Alzheimer's disease is a pathology with neurodegenerative disorders in the brain. As the disease progresses, patients' intellectual abilities deteriorate, memory is impaired, and self-care skills are lost. Naturally, patients and their families are primarily interested in the question: is there a cure for Alzheimer's disease? However, modern science cannot yet give a positive answer. Alzheimer's disease is treated with drugs that can only slow down the pathological process, but do not eliminate it completely. New drugs are constantly being developed to treat Alzheimer's, but they cannot yet completely eliminate the disease. The Yusupov Hospital uses the most modern methods of treating Alzheimer's disease, which normalize the patient's condition and improve his quality of life.
Symptoms of Alzheimer's disease
The disease most often occurs in old age. But its development can begin from 40 to 60 years. In most cases, I diagnose it when the signs of pathology have already become obvious, which significantly complicates the treatment of the disease and worsens the prognosis. This is due to the fact that the first signs of pathology are ignored, and in the meantime the disease progresses. The sooner medications for Alzheimer's disease are started, the greater the chance of maintaining the patient's mental clarity for a long time.
The first sign of developing Alzheimer's disease is memory loss. Typically, short-term memory suffers when the patient cannot remember recent events. At the same time, the events of bygone days are remembered very well.
Another sign of the disease is periodically inappropriate behavior of the patient. This can manifest itself as unreasonable aggression, increased irritability, and inappropriate fun. Human activity decreases and interest in the world around us disappears. A person has difficulty perceiving information, and speech impairment occurs.
As the disease progresses, the severity of clinical manifestations increases. It is recommended to start taking Alzheimer's medicine at an early stage to slow down neurodegenerative processes. Drugs for the treatment of Alzheimer's help stop the development of pathologies and improve the patient's condition.
Alzheimer's disease (AD) is one of the most common and severe diseases of late life. Although this disease has been known for more than 100 years, real steps towards studying its neurobiological basis and searching for methods of therapy began to be actively taken in the world only in the last quarter of the last century. Today, in economically developed countries, research in the field of asthma has become one of the priority areas in the development of medical science and healthcare.
In 2012, according to the Alzheimer's Association in the USA, 5.4 million patients with AD were recorded; this figure is expected to approach 16 million by 2050 [1]. An epidemiological population study conducted by employees of the Department for the Study of Alzheimer's Disease of the National Center for Clinical Prevention of the Russian Academy of Medical Sciences showed that 4.5% of the Moscow population aged 60 years and older suffer from AD [2].
In accordance with diagnostic guidelines developed by international expert groups, including NINCD-ADRDA (National Institute of Neurological and Communicative Diseases and Stroke-Alzheimer's Disease and Related Disorders Association) [3], and the International Classification of Diseases, 10th revision ( ICD-10) lifetime diagnosis of asthma is based on the following mandatory features:
1. Presence of dementia syndrome.
2. Development of multiple deficits in cognitive functions, which is determined by a combination of memory disorders with deterioration in memorizing new and/or reproduction of previously learned information and the presence of signs of at least one of the following cognitive impairments:
• aphasia (impaired speech function);
• apraxia (impaired ability to perform motor activity, despite intact motor functions);
• agnosia (inability to recognize or identify objects, despite intact sensory perception);
• violations of intellectual activity itself, i.e. planning and programming activities, abstraction, establishing cause-and-effect relationships, etc.
3. Impairments of both memory and cognitive functions must be expressed to such an extent that the patient’s social or professional adaptation is reduced.
4. The course is characterized by a gradual, subtle onset and steady progression of impairment of cognitive functions.
5. There are no data from clinical or special paraclinical studies that could indicate that memory and cognitive disorders are caused by any other disease or damage to the central nervous system (for example, cerebrovascular disease, Parkinson's or Pick's disease, Huntington's chorea, subdural hematoma, hydrocephalus, etc.), a systemic disease that is known to cause dementia syndrome (for example, hypothyroidism, vitamin B12 or folic acid deficiency, hypercalcemia, neurosyphilis, HIV infection, severe organ failure, etc.), or state of intoxication (including medication).
6. Signs of the listed cognitive impairments should be detected outside of states of stupefaction.
7. Anamnestic information and clinical study data exclude a connection between the detected cognitive dysfunctions and any other mental illness (for example, depression, schizophrenia, mental retardation, etc.).
The modern classification of asthma is based on age. In accordance with ICD-10, two forms are distinguished: early-onset AD, i.e. before 65 years of age (synonyms: type 2 AD, presenile dementia of the Alzheimer's type); AD with late onset, i.e. after 65 years (synonyms: type 1 AD, senile dementia of the Alzheimer’s type). In addition, a distinction is made between atypical asthma and mixed type dementia, i.e. a combination of manifestations characteristic of asthma and vascular dementia.
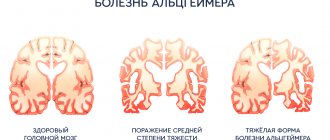
The course of the disease is traditionally divided into three main stages: mild, moderate and severe dementia. At the stage of “mild” dementia, memory impairments (especially for current events become obvious to others, patients have difficulties in chronological as well as geographic orientation. There are obvious difficulties in mental operations, especially in abstract thinking, the ability to generalize, judge, and compare. Patients can no longer independently carry out financial transactions, conduct correspondence, or travel, although they still retain the ability to self-care and relatively independent living.With presenile AD, impairments of higher cortical functions (speech, praxis, optical-spatial activity) already at the stage of “mild” dementia reach clear severity. Senile asthma, in contrast to the presenile type of the disease, debuts exclusively with amnestic disorders. The latter are most often combined with personality changes such as the so-called transindividual (senile) restructuring of the personality structure or the psychopathic type in the form of sharpening the patient’s characterological characteristics.
At the stage of moderately severe dementia, manifestations of amnestic syndrome predominate in combination with disorders of higher cortical functions characteristic of damage to the temporo-parietal parts of the brain, i.e. symptoms of dysmnesia, dysphasia, dyspraxia and dysgnosis. At this stage, pronounced memory disorders are observed, concerning both the possibility of acquiring new knowledge and remembering current events, and reproducing past knowledge and experience; orientation in time, and often in the environment, is grossly disrupted. Patients can no longer independently cope with any professional or social responsibilities. They only have access to simple routine housework, their interests are extremely limited, and they need constant support and assistance - even with self-care. Patients with the senile type of asthma are characterized by amnestic disorientation with the phenomenon of “shifting the situation into the past,” i.e., with a pathological revival of memories of the distant past and false recognition of others, whom patients mistake for people from their past. At the stage of severe dementia, the condition of patients (regardless of the type of disease) is characterized by total dementia with profound memory decay, complete fixation amnesia and amnestic disorientation close to total. The severity of the collapse of intellectual functions is such that patients almost completely lose the ability to make judgments and inferences, verbal communication, and lose psychomotor skills. They are not capable of independent existence and require constant care and supervision. Neurological symptoms reach their greatest severity. But in senile asthma, even at the initial stage, there are no severe neurological disorders (grasping and oral automatisms, amyostatic syndromes or hyperkinesis) characteristic of the final stage of presenile asthma. In patients with severe senile dementia, the final stage usually develops following the addition of some somatic pathology, most often pneumonia: against this background, cachexia, severe degenerative disorders, and fetal position quickly develop.
In the last decade, attempts have been made to purposefully influence both the already known links in the pathogenesis of the neurodegenerative process underlying AD, and the consequences of those dysfunctions that arise at the cellular and molecular levels during its development. This led to the development of the main directions of pathogenetic therapy for AD. The most well developed of them are compensatory (replacement) therapy aimed at overcoming neurotransmitter deficits in various neuronal systems that suffer to a greater or lesser extent in AD.
The main directions in the development of pharmacological methods for the treatment of AD are associated with attempts to correct cholinergic deficiency. Deficiency of the neurotransmitter acetylcholine (ACh) underlies cognitive failure and the subsequent formation of total dementia. The severity of cholinergic disorders correlates with the degree of dementia. Currently, acetylcholinesterase inhibitors (AChEIs) are mainly used to overcome cholinergic insufficiency. Representatives of the new generation of AChE inhibitors are rivastigmine, donepezil and galantamine. The therapeutic effects of these drugs, as well as the safety of their use in AD patients at the stage of mild and moderate dementia, have been convincingly demonstrated in numerous domestic and foreign clinical studies. One can note the dose-dependence of their action, as well as the greatest effectiveness for patients with relatively more intact higher mental functions. The recommended minimum duration of treatment is 6 months.
Rivastigmine is a centrally selective, pseudoreversible (slowly reversible) carbamate-type cholinesterase inhibitor with dual action. Rivastigmine inhibits both AChE and butyrylcholinesterase (BuChE) and has affinity for the cells of the hippocampus and cerebral cortex, i.e., those areas of the brain that are most involved in the pathological process in AD.
Already in the first clinical studies of rivastigmine, its positive effects and good tolerability were noted. In a large multicenter study that included 696 patients with mild and moderate asthma and lasted 26 weeks, significant positive dose-dependent effects of the drug (6–12 mg/day) on cognitive functions and general functioning were established [4]. A study by G. Grossberg et al. [5] showed that the effect of rivastigmine on cognitive function remained clinically significant for at least two years of continuous drug use. Analysis of pooled data (for a group of 2010 patients) showed significantly less deterioration in cognitive function in patients treated for 2 years with rivastigmine compared with patients receiving placebo. The differences at the end of the study were 4–5 points on the ADAS-cog scale. (Alzheimer's disease assessment scale). Similar data were obtained for the Global Clinical Rating Scale.
When using rivastigmine, there was an improvement in the performance of such daily activities as shopping for groceries and cooking, taking medications on time, using the telephone, household appliances, maintaining previous hobbies, etc. [6, 7]. In addition, SG Potkin et al. [8] were able to show that rivastigmine can improve the daily functioning of patients at any stage of the disease, but the greatest effect in this regard is observed at its moderate stage.
Donepezil, a piperidine derivative, is a highly specific, reversible inhibitor of central AChE. The drug has high bioavailability (100%). The effectiveness of donepezil was also confirmed in a multicenter, double-blind, placebo-controlled study of more than 900 patients with mild to moderate asthma, conducted over 24 weeks [9]. The use of the drug significantly improved the cognitive functions of patients. During treatment, the condition of the majority (80%) of patients receiving donepezil improved or remained at baseline. A similar therapeutic effect occurred in only 30% of patients in the control group receiving placebo.
A dosage of 10 mg/day of the drug has been shown to be more effective than 5 mg/day. The researchers noted that the drug's beneficial effects compared to placebo persisted for 6 weeks after completion of donepezil.
K. Rockwood et al. [10], who performed a multicenter, 52-week open-label study of patients with mild-to-moderate asthma, were able to identify targets for therapeutic intervention during donepezil treatment depending on the assessment made by the physician or caregiver. According to the clinician's assessment, the therapeutic targets of donepezil include cognitive function (85% of all patients), patient functionality (68%), behavioral disorders (57%), social interaction (52%) and leisure (20%). Caregivers rated functional activity (86%), cognition (83%), leisure (76%), behavior (57%), and social interaction (49%) as therapeutic targets.
A study of the effectiveness and safety of donepezil in the treatment of asthma was also carried out in Russia [11]. Based on the data obtained, the authors concluded that donepezil is a safe and effective treatment for AD at the stage of mild and moderate dementia. The clinical effectiveness of a 3-month course of treatment with donepezil was established using the MMSE (Mini-Mental State Examination) and ADAS-cog. cognitive scales, as well as based on the general clinical impression of the effect of therapy by the caregiver. The data obtained are in good agreement with international experience in the use of donepezil for the treatment of patients with asthma.
Galantamine is a cholinomimetic drug with a dual mechanism of action unique to AChE inhibitors. It enhances the effects of ACh not only through reversible inhibition of AChE, but also through modulation of nicotinic acetylcholine receptors [12].
In randomized studies performed to date, the effectiveness and safety of long-term (6 months) course therapy with galantamine was studied in cohorts of AD patients with mild and moderate dementia. These studies were carried out in Europe, Canada, Australia and South Africa, as well as in the USA [13, 14–16]. In all of the studies mentioned, galantamine showed a significant benefit in improving cognitive function on the ADAS-cog scale. compared to placebo. After 6 months of treatment with galantamine, cognitive function improved by 3–4 points compared with the placebo group [13]. In addition, significant differences were established between the effects of galantamine and placebo in maintaining the daily functioning of patients at baseline throughout the entire treatment period [17]. It is important that the therapeutic effect of galantamine was accompanied by a significant reduction in the burden on caregivers. The average daily time spent on such care decreased by 15–38 minutes over the 6-month study period, although it increased to 23 minutes in the placebo group [18].
The clinical efficacy and safety of the use of galantamine in asthma at the stage of mild and moderately severe dementia was also studied in Russia in the framework of an open clinical trial conducted in the department for the study of asthma and associated disorders of the National Center for Clinical Prevention of the Russian Academy of Medical Sciences [19]. The results of the study indicate a clear therapeutic effect of a 4-month course of therapy with galantamine at a dose of 16–24 mg/day in patients with mild/moderate severity of dementia caused by AD, which is confirmed in the general clinical assessment of its effectiveness: a positive effect of therapy was established for 88. 2% of patients, including marked improvement in 47% of cases. The therapeutic effectiveness of galantamine was confirmed by a significant improvement in the cognitive and daily functioning of patients, and these significant therapeutic effects were achieved by the end of the 2nd month of therapy and did not depend on the initial severity of dementia.
Of particular interest are studies of the effect of AChE inhibitors on behavioral and psychotic disorders in patients with AD, since behavioral and psychotic disorders that accompany the development of dementia at different stages of its formation occur in more than 80% of patients with AD [20]. The following groups of behavioral and psychopathological disorders occurring in AD are distinguished: psychotic (delusional, hallucinatory and hallucinatory-delusional), depressive symptoms, as well as behavioral disorders themselves (aggression, wandering, motor restlessness, violent screams, inappropriate sexual behavior, etc.). ).
The use of replacement therapy by AD patients has a positive effect on the severity of behavioral and psychotic symptoms of dementia and significantly reduces the need to use psychotropic drugs to correct these conditions, and in some cases allows one to completely stop taking psychotropic drugs.
The results of numerous previous studies of AChE inhibitors, in particular galantamine, indicate that the use of these drugs at the stage of mild/moderate dementia not only reduces the severity of cognitive impairment and functional deficits in daily activities, but also appears to be significantly effective in relation to a number of behavioral and psychotic symptoms, such as anxiety, apathy, disinhibition, which is confirmed by a significant reduction in the overall score of the Neuropsychiatric Inventory (NPI - Neuropsychiatris Inventory), which assesses the severity of various behavioral and psychopathological symptoms of dementia, as well as a decrease in the burden on caregivers [21, 22].
A 24-week open-label study assessed the effect of donepezil on behavioral and psychiatric symptoms of dementia in hospitalized patients with AD [23]. The reason for their hospitalization was the presence of delusions, hallucinations, apathy or aggressive behavior. By the end of the course of therapy, a significant improvement was found in the following indicators of the NPI scale: delirium, irritability and disinhibition.
In a study of the effectiveness of another AChE inhibitor, rivastigmine, in patients with asthma in a nursing home, the severity of behavioral and psychotic symptoms decreased in 58% of patients [24]. Similar results were found in two 26-week studies of rivastigmine. In the first, improvement in behavioral functions was noted in more than 53% of patients on all points of the NPI scale [25]. In the second study, the average NPI score significantly decreased by 3.25 points [26]. According to researchers, the use of rivastigmine not only reduces behavioral disorders in patients, but also allows them to stabilize cognitive functions even in people with advanced dementia.
A comparative study of the clinical effectiveness of cholinergic therapy (on the models of rivastigmine and ipidocrine) for the treatment of psychotic and behavioral disorders in patients with asthma was carried out in the department of the Scientific Center for the Study of AD and associated disorders [27]. The results of the study showed that the addition of AChE inhibitors, especially rivastigmine, to the standard treatment of patients with AD and psychotic disorders has a more favorable effect on the dynamics of behavioral and psychotic symptoms of dementia. When antipsychotic therapy is combined with AChE inhibitors, along with behavioral correction, the cognitive functions of patients with AD improve. This therapeutic effect is greatest in patients treated with rivastigmine. The use of antipsychotic therapy alone, on the contrary, negatively affects the cognitive functions of patients with AD and thereby leads to the progression of dementia, and also reduces behavioral and psychotic symptoms in these patients to a lesser extent (compared to combined therapy).
In recent decades, the biological prerequisites for another direction of pathogenetic therapy of AD, glutamatergic pharmacotherapy, have been successfully developed. Thanks to advances in molecular biology, the understanding of the functioning of the glutamatergic system in the central nervous system (CNS) has expanded significantly. It has been established that glutamate as a neurotransmitter plays a significant role in many physiological functions of the central nervous system. It was found that in AD, the content of glutamate receptors in the hippocampal region is significantly reduced, and the degree of reduction correlates with the severity of dementia. The neurotoxic properties of glutamate (the phenomenon of excitotoxicity) have been proven. The main drug in the glutamatergic strategy for treating AD is memantine. The mentioned drug combines the properties of a low-affinity non-competitive antagonist of NMDA (N-methyl-D-aspartate) receptors and an agonist of AMPA (amino-3-hydroxy-5-methylisoxazole-4-propionate) glutamate receptors. The drug was found to be well tolerated and without serious side effects. It is advisable to carry out a 6-month course of treatment, and for moderate-severe and severe dementia, a longer (1 year or more) use of the drug.
J. Ricke and A. Glazer [29] analyzed the assessment by general practitioners of the results of using memantine in outpatient settings (1420 patients with dementia). The general physician assessment of effectiveness as “good” or “very good” was given by 70% of patients. Moreover, the improvement achieved after a 3-month course of therapy in various assessment parameters (memory, concentration, sleep, mood, motor skills) was maintained over a long period (more than a year) of observation.
A study of the effectiveness and safety of the drug memantine in the treatment of AD at the stage of moderate and severe dementia was carried out in the department of the National Center for the Study of AD and associated disorders of the Russian Academy of Medical Sciences [30, 31]. An undoubted positive effect of memantine at a dose of 20 mg/day on memory and other intellectual functions, as well as on the correction of motor and emotional disorders, was established. In addition, an increase in the level of spontaneous activity, an improvement in concentration and an increase in the pace of activity, as well as a decrease in the severity of a number of behavioral and psychotic symptoms of dementia (agitation and aggression, irritability and mood instability, aberrant motor behavior) were noted.
Our data are confirmed by the results of a study performed by S. Gautheir et al. [32], which analyzed the effect of memantine on behavioral disorders using databases from two clinical studies. The analysis showed that with monotherapy with memantine, as well as with combination therapy with memantine and donepezil, patients with asthma showed a positive effect in relation to not only cognitive disorders, but also behavioral disorders, with the most pronounced effect noted in relation to agitation/aggression. The effect of memantine on agitation/aggression was either a reduction in symptoms at the start of treatment or a delay in the onset of these symptoms in patients without pre-treatment symptoms. This effect of memantine is unique compared with other classes of drugs used in the treatment of behavioral symptoms associated with dementia and justifies the increasing use of this drug as monotherapy or in combination with cholinesterase inhibitors.
Main drugs for Alzheimer's disease
To date, a cure for Alzheimer's disease that actually works and can completely cure a person has not yet been invented. All developed medications only help to slow down the course of the pathology, but are not able to eliminate it.
To treat Alzheimer's disease, drugs called cholinesterase inhibitors are used. This is an enzyme necessary for the breakdown of choline. Increasing the level of acetylcholine slows down the development of pathology and the formation of amyloid protein, which is one of the causes of the development of the disease. A representative of this drug for Alzheimer's is Exelon. It is available in the form of tablets, a solution for internal administration and a patch with the active substance applied. The latter form is very convenient, since in this case the person receives the required dose of the medicine automatically. While patients usually forget to take pills.
Aricept based on donepezil hydrochloride can be used to treat any form of dementia in Alzheimer's disease. It helps eliminate the clinical manifestations of pathology and slows down degenerative processes. Available in the form of tablets and solutions.
Glutamate NMDA blockers are also used in the treatment of dementia. The representative is the drug “Akatinol Memantine”. It slows down the atrophy of the gray matter of the brain.
FDA approves new drug for Alzheimer's disease
Garcia-Marin et al. / Front Neuroanat, 2009
The US Food and Drug Administration (FDA) has approved Biogen's Alzheimer's disease aducanumab. The previous drug for this disease that received FDA approval came to market 18 years ago. The new drug targets amyloid plaques in the brain, but how well it treats the disease is still unclear. Developers will have to prove that aducanumab actually improves cognitive function in patients - otherwise the FDA may withdraw its approval.
Until recently, there were five drugs in the world to treat Alzheimer's disease. Four of them are approved in the US and around the world, but do not actually cure patients - because they do not fight the cause of the disease, but only mitigate the manifestation of some symptoms.
The fifth medicine was approved in 2021 in China - we talked about this in detail in the text “The Fifth Odd One”. It was created on the basis of an algae extract: the developers expected that the components of the plant cell wall would feed the “right” bacteria in the human intestine, and they, in turn, would suppress inflammation in the nervous tissue. However, many questions immediately arose about this medicine - and so far it has not received worldwide recognition.
At the same time, the American company Biogen was developing its own drug, aducanumab. These are monoclonal antibodies that are designed to attack and destroy beta-amyloid aggregates, one of the main signs of Alzheimer's disease. So far, none of the therapies targeting beta-amyloid had worked in clinical trials, and many scientists suspected that amyloid was not a cause but a side effect of the disease. In March 2021, Biogen also suffered a setback: it stopped its clinical trials, explaining that the drug did not demonstrate the desired effect - amyloid plaques in the brain became smaller, but aducanumab did not always affect cognitive abilities.
However, already in the fall of 2019, Biogen announced that it had revised the data and came to new conclusions. According to the drug's developers, the samples of subjects turned out to be heterogeneous: one of the arms of the trial probably included more people in whom the disease developed faster than average. If they were excluded from the analysis, the drug appeared to be effective. With this wording, Biogen submitted documents for review to the FDA.
The department’s expert commission looked into the situation for about a year, and in the fall of 2020 it issued a verdict (we discussed it in detail in the text “In the World of Complex Decisions”): data from different branches of the trial can be considered independently of each other. This sounded like a recommendation to approve the drug, as long as failure in one of the branches did not diminish the success in the other. A panel of outside experts then reviewed the FDA experts' report and came up with a contrary verdict: it did not recommend approval of the drug, with ten votes against to one in favor.
And six months later, the FDA published its decision: the drug (it was named Aduhelm) was approved, but provisionally. In its statement, the agency clarifies that such a procedure is used when “there is an expectation of clinical benefit, despite doubts that remain about this benefit.” The FDA expects that since amyloid plaques in the brains of patients have become smaller in all arms of the trial, the drug can still be expected to work against external signs of the disease.
However, the developers will have to conduct a fourth, post-registration phase of trials and confirm that aducanumab actually improves cognitive function in patients. If this cannot be proven, the FDA reserves the right to revoke its approval.
Previously, we talked about a mutation that protected a Columbia resident from a hereditary form of Alzheimer's disease. In addition, researchers tried to treat this disease using ionizing radiation - and received the first positive results.
Polina Loseva
Second-line drugs for the treatment of Alzheimer's disease
The most effective drugs for Alzheimer's disease are cholinesterase inhibitors. However, treatment of the pathology should be comprehensive with the elimination of clinical manifestations.
What medications treat Alzheimer's disease:
- Glycine can be used to improve cerebral circulation and normalize the emotional background;
- To eliminate hallucinations and the appearance of obsessions, antipsychotics and tranquilizers can be used;
- Treatment of anxiety, panic attacks, and depression is carried out with the help of antidepressants.
All drugs for the treatment of Alzheimer's disease must be prescribed by the attending neurologist. Each of the drugs has its own contraindications and side effects, so using them independently can negatively affect your health.
In addition to drug treatment, the patient is prescribed other types of therapy:
- Physiotherapy;
- Aqua aerobics;
- Art therapy;
- Special classes to improve cognitive functions.
Alzheimer's disease: lines of therapy
ALZ 25.09.2020/5
In 2018, the German publication InTouch made a sensational statement: the heir to the English throne, Prince Charles, will never become king because he has been diagnosed with Alzheimer's disease (AD). The information was allegedly confirmed by insiders: according to them, Charles constantly forgets what happened five minutes ago and has poor orientation.
Well, the prospect of receiving a royal crown is not a panacea for the onset of AD, or any other incurable disease. The possibilities of neuroprotective therapy for Alzheimer's disease remain very limited today [1]. The only way modern medicine can help patients (and today, according to WHO estimates, there are at least 25 million of them in the world [2]) is pharmacotherapy and rehabilitation. Effective treatment of mild (mild) and moderate dementia is very important, since it is at this stage that the highest rate of progression of cognitive impairment, psychotic and antisocial disorders is observed.
The “gold standard” for the treatment of asthma, according to the consensus of the FDA, the opinion of EU regulators, as well as the approval of the Ministry of Health of the Russian Federation, is stepwise therapy. Its first stage is the use of cholinesterase inhibitors [3,4] that optimize synaptic transmission, for example, donepezil ( Alzepil ®).
Algorithm for pathogenetic therapy of asthma* [5]Mild dementia Goal: maintaining the patient’s cognitive and daily functioning, preventing progression. Drugs (level of evidence 1++, A): donepezil and other AChE inhibitors. Efficacy criteria: stabilization of cognitive disorders and impairments.. Moderate dementia Goal: Stabilization of cognitive functions and self-care capabilities. Drugs (level of evidence 1++, A): donepezil and other AChE inhibitors, akatinol, memantine. Efficacy criteria: improved functioning at home, slowed progression of dementia. Moderate-severe and severe dementia Goal: maintaining the ability to perform minimal self-care, facilitating care. Drugs (level of evidence 1+ and 1++, A): combination of donepezil + memantine or memantine in monotherapy. Efficacy criteria: stabilization of condition, maintenance of hygiene skills. *Antidepressants and antipsychotics are used for symptomatic purposes in the development of depression or behavioral disorders in asthma. |
Alzepil ® promotes activation of the cholinergic system, the “central player” in memory and learning ability. The drug has high bioavailability. Patients with impaired renal function do not need to change the treatment regimen, because this condition does not affect the clearance of donepezil. Due to the possible increase in exposure in mild to moderate liver dysfunction, dose increases should be based on individual tolerance. [5]
Titration scheme [6]
- Initial dose 5 mg/day (orally, before bedtime), at least 1 month
- If well tolerated, increase to 10 mg/day (1++, A)
One recent meta-analysis of 30 studies (8257 participants) confirmed that donepezil 10 mg/day for 6 months resulted in better preservation of cognitive function compared with placebo with minimal adverse events [7].
Literature
- Neurology. National leadership. Brief edition / ed. E. I. Guseva, A. N. Konovalova, A. B. Gekht. - M.: GEOTAR-Media, 2021. - 688 p.
- World Health Organization [WHO]. (2017). Dementia. Fact Sheet. Available at: https://www.who.int/mediacentre/factsheets/fs362/en/ (accessed 1 February 2018).
- O'Brien JT, Holmes C, Jones M, Jones R, Livingston G, McKeith I, Mittler P, Passmore P, Ritchie C, Robinson L, Sampon EL, Taylor JP, Thomas A, Burns A. Clinical practice with anti-dementia drugs: a revised (third) consensus statement from the British Association for Psychopharmacology. J Psychopharmacol. 2017;31(2):147–168.
- Wong CW. Pharmacotherapy for dementia: a practical approach to the use of cholinesterase inhibitors and memantine. Drugs Aging. 2016;33(7):451–460.
- Instructions for medical use of the drug Alzepil, tablets, LP-000228 dated 01/23/2020
- Diagnosis and treatment of Alzheimer's disease. Clinical recommendations. Russian Society of Psychiatrists. Moscow, 2014.
- Jacqueline S Birks and Richard J Harvey. Donepezil for dementia due to Alzheimer's disease. Cochrane Database Syst Rev. 2021 Jun; 2018(6): CD001190.
The material is intended for medical workers.
How to treat Alzheimer's disease: new drugs
New drugs and treatments for Alzheimer's disease are constantly being developed around the world. However, no one can yet say that a cure for Alzheimer's has been found.
An effective cure for Alzheimer's disease, developed in the United States, is currently in testing. The drug CAD 106 helps to increase antibodies to the amyloid protein, without increasing the concentration of T cells.
Another promising drug is MDA7. This immunostimulating agent, which increases the body's resistance to negative agents, stops the progression of degenerative processes in the brain.
Also, drugs that treat Alzheimer's disease may be substances originally invented for the treatment of other pathologies. Thus, Rosiglitazone, which was developed for the treatment of insulin-dependent diabetes mellitus, showed good results in eliminating dementia. The drug is still being tested on animals.
Prevention of Alzheimer's: drugs
Unfortunately, drugs have not yet been developed to prevent Alzheimer's disease, since the exact cause of this pathology cannot be reliably identified.
Prevention includes measures to improve overall health and improve brain function:
- Balanced diet;
- Moderate physical activity;
- Active lifestyle;
- Mental activity;
- No bad habits (smoking, drinking alcohol, drugs);
- No stress.
Treatment of Alzheimer's disease at the Yusupov Hospital
A special department has been created at the Yusupov Hospital for the treatment of neurological pathologies. The hospital's doctors have extensive experience treating various forms of Alzheimer's disease. Prescription of drugs is carried out by a qualified neurologist based on the individual characteristics of the patient.
Patient care is provided by specially trained staff who know the intricacies of caring for patients with Alzheimer's. Psychological support is also provided to patients and their relatives.
The work uses drugs for Alzheimer's, which are approved for use in Russia. Also, a certified research center operates on the basis of the Yusupov Hospital. Therefore, patients have the opportunity to receive the latest treatment, which is not available in other hospitals.