General information
Hyperventilation syndrome is one of the types of disorders of the autonomic nervous system, which is manifested by difficulty breathing.
The pathology is quite common and is diagnosed in approximately 15% of the population. Hyperventilation syndrome is in no way associated with diseases of the pulmonary system, bronchi or heart. The feeling of lack of air occurs solely against the background of disruption of the autonomic nervous system , which is responsible for the vital processes of the body that are beyond the control of our consciousness.
A person can control the frequency and depth of breathing only for a certain time. Breathing can be deep and shallow, rare and frequent, with or without delay.
The pathology occurs in people of various age groups, but the peak incidence is recorded in people 30-40 years old. Females among patients are 4-5 times more common than males. The syndrome is characterized by a predominantly chronic course, with acute cases accounting for only 2% of calls.
Pathogenesis
The psycho-emotional state of a person quite strongly influences the functioning of the respiratory system. Various psychogenic triggers (for example, anxiety) lead to biochemical shifts that affect the balance of calcium and magnesium. The development of hyperventilation is potentiated by changes in the functioning of respiratory enzymes.
Due to excessive release of carbon dioxide, its concentration in the blood decreases, which leads to a shift in pH to the alkaline side, hypocapnia and the development of respiratory alkalosis . Against the background of the changes described above, specific symptoms appear:
- tetany;
- algic disorders;
- disturbances of consciousness;
- autonomic and sensory disorders.
The result is increased anxiety, which supports hyperventilation. Even after eliminating the provoking etiological factor, the vicious circle continues to exist and negatively affect the patient’s health.
Reanimatology School of Professor Sergei Vasilievich Tsarenko
A typical example of contradictions between therapeutic doctrines is the use of hyperventilation for therapeutic purposes. Hyperventilation causes hypocapnia, which increases cerebral vascular tone. An increase in vascular tone leads to a decrease in blood volume in the cranial cavity and a decrease in ICP. A number of early experimental and clinical studies showed that hyperventilation can reduce ICP due to vasoconstriction and a decrease in blood volume in the brain (SS Kety, CF Schmidt, 1948; N. Lundberg et al., 1959). Evidence of neurological improvement after hyperventilation was also established (A. Bricolo et al., 1972; TW Langfitt, NF Kassel, 1966).
There is also a flip side to the coin. A decrease in blood supply due to an increase in vascular tone may be accompanied by a decrease in cerebral blood flow, already compromised due to compression of blood vessels by the edematous brain. In this regard, modern studies have failed to confirm the usefulness of hyperventilation, at least when used prophylactically.
The use of hyperventilation caused a decrease in hemoglobin oxygen saturation in blood flowing from the brain and an increase in the arteriovenous oxygen difference in healthy people, as well as in patients with TBI (SP Gopinath et al., 1994). These facts indicated a discrepancy between the supply of oxygen to the brain and the need for it, in other words, a lack of blood flow. Hyperventilation was especially dangerous at initially low levels of oxygen tension in brain tissue (рtiO2), which was most often observed in the first two days after injury and after the sixth day (J. Meixensberger et al., 1997). Based on this, a number of authors propose to completely abandon the use of hyperventilation in the treatment of patients with TBI. A class I randomized prospective trial examining the prophylactic use of hyperventilation in TBI (JP Muizelaar et al., 1991) showed a negative effect of this treatment on long-term outcomes of brain injury.
To relieve excess blood supply to the brain (cerebral hyperemia), they are currently trying to use dosed hyperventilation within the so-called concept of “optimized hyperventilation” (J. Cruz, 1998).
According to this concept, hyperventilation should not be used prophylactically, but only when diagnosing brain hyperemia. The basis for this approach is experimental and clinical data on phase changes in cerebral blood flow during TBI. In the first 24-36 hours after TBI, a decrease in cerebral blood flow is observed. Over the next 2-3 days, a number of patients develop excessive or so-called “luxurious perfusion”. The essence of the phenomenon is that there is an increase in cerebral blood flow, excessive in relation to the needs of the affected brain. Excessive blood flow may be accompanied by excessive blood filling of the cerebral vessels due to the lack of a compensatory increase in their tone. As a result, intracranial hypertension develops, the mechanism of which is brain hyperemia. The logical treatment in this situation is the use of hyperventilation. J. Cruz considers safe the level of hyperventilation that does not lead to increased arteriovenous oxygen difference. However, assessment of hemoglobin oxygen saturation in the jugular vein reflects cerebral blood flow and does not take into account regional differences. Experimentally (DF Wilson et al., 1992) and clinically (JB Salvant, JP Muizelaar, 1993) the heterogeneity of changes in blood flow and metabolism in the brain during TBI has been established. The mosaic nature of the regional sensitivity of cerebral vessels to changes in carbon dioxide tension in arterial blood has been proven (DW Marion, GJ Bouma, 1991). These data indicate that the problem of the effective and safe use of hyperventilation cannot be solved entirely on the basis of an assessment of hemoglobin saturation in the blood flowing from the brain. ‹ 2.6. Conflicts of doctrines.Up2.6.2. Sedatives, narcotic analgesics and muscle relaxants. ›
Classification
Pathological types of breathing:
- terminal;
- periodic;
- dissociated.
Types of periodic breathing:
- Biota;
- Cheyne-Stokes;
- wavy.
Periodic breathing is characterized by alternation of respiratory movements and pauses in the form of apnea . The pathology occurs against the background of a disorder of the automatic respiratory control system.
Terminal breathing types include:
- gasping breath;
- apnestic breathing;
- Kussmaul's breath.
Pathological terminal types of breathing are accompanied by gross disturbances of rhythmogenesis. Kussmaul breathing is characterized by a deep inhalation followed by an extended, forced exhalation. Kussmaul is described as deep and noisy breathing, which is recorded in unconscious patients due to uremic, diabetic or hepatic coma. Kussmaul breathing is triggered due to a pathology of excitability of the respiratory center in individuals with cerebral hypoxia , metabolic acidosis and toxic phenomena .
Dissociated breathing is characterized by:
- asymmetry of the right and left halves of the chest;
- paradoxical movements of the diaphragm.
Da Costa syndrome is named after the monk and is manifested by a paroxysmal increase in pulmonary ventilation, which is accompanied by changes in consciousness, pain, sensitivity, muscle-tonic and autonomic disorders. Da Costa syndrome occurs after psychological trauma in the form of acute and chronic stress.
How can I install a hot water supply?
The purpose of diagnosis is to establish the causes of hypoventilation syndrome and prescribe treatment. To confirm this diagnosis, the doctor must collect the patient’s medical history and perform an examination. Typically, the patient complains of pain in various systems and organs - stomach, heart, lungs. To begin with, it is worth examining the organs that the patient is complaining about. This is possible with the help of ultrasound examination, electrocardiogram, computed tomography and magnetic resonance imaging.
A qualified doctor will be able to find a logical connection between complaints about pain in certain organs, the emotional state of the patient and draw up an appropriate picture of the disease. If hyperventilation is suspected, the patient is usually asked to take a deep breath and exhale. This should be enough to determine the diagnosis.
Electromyography involves taking samples for muscle spasms, and specialized blood serum tests can detect changes in the acidic environment of the blood. Experts even created a specialized survey, which helps to diagnose “hyperventilation” in 95% of cases.
Electromyography involves taking samples for muscle spasms
It is worth remembering that any one detected sign does not at all mean that the patient has HVS. Respiratory system problems may indicate other serious illnesses. Only a doctor's examination and a comprehensive examination can determine the correct diagnosis.
Causes
Hyperventilation syndrome occurs due to the combination of the respiratory regulation system. During periods of stress, or when the patient is overtired or afraid, the depth and rhythm of breathing movements changes involuntarily, which leads to a feeling of lack of air. This is what provokes panic attacks , which further aggravate the course of hyperventilation syndrome.
Also, increased suspiciousness or the patient’s exposure to outside influences can lead to pathological breathing. For example, an attack of suffocation may occur after a person has seen an attack of bronchial asthma in another patient. This event can be recorded in memory and even after a few years lead to the formation of hyperventilation syndrome.
Etiological factors:
- Organic. These include various lesions of the central nervous system (dyscirculatory encephalopathy , hydrocephalus , arachnoiditis ), as well as diseases of internal organs (recurrent bronchitis , arterial hypertension , diabetes mellitus ). The influence of only organic factors occurs in 5% of patients with hyperventilation syndrome.
- Psychogenic. They are provoked by mental disorders ( neurasthenia , depression , anxiety or phobic disorders, and extremely rarely – hysterical neurosis ). Pathology can develop against the background of acute and chronic stressful situations. In some cases, the syndrome develops as a result of psychogenic behavior in childhood, when the child witnessed an episode of suffocation of a drowning person or asphyxia .
- Mixed. In these cases, the psychogenic trigger is triggered in response to organic pathology. Occurs in 35% of cases.
Hyperventilation syndrome can also be triggered by taking certain medications (methyl xanthine derivatives, salicylates, beta-agonists, progesterone ).
Symptoms of pulmonary hyperventilation syndrome
The main manifestation of hyperventilation syndrome is a variety of breathing problems, which are accompanied by an attack of irrational anxiety and uncontrollable fear. At the moment of crisis, the subject feels that he does not have enough oxygen to breathe. To feel satisfied, he needs to take frequent deep breaths.
Hyperventilation of the lungs in many patients is manifested by arrhythmic breathing. During an attack, the individual experiences severe yawning and hiccups. Psychogenic shortness of breath occurs, not associated with physical movements.
The patient may feel that he has lost the automaticity of breathing. He has to control his breathing process. To perform each inhalation and exhalation, he makes volitional efforts.
Another sign of pulmonary hyperventilation syndrome is the feeling of a present obstacle to breathing movements. A person may feel like there is a foreign object stuck in their airway. He may feel that the muscles of his larynx are in spasm. At such a moment, a person develops an obsessive fear of premature death from an attack of suffocation.
This type of organ neurosis is often accompanied by unpleasant manifestations of the heart. The patient may indicate the occurrence of cardialgia - pain in the heart area radiating to the left shoulder. A common complaint is a change in the rhythm of the heartbeat. The patient feels that his organ is beating irregularly and “freezes” for a while. Some patients indicate an acceleration of the heart rate. They feel a pulsation in the neck area. Unpleasant sensations are often perceived by the patient as severe cardiac pathology.
During an attack, a person may feel dizzy and unstable in the position of their body in space. He may have anticipation of impending fainting.
With pulmonary hyperventilation syndrome, psychotic symptoms and cognitive defects develop. Very often, patients indicate problems with sleep, complaining that it is very difficult for them to fall asleep at a set time. Patients note difficulties concentrating: fixation on internal sensations does not allow such people to concentrate on completing the current task.
The psycho-emotional status of a person changes. The patient is in a gloomy, melancholy mood. He becomes nervous and irritable. Very often he demonstrates hostility and aggression towards others.
Some people, obsessed with the fear of dying from suffocation, begin to be afraid to stay in cramped and enclosed spaces. Other people are afraid to be alone even for a short time, since the presence of other people for them is a guarantee of timely assistance in the event of an attack.
Anxiety and depression become significantly worse as pulmonary hyperventilation syndrome develops. A person ceases to lead a full life, refuses many activities, being in the grip of his destructive experiences. Against the backdrop of poor health, he may have ideas about the meaninglessness of existence. Severe depression can lead to complete social isolation and lead to suicide attempts.
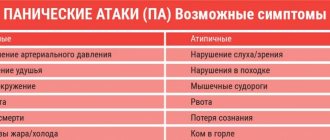
Symptoms of hyperventilation syndrome
The disease is characterized by polymorphism and a multiplicity of symptoms. However, it is customary to distinguish a typical triad in the clinical picture of HVS:
- emotional disturbances;
- respiratory dysfunction;
- muscle-tonic phenomena.
There are 4 forms of breathing disorder:
- Empty breath is a subjective feeling of lack of air, which encourages the patient to breathe more often and deeper.
- Labored breathing. Patients describe the condition as “a lump in the throat”, “stiffness when inhaling.” It takes some effort to take a full breath. Accessory muscles take part in the act of breathing, and arrhythmic increased breathing is recorded.
- Respiratory automaticity disorder. It seems to the patient that breathing stops, which encourages him to independently control the breathing process and correct it.
- The use of hyperventilation equivalents (coughing, yawning, deep sighs, sniffling).
Psycho-emotional disorders are manifested by feelings of fear and anxiety. The most commonly reported disorder is generalized anxiety disorder . Patients complain of loss of the ability to relax on their own, note increased anxiety and constant nervous tension. Quite often, fear of public places (social phobia) and open spaces (agoraphobia), aggravated by respiratory disorders, is detected.
Muscular-tonic syndrome develops due to changes in the electrolyte composition of the blood, which is responsible for neuromuscular excitability. Patients complain of " paresthesia ", which is manifested by burning, numbness, tingling and a crawling sensation. Tetanic phenomena also appear in the form of muscle spasms and tonic convulsions in the distal limbs. Carpopedal spasm is extremely rarely recorded.
Classic symptoms of hyperventilation:
- cardialgia;
- headache;
- pain in the epigastric region;
- dyspepsia;
- confusion;
- cardiopalmus;
- syncope.
Symptoms
Hyperventilation syndrome often has a crisis course, that is, its symptoms appear quite suddenly, last for a certain period of time (several minutes or hours) and recede. After some time, the attack repeats.
A typical picture of a hyperventilation crisis looks like this. The patient experiences anxiety and fear for no apparent reason. At the same time or a little later, shortness of breath appears, a feeling of lack of air (they swallow air, frantically opening their mouth), the inability to take a deep breath, a lump in the throat. Breathing quickens. The fear intensifies, the patient thinks that death will overtake him now. Cardiovascular disorders occur (chest pain, rapid heartbeat, increased blood pressure). The patient panics. In addition to respiratory and cardiovascular disorders, other symptoms may appear.
All symptoms of hyperventilation syndrome can be divided into several groups:
- vegetative (respiratory, cardiovascular, gastrointestinal disorders, urinary disorders);
- changes in consciousness;
- muscular-tonic and movement disorders;
- pain and other disturbances from the sensory organs;
- mental disorders.
Let's take a closer look at each group of symptoms.
Respiratory disorders
Respiratory disorders can be very diverse. They constitute the main clinical component of a hyperventilation crisis. These are symptoms such as:
- a feeling of lack of air (oxygen), dissatisfaction with inhalation, a feeling of its ineffectiveness. The patient is fixated on his breathing, fresh air, “breathing hygiene,” that is, on correcting environmental factors that will provide him with a full breath. Patients complain of an irrepressible desire to breathe deeply, which is impossible, in their opinion, although they try. If they succeed in taking such a breath, they focus on it, as if confirming the reality of their violations, although in fact this “deep” breath is no different from the others. Typically, the actual breathing in such patients is rapid and deep, with a normal rhythm of inhalation and exhalation. In stressful situations, the degree of fixation on one’s feelings increases;
- loss of automatic breathing. It seems to the patient that if he does not monitor his breaths, that is, if he does not reproduce them with volitional effort, then independent respiratory activity will stop. “I will stop breathing and I will suffocate,” this is what such a patient says about himself;
- a feeling of being unable to take a full breath as a result of some obstacle (lump in the throat, tightness of the chest). With this type of respiratory disorder, patients are also fixated on their breathing, but more at its individual stages (rather than on environmental factors, as described above), that is, they look for the cause in themselves (“remove the lump”, “relax the chest muscles”). . Objectively, breathing in such patients is frequent, with an irregular rhythm of alternating inhalation and exhalation, with the participation of auxiliary muscles (those that are not normally involved in the act of breathing). Clinically, this looks like an attack of suffocation during asthma, so this variant of respiratory disorders is sometimes called atypical asthma, but upon auscultation (listening) no respiratory sounds characteristic of a real asthma attack are detected;
- periodic sighs, coughing, yawning, sniffling. Naturally, this does not mean occasional yawning or snoring, or isolated episodes of coughing, but a systematic, causeless repetition of these actions. These manifestations of respiratory disorders do not occur during a crisis of hyperventilation syndrome. They are not noticed by the patient himself, do not cause him discomfort, and usually those around him pay attention to this. However, such minor changes are sufficient to alter the normal blood gas state and disturb the pH.
Respiratory symptoms are always present in the picture of hyperventilation syndrome. Manifestations from other organs and systems can range from absence at all to pronounced manifestations.
Cardiovascular disorders
Such changes often accompany hyperventilation crises. Such violations include:
- pain in the region of the heart of various types (stabbing, shooting, squeezing, aching);
- feeling of heartbeat;
- chest pain, feeling of constriction;
- discomfort in the heart area;
- changes in blood pressure;
- heart rhythm disturbances (usually extrasystoles);
- possible changes in the ECG (elevation of the S-T segment);
- headache;
- dizziness, unsteadiness when walking;
- noise in the ears and head, short-term hearing loss;
- bluish coloration of hands and feet;
- increased sweating;
- Raynaud's syndrome (due to vasospasm).
Gastrointestinal disorders
Manifestations from the gastrointestinal tract almost always accompany hyperventilation syndrome. It can be:
- changes in peristalsis (usually in the direction of intensification) and, as a consequence, frequent bowel movements up to diarrhea; much less often - constipation;
- swallowing air when eating and belching air (aerophagia);
- bloating, flatulence, rumbling in the stomach;
- nausea, vomiting;
- intolerance to any food products (to which previously, before the disease, the patient was quite calm);
- stomach ache.
Urinary disorders
This type of disturbance directly accompanies a hyperventilation crisis. The changes are most pronounced towards the end of the crisis. This is a frequent urge to urinate with the release of large amounts of light-colored urine.
Changes in consciousness
This group of disorders includes such disorders of consciousness as:
- fainting;
- pre-fainting states: darkening in the eyes, “spots”, “fog” before the eyes, narrowing of the visual fields (including looking through binoculars), blurred vision, transient blindness;
- the feeling of déjà vu (déjà vu) – “already seen.” There may also be a feeling of “already heard”, “already experienced”, “never seen”, “never heard”. That is, there is an obsessive feeling that similar events have already happened (or have not happened);
- a feeling of loss of reality: a person is lost in reality, he imagines himself in some kind of parallel world (a fairy tale, a horror film, and so on). This state is called derealization;
- a feeling of loss of personality, of becoming someone else, that is, a situation where “I” is not “I.” The name of this condition is depersonalization.
Musculoskeletal and movement disorders
These disorders in 90% of cases are accompanied by hyperventilation crises. They look like this:
- trembling in the arms and legs;
- internal trembling with sensation of heat or cold;
- convulsive muscle spasms (contractions): the most common is the so-called carpopedal spasm. This is when the hand takes on the appearance of an “obstetrician’s hand” and/or the foot flexor muscles sharply contract. “Obstetrician’s hand” - fingers are brought together (gathered as if you are taking a pinch of something) and slightly bent;
- increased readiness for muscle contractions. It is checked by tapping the face below the zygomatic arch with a neurological hammer (Chvostek's sign).
Pain and sensory disorders
These disorders develop in 100% of cases with hyperventilation syndrome. Most often represented by the following phenomena:
- a feeling of numbness in various parts of the body (mainly the face and hands);
- tingling, crawling, burning, twisting;
- “my legs give out”, “I can’t move” and similar sensations;
- the pain component of muscle spasms (that is, all convulsive muscle contractions are accompanied by pain);
- pain in different parts of the body (in the heart, abdomen, head, and so on).
Mental disorders
Mental disorders in this case do not at all mean inappropriate behavior, but only reflect the psychological characteristics of the patient’s condition at the time of crisis:
- anxiety;
- fears;
- anxiety;
- sadness and melancholy;
- emotionality (violent reaction to what is happening around).
Tests and diagnostics
In addition to instrumental diagnostic methods, the most important components when examining a patient are a thorough examination and a detailed history taking. Hyperventilation syndrome is always accompanied by a huge number of complaints about the functioning of organs and systems. The final diagnosis can be made only after the examinations show the absence of organic pathology. It is for this purpose that patients are prescribed spirography, echocardiography, ECG, and ultrasound examination of the abdominal organs.
When you first interview a patient, you can easily identify high emotional tension or a certain amount of anxiety. If a positive result is obtained from a psychogenic test, the doctor may immediately suspect hyperventilation syndrome.
Also, to identify pathology, the patient is recommended to breathe frequently and deeply for 5 minutes. Specific symptoms will appear immediately if the patient actually suffers from HVS. There is also a unique questionnaire that allows you to easily diagnose pathology in 9 out of 10 patients.
The diagnosis cannot be made only based on the results of additional research methods or on the basis of one specific symptom. It is important to remember that disturbances in the respiratory system may also indicate other more serious diseases ( bronchial asthma , heart failure , etc.). Only thanks to the individual approach of the attending physician in combination with modern diagnostic methods can the only correct diagnosis be established.
Hyperventilation
A big problem for society is stress. The constant race for a good life and comfort presents many unpleasant situations closely related to health. At first glance, stress seems like a minor illness, and we often leave this process to chance. We shouldn’t sound the alarm in vain, because stress turns the most unpretentious state of malaise into an irreversible process. Frequent consequences of increased pulmonary ventilation are diseases such as hypertension, terrible headaches in the form of migraines, peptic ulcers of the stomach and duodenum, hyperthyroidism, diabetes mellitus, cancer and pulmonary hyperventilation. Yes, you heard right – hyperventilation.
Let's talk about hyperventilation . This is a scary name at first glance, but it is not a fatal verdict, but a diagnosis that, if dealt with correctly, can be successfully gotten rid of. Hyperventilation is characterized by rapid, deep or shallow breathing. At first, the illnesses, attacks do not last long, about 10 minutes, and go away on their own without the use of any techniques specifically aimed at regulating the breathing rate.
If you do not pay proper attention to all these symptoms, then hyperventilation acquires its crowning place in the human body. What exactly happens during an attack and why do you need to worry so much about the consequences? During a stressful situation, and this could be a simple nervous altercation or fear of something, a large amount of adrenaline and an endless amount of biologically active substances are released in the human body. These substances have a direct effect on the respiratory center. This is controlled by the central nervous system, but more often the situation goes beyond the control of the central nervous system and a crazy heartbeat and increased breathing begin.
Hyperventilation or increased ventilation of the lungs gives rise to the following biochemical processes - rapid breathing enriches the blood with a large amount of oxygen, which in turn pushes carbon dioxide out of the body causing hypocapnia, that is, a decrease in the amount of CO2. The acid-base balance of the blood is disturbed towards alkalization. An attack of oxygen starvation occurs, or in other words, tissue hypoxia occurs.
Hyperventilation produces the following symptoms:
- rapid heartbeat and palpitation,
- anxiety with sleep disturbances,
- feelings of numbness and tingling in the hands, feet, face and other parts of the human body,
- heaviness in the epigastric region with bloating and constant belching,
- general weakness with fainting, etc.
With chronic hyperventilation, all symptoms are aggravated, namely:
- accompanied by severe chest pain,
- spasm of the trachea with a symptom of suffocation,
- increased general body temperature with febrile attacks,
- severe headache with general muscle spasms,
- bleeding from the nose and other types.
What reasons can lead to increased hyperventilation:
- stress of any kind,
- anxiety,
- apathy,
- panic and psychosomatic disorders,
- strong emotions of positive and negative origin,
- alcohol and drug abuse,
- acidosis in liver and kidney failure, etc.
List of somatic diseases leading to increased pulmonary ventilation:
- bronchial asthma with an allergic component,
- chronic lung diseases: obstructive bronchitis, emphysema, bronchiectasis,
- chronic heart failure,
- coronary heart disease and other heart diseases,
- hormonal dysfunction of any etiology,
- climacteric changes,
- benign or malignant brain tumor, etc.
How to diagnose hyperventilation, and what measures should be taken? The first diagnostic step is general and biochemical blood tests. Second computed tomography scan. The third is a chest x-ray. The measures taken are eliminating the source of stress, treating chronic diseases and special breathing exercises. During therapeutic exercises, patients learn proper breathing using a breathing simulator - this is the most important step towards recovery. Attention! Drug treatment should be strictly coordinated with your doctor!
Treatment of hyperventilation syndrome
Therapy for hyperventilation syndrome should take an integrated approach and combine both pharmacotherapy and non-drug methods. It is important for the attending doctor to conduct explanatory conversations about the reasons for the occurrence of violations. It is necessary to show the patient the connection between the emotional component and somatic symptoms, to convince the patient of the absence of organic pathology. Treatment consists of several areas:
- Psychotherapy. When psychogenicity is detected in childhood, psychoanalysis sessions are required. Psychoanalytic and cognitive-behavioral techniques are also effective.
- Formation of correct breathing. Regular breathing exercises have a positive effect on the course of the disease. Auxiliary methods include courses on relaxation and relaxation techniques. It is necessary to teach the patient the technique of breathing into a bag to relieve a hyperventilation crisis.
- Biofeedback therapy. Special equipment allows not only to obtain objective information about the respiratory system, but also to teach the patient how to breathe correctly.
- Drug treatment of mental spheres.
- Elimination of electrolyte disturbances. Taking magnesium and calcium with the drug can not only reduce the tendency to tetany, but also have an anticonvulsant, calming effect.
Complex treatment is carried out over 4-6 months. Regular monitoring of the patient is recommended to prevent relapses.
Drug treatment of hyperventilation
After all the research has been carried out and hyperventilation syndrome has actually been identified, the doctor prescribes the necessary medications.
First of all, sedatives are prescribed, such as:
| A drug | Photo | Price |
| Glycine | from 23 rub. | |
| Valerian | from 36 rub. | |
| Motherwort | from 20 rub. |
In serious cases, they resort to antidepressants (Prozac, Paxil), however, it is necessary to carefully monitor the patient’s condition, since side effects can override the positive effect.
Often, tranquilizers (Phenazepam, Buspirone) are also prescribed along with them in the treatment of hyperventilation in order to minimize side effects.
| Drugs | Photo | Price |
| Prozac | specify | |
| Paxil | from 726 rub. | |
| Phenazepam | specify | |
| Buspirone | specify |
No less important in therapy are drugs intended to eliminate metabolic abnormalities:
| Drugs | Photo | Price |
| Solcoseryl | from 322 rub. | |
| Asparkam | from 7 rub. | |
| Mildronate | Mildronate | from 291 rub. |
| Mexiprim | from 167 rub. |
To reduce neuromuscular excitability, medications containing magnesium and calcium are used:
| A drug | Photo | Price |
| Calcium D3 Nycomed | from 333 rub. | |
| Vitrum magician | from 789 rub. |
Also, in the treatment of pulmonary hyperventilation, analgesics such as Voltaren and Spazmalgon, and calcium channel blockers (Cardil) can be used.
| A drug | Photo | Price |
| Voltaren | from 284 rub. | |
| Spasmalgon | from 129 rub. | |
| Cardil | specify |
An excellent addition to drug treatment would be physiotherapeutic procedures to help relax: swimming pool, massage, aromatherapy.
Medicines
For the purpose of drug correction of mental areas, the use of antidepressants with a pronounced anxiolytic effect ( Amitriptyline , Fluvoxamine ) is indicated.
Also, patients with hyperventilation syndrome are prescribed antipsychotics, tranquilizers and sedatives. During a crisis, taking benzodiazepine drugs ( Diazepam ) is indicated. When the vegetative component is strongly expressed, vegetotropic medications are prescribed.
Prognosis and prevention
Hyperventilation syndrome does not threaten the patient’s life, but significantly reduces its quality. In the absence of timely and competent treatment, the symptoms worsen and a vicious circle occurs. In the future, the influence of trigger factors may resume and provoke a relapse.
To prevent hyperventilation syndrome, it is necessary to promptly correct emerging psychological problems, learn to adequately respond to stressful situations and form an optimistic, friendly outlook on life.
List of sources
- N.V. Daragan, S.Yu. Chikina “Hyperventilation syndrome in the practice of a pulmonologist: pathogenesis, clinical picture, diagnosis”, article in the journal “Pulmonology” No. 5, 2011
- Kovalenko T.G. “Hyperventilation syndrome. A new look at the problem", Electronic collection of scientific works "Health and education in the 21st century" No. 7, 2011
- Shchekotov V.V., Barlamov P.N., Urban P.I. “Hyperventilation as a risk factor for endothelial dysfunction in patients with hypertension,” Medical Almanac No. 3, 2011
What happens with hyperventilation syndrome
With hyperventilation syndrome, the lungs become overfilled with oxygen as a result of breathing too quickly and deeply. Most often, breathing quickens during great nervous experiences. In a state of strong excitement, a person begins to breathe more often and deeper, since the body needs oxygen to fight stress.
Hyperventilation syndrome
At a certain point, the blood becomes oversaturated with oxygen, and the percentage of carbon dioxide decreases, causing an imbalance. The respiratory center of the brain receives information about the disorder and gives a signal to slow down breathing. The person perceives this as a sign of suffocation and strives to breathe even deeper, while panic intensifies.
As a result, it turns out that a person harms himself. The blood vessels narrow, blood flow to the brain decreases. Attacks of breathing problems alternate with panicked deep breaths. Hyperventilation gets worse and worse. Oxygen starvation occurs, which threatens with very serious consequences.
One of the body's defense reactions to hyperventilation is fainting. At this time, normalization of breathing and blood chemistry occurs due to the body’s self-regulation. After the condition stabilizes, the person comes to his senses.
If such a protective mechanism does not work for some reason, the nervous system becomes overexcited and breathing increases even more. This can lead to irreversible changes in tissues, sclerosis in blood vessels and organs, and can lead to stroke, heart attack, or even death.