Cervicocranialgia; Barre-Lieu syndrome; spinal nerve syndrome; Cervical migraine, vertebral artery syndrome; Neuritis of the sympathetic vertebral nerve - under such names can be found in foreign and domestic medical literature - Posterior cervical sympathetic syndrome.
The syndrome described above is generally considered to be a functional stage of vertebral artery syndrome. Vertebral artery syndrome refers to cerebrovascular diseases that lead to vascular disorders of cerebral circulation. Brain strokes are the main cause of disability and mortality among the adult population of planet Earth!! This problem, which is extremely unfavorable in epidemiological terms, also exists in Ukraine.
- The reasons are impaired blood circulation in the vertebral arteries, compression of blood vessels in the cervical spine.
Clinical picture
Headache in the cervico-occipital region, radiating to the parietal, temporal, fronto-orbital and ear regions, more often on one side. The headache is throbbing, aching, burning in nature and is provoked by head movements. Often, cervicocranialgia is combined with short-term vestibulo-cochlear disorders (balance disorders), sometimes with transient visual (blurred vision, darkening of the eyes). Physical and mental performance decreases sharply.
Vertebral artery syndrome. Pain, a feeling of numbness, a “crawling sensation” in the cervical-occipital region with irradiation to the anterior parts of the head, parietal, temporal, and postauricular regions. There is a sensation of a foreign body in the eye on the affected side, dizziness, nausea (or vomiting), congestion in the ear, tinnitus. There may be sensations of falling through, surrounding objects falling on the patient, a transient decrease in visual acuity, the patient falling without loss of consciousness - falls of the dropp attack type. Unsteadiness when walking. Possible increase in body temperature. General weakness, increased irritability, mood instability, feeling of heaviness in the head, sleep disturbances, memory problems.
Diagnosis and treatment of cervical syndromes
As an example, consider posterior cervical sympathetic syndrome. It is also called vertebral artery syndrome or cervical migraine. Its cause is compression of the nerve endings that lead to large blood vessels designed to supply the brain. Neck pain in this case is accompanied by headache and dizziness.
Specifics of the development of syndromes in the neck area
The main cause of pain is compression of nerve endings and squeezing of blood vessels. These syndromes occur due to previous injuries (dislocations and fractures of the shoulder, collarbone, injuries to the cervical spine or shoulder girdle). Also, the cause of the syndrome can be osteochondrosis and other diseases of the degenerative-dystrophic type.
There is nothing specific about the diseases themselves. However, their localization leaves an imprint - treatment of the cervical spine is quite difficult. The neck is one of the most vulnerable areas of the body. After all, many channels important for life pass through a small space - respiratory, circulatory, and so on. And even slight compression or injury to this area is accompanied by severe pain.
But the most dangerous thing is that when the nerve endings are compressed, the internal organs whose innervation passes through this channel begin to work worse. Symptomatic treatment of the organ itself in this case does not bring results. And in the absence of treatment, the situation becomes more and more serious.
What pain syndromes are included in the complex?
Although all cervical syndromes have similar features, each one is different from the others. At the same time, the goal of any treatment should be considered not to eliminate pain, but to eliminate its cause.
The most common cause of the lesion is osteochondrosis. And it is almost impossible to cure it completely today. But correct treatment eliminates pain, reduces the amount of compression, and returns a person to normal life.
The most common problems
Radicular syndrome is the most common, and its symptoms are very unique. First of all, this is, of course, neck pain. But a pinched nerve can have the most unexpected consequences. And the pain can appear far from the place of infringement. Your lower back, arm, or leg may hurt. But the worst thing is that pain can imitate signals that appear in organic diseases. For example, heart pain, characteristic of angina pectoris. But treatment of such pain in internal organs with conventional drugs does not give any effect.
To understand the picture of the disease, treatment should be carried out by an experienced specialist, since the nature of pain in the syndrome is somewhat different. For example, with angina pectoris, the pain is felt in attacks and is short-lived. With radicular syndromes, the pain lasts much longer, up to several hours in a row.
One of the most dangerous cervical syndromes is considered to be posterior cervical sympathetic or “cervical artery syndrome.” When it occurs, compression of the vessels supplying the brain with blood occurs. Consequently, not only pain in the neck appears, but also problems with hearing and vision, the functioning of the vestibular apparatus worsens, and the heart muscle becomes tense.
How are cervical syndromes treated?
It is difficult to treat this area due to the impossibility of using the full range of treatment methods. For example, cervical massage is performed very limitedly. You also need to use vasodilators and medications for dizziness in addition to non-steroidal anti-inflammatory drugs.
To relieve compression, special neck corsets are used. However, they have a side effect - wearing them weakens the neck muscles, so mandatory therapeutic exercises are required so that neck mobility does not decrease in the future and compression does not develop again.
Traumatic injuries
Another variant of the disease is cervicocranial syndrome. It occurs due to head injuries or chronic stress on the neck area. In this case, the functioning of the intervertebral joints is disrupted, and the pain receptors of the muscles and ligaments are irritated.
The symptoms are largely similar, and the treatment is expected to be similar.
The main difference is that the cause of the syndrome is not a chronic disease. So it can be completely cured. The main thing is to remove stress from the affected area in time and prevent the disease from becoming protracted. Using bandages together with drug treatment can quickly overcome the disease. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Clinical variants of ShCS
ShCS are divided into radicular (radiculopathy), spinal (myelopathy) and neurovascular (vertebral artery syndrome) syndromes.
Radiculopathies
Nociceptive afferentation entering various parts of the central nervous system triggers a complex of integrative responses, evolutionarily aimed at the functional immobilization of the affected parts. This is a muscular-tonic tension of para- and extravertebral skeletal muscles. The classic manifestation of NK compression is shooting pain, dermatomal hypalgesia, peripheral paresis, weakening or loss of reflexes. Radicular pain increases with coughing, sneezing, and body movements, especially when bending and turning. Only the detection of one of these signs or their combination makes it possible to diagnose the participation of the radicular component in the picture of cervicobrachialgia along with spondylogenic and musculofascial pain [5]. Tension symptoms for radicular lesions are nonspecific. Compression of each NK is associated with certain motor, sensory and reflex disorders.
Damage to C1 NK (cranio-vertebral spinal motion segment) is manifested in the clinic by pain and impaired sensitivity in the parietal region.
Lesion of the C2 NK (segment CI–II) is characterized by pain in the parietal and occipital regions.
Lesion of C3 NK (segment CII–III) is rare. Pain and decreased sensitivity occur in the half of the neck where the spinal nerve is pinched; decreased sensitivity of the tongue and paresis of the hypoglossal muscles are possible (since there is an anastomosis with the hypoglossal nerve); accordingly, speech impairment and uncontrolled language proficiency are likely.
Lesion of C4 NK (segment CIII–IV). Characterized by pain and decreased sensitivity in the shoulder girdle and collarbone, hypotonicity of the muscles of the head and neck (belly, trapezius, levator scapulae). Since this NC contains the phrenic nerve, respiratory problems, hiccups and pain in the heart and liver are possible.
Lesion of C5 NK (segment CIV-V). Occurs in approximately 5% of cases of cervical radiculopathy and is usually caused by C4-C5 disc herniation. Pain occurs, spreading to the shoulder girdle, the outer surface of the shoulder. Possible weakness and impaired trophism of the deltoid muscle. Paresis may affect the levator scapulae, rhomboids, serratus anterior, supraspinatus, infraspinatus, deltoid, biceps, and brachioradialis muscles, which are involved in varying combinations. Reflexes from the biceps brachii and brachioradialis muscles may be weakened. There is a violation of the sensitivity of the outer surface of the shoulder.
Lesion of C6 NK (segment CV–VI). It is observed in approximately 20–25% of cases of cervical radiculopathy and is most often a consequence of C5–C6 disc herniation. The pain spreads from the neck along the shoulder blade, forearm, outer surface of the shoulder, radial surface of the forearm to the thumb. Paresis may primarily affect the biceps brachii muscle; much less commonly, the serratus anterior, pronator teres, flexor carpi radialis, brachioradialis, extensor carpi radialis longus, supinator and extensor carpi radialis brevis muscles are affected. A decrease in tendon reflexes from the biceps brachii and brachioradialis muscles is determined. Sensitivity is impaired in the corresponding segment of the skin along the lateral surface of the hand, especially in the area of the 1st and 2nd fingers.
Lesion of C7 NK (segment CVI–VII). It is observed in approximately 60% of cases of cervical radiculopathy, most often in connection with a C6–C7 disc herniation. The pain spreads from the neck along the shoulder blade, forearm, back of the shoulder, dorsal surface of the forearm to the back of the II–IV fingers. Paresis involves the triceps muscle, but the serratus anterior, pectoralis major, latissimus dorsi, pronator teres, flexor carpi radialis, long and short extensor carpi radialis and extensor digitorum muscles may be affected. Since the innervation of the triceps muscle is disrupted, a decrease in the tendon reflex is observed. Sensitivity disorders are localized in the area of the third and fourth fingers of the hand. In rare cases, it is possible to develop the phenomenon of pseudomyotonia, which is characterized by the inability to quickly unclench a fist. When trying to unclench the fingers, their paradoxical flexion occurs, probably associated with abnormal regeneration of the root fibers.
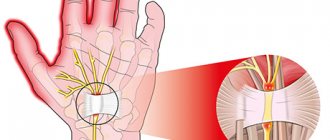
Lesion of C8 NK (segment CVII–TI). It occurs in approximately 10% of cases of cervical radiculopathy and is most often caused by C7-T1 disc herniation. Pain and loss of sensitivity spread from the neck to the shoulder, elbow to the little finger. Possible wasting of the muscles of the eminence of the little finger. Paresis may extend to the flexor digitorum superficialis, flexor pollicis longus, flexor digitorum profundus I–IV, pronator quadratus, abductor pollicis brevis, oppons pollicis, all lumbrical muscles, flexor carpi ulnaris, abductor pollicis, abductor pollicis, , Opposite little finger, flexor little finger, interosseous muscles, adductor pollicis, extensor of the little finger, extensor carpi ulnaris, abductor pollicis longus, extensor pollicis brevis and longus, and extensor of the index finger. Weakness of the hand muscles is observed only when the C8 root is affected. The reflex from the finger flexors may decrease; due to damage to the sympathetic fibers following the superior cervical ganglion, ipsilateral Horner's syndrome is possible.
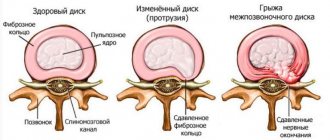
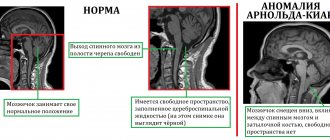
Discogenic cervical myelopathy
The cause of myelopathy (damage to the spinal cord) is most often herniated protrusions of intervertebral discs, proliferation of vertebral bodies (osteophytes), and hypertrophied ligamentum flavum. In its course, cervical myelopathy with osteochondrosis of the cervical spine resembles extramedullary tumors of the spinal cord. More often it has a progressive, less often intermittent with remissions and stationary course. The disease in most cases lasts a long time – years. As a rule, typical patient complaints are pain, numbness and weakness in the arms and legs. Often, when moving the head, there is an unpleasant sensation of electric current passing from the neck to both arms and along the spine to the legs (Lhermitte’s symptom).
Vertebral artery syndrome
Irritation of the efferent sympathetic fibers of the plexus causes vasospasm. There are two variants of vertebrogenic syndrome of the vertebral artery: compression-irritative and reflex angiospastic. With the compression-irritative variant, narrowing of the vessel is possible not only due to spasm, but also as a result of mechanical action on its wall - compression of the artery.
The reflex angiospastic variant is characterized by:
• bilaterality and diffuseness of cerebral vegetative-vascular disorders;
• predominance of vegetative manifestations over focal ones;
• relatively less connection between seizures and head rotation.
Compression-irritative syndrome is more common in pathologies of the lower cervical spine and is combined with brachial pectoral syndromes, while reflex syndrome occurs when the upper and middle cervical levels are affected.
When organic disturbances in brain function appear, they speak of the organic stage of the syndrome, and in their absence - of the functional stage. The functional stage of vertebral artery syndrome is characterized by three groups of symptoms: headache (and accompanying autonomic disorders), cochleovestibular disorders in the form of paroxysmal non-systemic dizziness, visual disturbances (darkening in the eyes, sensation of sand, sparks and other photopsies, slight changes in the tone of the fundus vessels).
Headache, pulsating or cerebral, aching, burning, constant and intensifying in attacks, especially when moving the head or its prolonged forced position, spreads from the back of the head to the forehead. The patient, showing this zone on himself, makes a movement with his palm, as when removing a gas mask - a symptom of removing a helmet. The pain is reproduced or intensified by pressure, especially when tapping the point of the vertebral artery. On the sore side, other vascular points are also painful - the temporal branch of the external carotid artery (to the greatest extent), the branches of the ophthalmic artery along the inner-superior corner of the orbit. Often the scalp is painful even with a light touch or combing the hair.
In conditions of prolonged and intense vascular spasms, the development of foci of persistent ischemia is possible - the organic stage of vertebral artery syndrome. It manifests itself as transient and persistent circulatory disorders in the brain and spinal cord. Short-term ataxic disorders, nausea, articulation disorders and other loss of function from the IX-X or other cranial nerves are possible. There are forms of transient cerebral ischemia, most often observed with vertebrogenic lesions of the vertebral arteries. They often occur when turning or tilting the head. First of all, these are attacks of sudden falling while maintaining consciousness and fainting (syncope) attacks. The first last for one to two minutes, the second last longer. The return of consciousness occurs faster in a horizontal position. After an attack, in addition to general weakness, headaches, tinnitus, photopsia, and severe autonomic lability are observed. The attacks are caused by paroxysmal ischemia of the brain stem, its reticular formation (during syncope attacks) and in the area of the intersection of the pyramids (during attacks of falling).