However, a visit to a neurologist would not be a bad idea; more on that below.
Causes of drooping eyelids
The upper eyelid is more than just a flap of skin. The eyelid consists of a muscle that attaches to the cartilage in the eye socket. The muscle (it is called the muscle that lifts the upper eyelid) is located in the thickness of the subcutaneous fat.
The main causes of the pathology:
- a congenital disease that is associated with insufficient development of the muscle designed to lift the upper eyelid;
- injury to the muscle that lifts the upper eyelid;
- damage to the oculomotor nerve;
- stretching of the tendon of the muscle that lifts the upper eyelid (this condition is typical for old age);
- damage to the cervical sympathetic plexus (the so-called Horner's syndrome, expressed in ptosis, constriction of the pupil and “retraction” of the eyeball);
- diabetes mellitus as a cause of metabolic damage to muscles and nerves;
- acute cerebrovascular accident (in this case, drooping eyelid is accompanied by a number of other symptoms);
- tumor of the brain, spinal cord, or neck area;
- disturbance of neuromuscular transmission (myasthenia gravis or myasthenic syndrome);
- damage to the oculomotor nerve as part of polyneuropathy (in combination with damage to a number of other peripheral nerves);
- complication of botulinum toxin administration for cosmetic or medicinal purposes;
- botulism.
Considering the many factors that lead to drooping eyelids, consultation with a doctor is mandatory.
At CELT you can get advice from a neurologist.
- Initial consultation – 4,000
- Repeated consultation – 2,500
Make an appointment
Horner's syndrome - Treatment in Israel
As an independent disease, Horner's syndrome is not dangerous. However, its appearance indicates the presence of a pathological process in the body. Therefore, the basis of treatment for Horner's syndrome is the identification and treatment of the underlying disease.
However, there are some methods of treating this disease, which also has a negative cosmetic effect:
- Neurostimulation is the effect of current pulses on the affected muscles and nerves. Electrodes are applied to the skin, sending impulses to nerves, muscle fibers, and blood vessels. This leads to active muscle contractions, improved blood supply and innervation.
- Plastic surgery deals with the correction of pronounced cosmetic defects in Horner's syndrome. Experienced plastic surgeons will help restore the normal shape of the eyelids and palpebral fissure.
Horner's syndrome is a pathological condition that requires careful diagnosis and targeted treatment.
Attention! All form fields are required. Otherwise we will not receive your information. Alternatively use
Neurological diseases leading to ptosis
- Myasthenia gravis is a serious disease in which the transmission of impulses from nerve to muscle is disrupted. Myasthenia gravis is characterized by increased muscle fatigue. The disease affects all muscles, but the greatest manifestations can affect only the eye muscles, causing ptosis, double vision, and decreased focus. For the initial diagnosis of myasthenia gravis, a neurologist conducts a test with the introduction of proserin and examines the nerves and muscles using ENMG (electroneuromyography).
- Myopathy, in which double vision and drooping of both eyelids are also observed, while the performance of the muscle that lifts the eyelid is weakened, but present. Myopathies are of different types according to their origin. The examination uses needle EMG and a number of laboratory tests.
- Palpebromandibular synkinesis is involuntary concomitant movements that accompany chewing, abduction and opening of the lower jaw. For example, when you open your mouth, the prolapse can suddenly disappear, but after closing the mouth, it can be restored. This condition can be either an independent disease or the result of improper restoration of the motor fibers of the facial nerve after its damage.
- Bernard-Horner syndrome (expressed by a combination of drooping of the upper eyelid, narrowing of the pupil and “recession” of the eyeball). It is a manifestation of the pathology of the cervical sympathetic plexus. Sometimes the pathology is detected against the background of increased sweating on the face and incomplete paralysis of the brachial nerves on the affected side.
Causes of the disease
Bernard-Horner syndrome is rare and in most cases is considered a secondary acquired disease. Moreover, the etiopathogenetic factor of the disease, that is, the exact cause, cannot always be established and described. But in the case of a certain primary disease, it is precisely this disease that is targeted for elimination and treatment by doctors.
Classification of forms of pathology involves two options:
- Idiopathic – primary type. An individual disease that arises as a result of its own causes does not depend on other pathologies. A set of symptoms can appear independently and suddenly against the background of a person’s completely good state of health. The most interesting thing is that the syndrome can disappear as unexpectedly as it appeared.
- Secondary type. It manifests itself as a result and against the background of a previously occurring disease that was diagnosed, established and treated. These diseases most often fall into the category of vascular, neurological, autoimmune, viral, and oncological.
Among the nosologies that are associated with oculosympathetic syndrome: prolonged headache, various injuries, aortic aneurysm, inflammatory processes in the middle ear, thyroid hyperplasia (goiter), multiple sclerosis, and a number of others.
The appearance of the syndrome can lead to damage to the central sympathetic pathway and the pathways leading from it to the eye. Among them, the cervical sympathetic ganglion and postganglionic fibers are of particular importance. These are efferent sympathetic fibers that go from the ganglia (nodes) to the tissues of the eye muscles.
Cerebral infarction, also known as stroke, is also among the causes of the symptom complex.
Disruption of the brain stem structures can cause Bernard-Horner syndrome, and since these structures contain the centers of thermoregulation of the human body, it is accompanied by loss or impairment of heat and pain sensitivity. Moreover, this phenomenon is observed on the opposite side of the body in relation to the pathways in the brain stem. The explanation for this is the bilateral symmetry of the human anatomical structure.
One of the ways a symptom complex arises is iatrogenic, arising as a result of medical influence on the patient. Iatrogenic options include surgical or obstetric trauma.
Drooping eyelid after botulinum toxin injection
According to statistics, after injections of botulinum toxin (Botox and other drugs containing it) into the eye area, drooping of the eyelid occurs in 20% of complicated cases, but this is almost always associated with errors during the procedure or is associated with the individual characteristics of the person.
Drooping of the eyelid after Botox injection is unpleasant, but, fortunately, it cannot be considered a serious pathology, since without additional therapy, signs of drooping completely disappear within 3-4 weeks after the injection of the drug.
Treatment of drooping eyelid
If the cause of drooping eyelid is a neurological disease, such as myasthenia gravis or neuropathy, then the underlying disease is treated first. Since ptosis is a symptom, it also goes away when the underlying disease is cured.
However, in some cases, complete recovery is impossible, and then surgical treatment is carried out for cosmetic purposes or, if ptosis leads to significant disruption of life due to deterioration of vision, then for therapeutic purposes.
Children undergo this operation no earlier than 3 years of age, but it should be done as soon as possible to prevent decreased vision and the development of strabismus.
In order to eliminate a cosmetic defect (when vision is not impaired), the operation is recommended to be performed after puberty, when the bony facial skeleton is finally formed.
If the prolapse is caused by injury, the operation can be performed directly during the initial treatment of the wound surface by the surgeon, or after healing, that is, after 6-12 months.
One way or another, the doctor makes a decision on the timing of the operation depending on the specific case.
Horner's syndrome - Types
Depending on the etiology, Horner's syndrome is:
- Primary (idiopathic) – develops without connection with any pathological processes as an independent disease.
- Secondary – develops in various diseases (for example, stroke).
In Horner's Syndrome, disturbances may occur at the level of any of the three neurons of the nerve impulse pathway:
- Lesions of the first neuron - can occur during transverse dissection of the spinal cord.
- Damage to the second neuron - develops when a tumor compresses the sympathetic nerve pathway.
- Damage to the third neuron occurs when motor fibers are damaged.
Preventing the development of drooping eyelids
An important point in the prevention of eyelid drooping is the timely treatment of any diseases that can provoke this pathology. For example, neuritis of the facial nerves must be immediately treated by a neurologist, and the possibility of drooping eyelids after Botox injections should be discussed with the specialist performing the manipulation.
If you notice weakness of the eyelids associated with age-related changes, then cosmetics and folk remedies can help you. Prevention methods include the use of tightening masks, oils and massage treatments.
Massage of the skin of the eyelids should be carried out with drooping eyelids. Before the procedure, the eyelids can be wiped with lotion to remove sebaceous scales and open the excretory ducts of the sebaceous glands. Massage using a cotton swab or disk soaked in an antiseptic solution or special ointment. Use stroking with light pressure, making circular and linear movements, moving from the inner corner of the eye to the outer corner. You can lightly tap your eyelids with your fingertips.
There are special gymnastics for weakness of the eye muscles.
Starting position – standing, sitting or lying down.
- We look up, without raising our heads, then sharply down. We repeat the movements 6-8 times.
- We look up and to the right, then diagonally down and to the left. We repeat the movements 6-8 times.
- We look up and to the left, then down and to the right. We repeat the movements 6-8 times.
- We look as far as possible to the left, then as far as possible to the right. We repeat the movements 6-8 times.
- We stretch our arm forward and keep it straight. We look at the tip of the index finger and gradually bring it closer, without stopping looking until the picture begins to “double.” We repeat the movements 6-8 times.
- Place your index finger on the bridge of your nose. We look at the finger alternately with the right and left eyes. Repeat 10-12 times.
- We move our eyes in a circle to the right and left. We repeat the movements 6-8 times.
- We blink quickly for 15 seconds. Repeat blinking up to 4 times.
- We close our eyes tightly for 5 seconds, then sharply open our eyes for 5 seconds. Repeat 10 times.
- Close your eyes and massage your eyelids with your finger in a circle for 1 minute.
- We shift our gaze from the nearest point to the far one and vice versa.
Movements of the eyeball during exercises should be as wide as possible, but not to the point of pain. The motor tempo can be made more difficult over time. The duration of such prophylaxis is at least 3 months.
It is worth noting that in case of myasthenia gravis and myopathy, such exercises are contraindicated, as they contribute to the worsening of drooping eyelids due to “exhaustion” of the muscle. Therefore, before engaging in any treatment, you must consult a specialist.
Horner syndrome
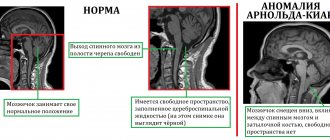
Horner's syndrome (JF Horner, Swiss ophthalmologist, 1831-1886) is a combination of symptoms caused by a violation of the sympathetic innervation of the eye.
In recent years, most manuals, in contrast to the classical canons, consider this symptom complex as a combination of ptosis, miosis and anhidrosis of the corresponding half of the face or the entire half of the body. Enophthalmos, as a rule, is weakly expressed, the impression of it is created mainly due to the narrowing of the palpebral fissure. Less permanent symptoms are homolateral disruption of tear secretion, heterochromia of the iris.
The clinical picture of Bernard-Horner syndrome includes:
- ptosis is a narrowing of the palpebral fissure due to paralysis or paresis of the levator muscle of the upper eyelid, specifically the Müller muscle, which receives sympathetic innervation.
- miosis is a narrowing of the pupil due to paralysis or paresis of the pupillary dilator and the predominance of parasympathetic innervation of the pupillary sphincter. Miosis is clearly visible in dim lighting, the reaction of the pupils to light and accommodation are preserved.
- enophthalmos - caused by paralysis or paresis of the orbital muscle of the eye, which receives sympathetic innervation; the fibers of this muscle are woven into the connecting membrane that covers the lower orbital fissure; weakening the tension of this membrane can lead to slight enophthalmos.
- hyperemia of the conjunctiva, dilation of the vessels of the corresponding half of the face due to the vascular smooth muscles of the eye and face, loss or insufficiency of sympathetic vasoconstrictor reactions.
- Other symptoms may develop: anhidrosis, increased skin temperature, as well as depigmentation of the iris (in the case of congenital syndrome).
Causes of the syndrome
It is observed with damage to the central sympathetic pathway, the ciliospinal center and its connections with the superior cervical sympathetic ganglion, the superior cervical sympathetic ganglion and postganglionic fibers on the way to the eye.
In addition, the syndrome develops when the cerebral hemispheres are damaged (massive infarction, etc.), or the brain stem. In the latter case, the syndrome is often combined with a disorder of pain and temperature sensitivity on the opposite side of the body. The causes may be vascular diseases, multiple sclerosis, pontine glioma, encephalitis, etc. The sympathetic pathway in the cervical part of the spinal cord is often involved in the pathological process in syringomyelia and spinal tumors. In these cases, a disorder of pain sensitivity and loss of reflexes in the hand are usually observed.
The cause may also be a primary or metastatic tumor in the upper lobe of the lung (Pancoast syndrome), rarely with osteochondrosis of the spine, cervical rib, or damage to the lower primary trunk of the brachial plexus (Dejerine-Klumpke palsy). Damage to the cervical sympathetic trunk may be associated with enlarged cervical lymph nodes, previous operations on the larynx, thyroid gland, etc. Malignant neoplasms in the area of the jugular foramen of the base of the skull can manifest as various combinations of Horner's syndrome and lesions of the IX, X and XI cranial nerves.
The incidence of Bernard-Horner syndrome with various regional analgesia techniques ranges from 4% to 75%. In 75% of cases, the syndrome is observed during blockade of the brachial plexus using a supraclavicular approach and, as a rule, has a clear connection with the administration of a large volume of local anesthetic.
There is also evidence for the development of unilateral Bernard-Horner syndrome as a complication of epidural anesthesia in the lumbar region.
This pathological syndrome can develop as a result of various pathological processes, the development of which leads to damage to the sympathetic pathways at the level of the hypothalamus, brain stem, and cervical spinal cord:
- Inflammatory processes in the central nervous system
- Brain and spinal cord injuries
- Tumors of the brain and spinal cord
- Inflammatory diseases of the upper spine
- Inflammatory diseases of the first ribs
- Migraine
- Myasthenia gravis
- Multiple sclerosis
- Stroke (bleeding in the brain)
- Intoxication (primarily alcoholic)
- Trigeminal neuralgia
- Block of the cervical plexus, stellate ganglion
- Tumor located at the apex of the lungs (Pancoast tumor)
- Inflammation of the middle ear
- Aortic aneurysm
- Syringomyelia
- Neurofibromatosis type I
- Hyperpalasia (enlargement) of the thyroid gland due to goiter
- Cavernous sinus thrombosis
- Simatectomy (surgery to cut the sympathetic nerve in the neck)
Anatomical Basics
The descending sympathetic pathway goes from the hypothalamus through the brain stem and cervical part of the spinal cord, then leaves the spinal canal along with the anterior roots (CVI-ThI-ThII) and returns to the skull. For ease of description, the portion of the path between the hypothalamus and the cervical ciliospinal center is called the first neuron (although it is probably interrupted by several synapses in the region of the pons and tegmentum of the midbrain). The area from the ciliospinal center to the superior cervical ganglion is called the second neuron; the area from the superior node to the muscle that dilates the pupil is the third neuron. Preganglionic fibers (second neuron) Cell bodies lie in the gray intermediolateral columns of the lower cervical and upper thoracic segments of the spinal cord, forming the so-called ciliospinal center of Budge.
In humans, most of the preganglionic fibers innervating the eye leave the spinal cord along with the anterior roots of the first thoracic segment. A small part may also be part of the roots СVII and ThII,V. From here, through the white connecting branches, the fibers pass to the paravertebral sympathetic chain. Then, without forming synapses, they continue upward and pass through the lower and middle cervical nodes, eventually reaching the upper cervical ganglion.
The superior cervical ganglion, which is the confluence of the first four cervical sympathetic ganglia, is located between the internal jugular vein and the internal carotid artery, below the base of the skull (i.e., somewhat higher than is usually believed). Oculosympathetic and sudomotor fibers of the face form synapses here.
Postganglionic fibers (third neuron) Fibers that innervate the dilator muscle leave the ganglion and accompany the internal carotid artery in the carotid canal and foramen lacerum, reaching the trigeminal ganglion region. Sympathetic fibers are close to the internal carotid artery in the cavernous sinus. Most of them connect to the ophthalmic part of the trigeminal nerve, penetrating the orbit with its nasociliary branch. The long ciliary nerves leave this branch, bypass the ciliary ganglion, pierce the sclera and choroid (both nasally and temporally) and eventually reach the muscle that dilates the pupil.
Postganglionic sympathetic fibers also pass to other structures of the eye. Those that innervate blood vessels or uveal chromatophores of the iris are involved in the formation of the initial part of the postganglionic pathway. They leave the nasociliary nerve as the “long roots” of the ciliary ganglion, passing through these structures (without forming synapses) on the way to their effector organs.
Most of the sudomotor and piloerection fibers innervating the facial region leave the superior cervical ganglion and reach their destination, passing through a plexus located along the external carotid artery and its branches.
Diagnostics
There are several diagnostic tests to identify Horner's syndrome:
- Instillation of an M-anticholinergic solution into both eyes, which will lead to anisocoria. This is due to the fact that on the healthy side the pupil will dilate, but on the sick side it will not.
- Instillation of drops with an alpha-adrenergic agonist (for example, aproclonidine, cocaine hydrochloride) into the eyes also leads to pupil dilation in the healthy eye (mydriasis), in the absence of such a process on the side of the pathological process.
- Test with oxamphetamine - will reveal damage to the third neuron of the sympathetic pathway.
- Determination of the delay time of pupil dilation - determined using the direction of the light beam using, for example, an ophthalmoscope. Anisocoria is observed in Horner's syndrome.
- Magnetic resonance imaging, computed tomography, x-ray examination are used to identify pathological formations that contribute to the development of Horner's syndrome.
Our doctors
Pankov Alexander Rostislavovich
Neurologist
40 years of experience
Make an appointment
Novikova Larisa Vaganovna
Neuropathologist, Candidate of Medical Sciences, doctor of the highest category
Experience 39 years
Make an appointment
Forecast of drooping eyelid
As a rule, ptosis requires either treatment of the disease that caused it, or purely cosmetic correction, or both.
When treated for cosmetic purposes, the prognosis is favorable. If surgical treatment was performed on a child, then he is monitored periodically throughout his growth period. For myasthenia gravis, the selection of adequate therapy or complete cure for myasthenia gravis can eliminate ptosis. With the exception of cases where, due to prolonged drooping of the eyelid, overstretching of the muscle tendon has occurred, then the defect becomes purely cosmetic and is eliminated surgically.
In all other cases of neurological pathology (syncinesia, neuropathy, facial nerve paralysis, myopathy), the prognosis depends entirely on the initial disease and the prognosis for its treatment.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions