Causes of development and classification of myelitis
Myelitis can be triggered by a variety of reasons and can occur in different scenarios. Most often, the cause of its development is infection. Pathogens include influenza, scarlet fever, typhus, polio, pneumonia, rabies, measles and other infectious diseases. The consequence of such conditions is most often transverse myelitis - inflammation in its most acute form.
The second reason why myelitis begins to develop is intoxication, leading to inflammation. In addition, injuries that affected the spinal cord, incorrect injections of drugs and punctures should be considered as the cause of myelitis.
In addition to the main reasons mentioned above, these may include factors such as hypothermia and various immunosuppressive conditions.
According to etiology, myelitis is classified into five types:
- viral;
- infectious;
- traumatic;
- toxic;
- post-vaccination myelitis.
According to the mechanism of its development, the disease is divided into primary and secondary types. In this case, secondary myelitis is a consequence of other diseases.
Based on the duration of its course, myelitis is differentiated into three main types: acute, subacute and classic. There are several types of this inflammation based on prevalence. This is diffuse, multifocal and localized myelitis. Transverse myelitis in this classification belongs to limited, as it represents a small focus of the disease.
List of used literature and sources
- Gerwig Imhof. Radiation diagnostics. Spine/ Gerwig Imhof – Moscow, “MEDpress-inform”, 2011. – 192-195 p.
- Acute transverse myelitis [Electronic resource] / Michael Rubin, MDCM, Professor of Clinical Neurology, Weill Cornell Medical College; Attending Neurologist and Director, Neuromuscular Service and EMG Laboratory, New York Presbyterian Hospital-Cornell Medical Center. – 2021. – Access mode: https://www.msdmanuals.com/ru-ru/ professional/neurological-diseases/spinal-cord-diseases/acute-transverse-myelitis—Reference to the source: 03.23.2018
- Kruglov O. Transverse myelitis [Electronic resource] / Radiographia: website. – 2021. — Access mode: https://radiographia.info/article/poperechnyy-mielit — Access to the source: 03/23/2018
- Transverse myelitis [Electronic resource] / Radiopaedia: website. – 2005-2018. – Access mode: https://radiopaedia.org/cases – Access to the source: 03.23.2018
Pathogenesis of myelitis
Acute myelitis can occur hematogenously when the blood-brain barrier is disrupted. The damage that the spinal cord undergoes in this type of disease is of lymphogenous origin. Moving along the roots and nerves, the pathology reaches the epidural space. Then it moves along the lymphatic pathways located in the dura mater of the brain and spreads to all subarachnoid spaces. At the same time, damage to the surrounding tissue occurs and, as a result, inflammation spreads to the entire spinal cord.
Toxic myelitis involves a degenerative disorder in tissue. In such cases, specialists often diagnose not myelitis, but myelosis - combined sclerosis associated with a lack of vitamins, in particular vitamin B12. In this case, the posterior and lateral columns of the spinal cord are mainly affected.
Myelitis causes changes in the structure of the spinal cord substance. It becomes flabby, swollen, and pronounced swelling appears on it. The “butterfly” pattern, visible in a cross-section in a healthy state, loses its clear contours. In the area of inflammation, hyperemia, minor hemorrhages, cell death, myelin breakdown, and infiltration of formed elements are observed.
Symptoms of myelitis
Among the signs of this neurological disorder, the first to appear are symptoms characteristic of any inflammation in the body. This is body temperature, often rising to 39-40 degrees or more. At the same time, aching bones, chills, a feeling of fatigue and general malaise, which are common for high temperatures, may occur. In this regard, the first signs of myelitis are often mistaken for typical cold symptoms.
Neurological disorders become noticeable later, when the lesion manifests itself as pain at the site of inflammation. Transverse myelitis causes especially severe pain. Discomfortable sensations spread not only to the back area, but also to the limbs, radiating to the internal organs.
The set of signs of myelitis depends on its stage and place of development. For example, symptoms such as loss of sensitivity, severe numbness and paresis of the legs are observed in cases where the disease affects the lumbar region. These conditions are accompanied by the absence of reflexes and impaired functioning of the internal organs of the small pelvis.
If myelitis is localized in the cervical region, then its main symptom is difficulty breathing, speech impairment, pain during swallowing. General malaise, dizziness and weakness also appear.
Myelitis of the thoracic spine is expressed by stiffness of movements and the presence of pathological reflexes. In this case, disturbances in the functioning of certain organs may occur.
If such symptoms are detected, it is important to immediately seek professional help, since prolonged inactivity aggravates the problem as a result of the rapid development of the disease. The stronger the tissue damage, the more difficult it is to return the spinal cord to its previous state, since its structure may change irreversibly. This threatens the loss of ability to work and the ability to move fully.
Read also
Pelvic pain
Pelvic pain is pain in the muscles that form the pelvic floor and organs located in the small pelvis, caused by microtrauma, chronic deformation of the sacrococcygeal region due to anatomical…
Read more
Herpes zoster
Varicella zoster first enters the human body at an early age and manifests itself as chickenpox, most often in children. Then follows the latent phase of circulation of the pathogen in the body and under certain conditions...
More details
Hepatic encephalopathy
Hepatic encephalopathy is a brain lesion that occurs against the background of liver pathology and is caused by liver failure. There is acute hepatic encephalopathy, which occurs on…
More details
Ankylosing spondylitis/ankylosing spondylitis
Ankylosing spondylitis (ankylosing spondylitis) is a chronic inflammatory disease of the spine and joints, accompanied by progressive pain, stiffness and limited movement at the beginning...
More details
Clubfoot
Clubfoot should not be understood as just one foot disorder. This is a group of deformities of the foot and ankle joint with their pathological setting. Clubfoot is a deformity in which...
More details
Diagnosis of myelitis
If myelitis is suspected, a mandatory procedure is a lumbar puncture to analyze the cerebrospinal fluid. The presence of inflammation is indicated by its traces and the absence of protein. The same study allows us to detect the presence of microorganisms in the fluid, which means that the spine has become infected.
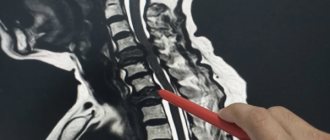
In addition to the puncture, the patient is sent for magnetic resonance imaging or tomography using contrast. As a rule, one of these tests, chosen at the discretion of the doctor, is sufficient. Necessary measures are the use of suboccipital myelography and analysis to identify microorganisms and other pathogens in the cerebrospinal fluid.
Since myelitis can be the result of a large number of processes, it is necessary to carry out a differential diagnosis to accurately exclude diseases such as multiple sclerosis, spinal stroke, cystic arachnoiditis and other pathologies with symptoms that are similar at first glance.
In addition to these conditions, it is necessary to make sure that the patient does not have epiduritis, a disease with an equally similar clinical picture that requires surgical intervention. In difficult situations, additional research may be required when the doctor prescribes an exploratory laminectomy. Diagnosis of epiduritis involves studying the affected tissues for purulent foci, radicular pain and syndrome of increasing compression of the spinal cord substance, which distinguishes this disease from myelitis.
It is necessary to differentiate myelitis from acute Guillain-Barré polyradiculoneuritis, which differs from it in the absence of conduction disorders, disorders of the pelvis and spastic phenomena.
Spinal cord tumors that need to be excluded during diagnosis have their own characteristic differences: a slow course, a clearly defined stage of radicular pain, a block in liquorodynamic tests, protein-cellular dissociations in the cerebrospinal fluid.
Excluding hematomyelia and hematorahis, you need to know whether elevated body temperature is present among the symptoms, since it is its absence, combined with a sudden onset and rapid development, that is a sign of these diseases. Hematomyelia causes damage to the gray matter, and when there is hemorrhage under its membranes, the patient experiences meningeal symptoms. Such pathologies often develop as a result of injuries.
Acute transverse lesion requires the exclusion of cerebrospinal circulatory disorders and multiple sclerosis, although the latter is always accompanied by such signs as damage to the white matter in certain areas, diffuse damage not only to the spinal cord, but also to the brain, and a decrease in the intensity of symptoms after a few days.
Myelitis also needs to be differentiated from chronic meningomyelitis, which is characterized by slow progression at normal temperatures. Meningomyelitis is caused by syphilis, detected using serological tests.
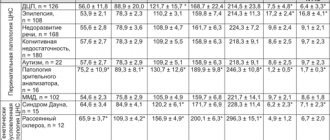
CSF examination
According to the literature, primary diseases of the central nervous system rarely lead to changes in a general blood test and biochemical analysis of serum, and if they exist, this indicates the likelihood of systemic disorders and secondary diseases of the central nervous system (Willard M. D., Tvedten H., Turnald GH, 1999). Therefore, in our practice, we perform a cerebrospinal fluid analysis even in the absence of abnormalities in blood tests before performing myelography.
In the cerebrospinal fluid sample, the physicochemical properties (color, transparency, protein content, glucose) are determined, and the cellular elements in the Goryaev chamber (erythrocytes and nuclear cells) are counted. Next, the cytogram in the stained preparation must be analyzed (May-Grunwald staining) to determine the content of each type of cell.
Normally, cerebrospinal fluid is transparent and colorless, the albumin content is 0.1–0.3 g/l, the number of cells does not exceed 5 cells per μl. The cytogram is scanty; single erythrocytes and mononuclear cells can be detected. The liquor is sterile.
With meningitis, turbidity of the cerebrospinal fluid is observed, accompanied by pleocytosis (increased content of cellular elements). In our studies, during acute inflammatory processes of the central nervous system, the protein concentration in the cerebrospinal fluid exceeded 100 mg% (1 g/l), cytosis - from 25 to several thousand nuclear cells per μl. Neutrophilic leukocytes predominate in the cytogram; microflora (usually coccal) is often detected. When the inflammatory process subsides, the number of cellular elements is often quite normal, the protein content may be normal or slightly increased, but, as a rule, does not exceed 3 g/l. In this case, the cytogram is represented by neutrophils, lymphocytes, and macrophages. In meningitis of viral etiology, the cerebrospinal fluid is usually clear, the protein content is slightly increased (up to 100 mg%), cytosis is 10–500 cells per μl, and mainly lymphocytes/mononuclear cells are present.
It should be noted that the cerebrospinal fluid is in direct contact with the membranes of the brain, therefore it more reflects the intensity of the inflammatory process of the membranes. In this regard, with deep disorders of the spinal cord parenchyma and the absence of damage to the membranes, analysis of the cerebrospinal fluid may not reveal significant abnormalities.
Rice. 1. Liqueur for purulent myelitis. Rice. 2. Swelling of the spinal cord in a Staffordshire Terrier due to myelitis. Block of liquor pathways in area C2. The cause of myelitis was chronic bacteremia, which in turn could be caused by impaired liver function. This dog was diagnosed with liver cirrhosis. After treatment for 3 years, no signs of spinal cord damage were observed.
Rice. 3. Repeated (in a week) myelography of the Staffordshire Terrier after the course of treatment. At the time of myelography, clinical manifestations of improvement were not observed. Recovery of spinal cord function occurred within 1.5 months.
Treatment of myelitis
Treatment of myelitis depends on how much the spinal cord is affected and which segment of it is affected by inflammation. Acute myelitis is the most complex and severe form of the disease, in which the patient requires urgent surgical intervention. The operation eliminates pressure on the vertebrae and spinal canal, leading to pain. The high temperature that accompanies myelitis is relieved by a course of antibiotics and relief from inflammation.
Any myelitis requires urgent treatment, otherwise motor function may be lost forever. The course of myelitis therapy carried out with already bedridden patients includes measures to combat bedsores: treating the skin with camphor oil, regularly changing bed linen, placing rubber rings. If bedsores do appear, the damaged tissue is excised and a bandage is applied with Vishnevsky, penicillin or tetracycline ointment. Prevention of new bedsores is carried out using ultraviolet irradiation of the buttocks, sacrum and feet.
Along with bedsores, patients may experience dysfunction of the pelvic organs. The cause of these failures is an ascending urogenital infection that accompanies myelitis, which also needs monitoring and appropriate treatment. Initially, anticholinesterase drugs are used to remove urine. If they are ineffective, catheterization and rinsing of the bladder with antiseptic solutions is necessary.
To return the patient to full movement, the doctor prescribes dibazole, prozerin and vitamin B. Taking these medications is most often combined with passive gymnastics and therapeutic massage.
Myelitis in any form is an inflammatory disease that requires maximum doses of broad-spectrum antibiotics. To reduce the intensity of pain, antipyretics are used simultaneously with ACLT 40 units twice a day for 2-3 weeks and glucocorticoid hormones 50-100 mg per day. The latter can be replaced with dexamethasone or triamcinolone.
Prevention and prognosis of myelitis
There is no specific prevention in this case. Considering that myelitis is a consequence of other diseases, injuries and various types of interventions, it is advisable to consider prevention of diseases that will cause it as prevention in this situation. These include infectious diseases: polio, mumps, measles and the like. Experts recommend vaccination as one of the means to combat them. Preventive measures include timely treatment of other infectious diseases when their first symptoms appear.
The prognosis depends on how severely the patient's spinal cord is affected. With timely and adequate treatment, improvement occurs within six months, and full recovery occurs after 1-2 years. If no positive dynamics are observed by this time, we should talk about disability.
The area of localization also plays a significant role. Thus, upper cervical myelitis can be a direct cause of death. Thoracic and lumbar myelitis without timely diagnosis and proper treatment leads to loss of motor function of the lower extremities. The prognosis is significantly worse if myelitis is accompanied by other pathologies: cystitis, pyelonephritis, pneumonia and frequent extensive bedsores.
Causes
The main cause of transverse myelitis is infections from other areas of inflammation entering the spinal cord. There are many factors that cause the disease. These are influenza viruses, herpes, syphilis, cytomegalovirus infection, HIV. Borreliosis and meningitis lead to inflammation of the spinal cord. Such pathologies cause infectious myelitis.
Based on other reasons, the following types of disease are distinguished:
- Intoxicating. The main development factors are alcohol, poisons, salts of heavy metals, and some medications.
- Traumatic. When the spine is damaged, pathogenic bacteria penetrate the spinal cord through the wound. On the other hand, direct nerve damage plays a role.
- Compression. It occurs due to compression of the spinal cord structures by hematomas, tumors, cysts, and intervertebral hernia.
- Post-vaccination. The disease appears after the vaccine is administered to people with hypersensitivity.
- Ray. Develops during radiation aimed at treating tumors.
- Hereditary. Pathology accompanies hereditary diseases. These are adrenoleukodystrophies, Friedreich's disease.
- Idiopathic. The general name for inflammation of the spinal cord, the exact causes of which are unknown. Suspected to be autoimmune. Under the influence of certain factors, the body begins to synthesize antibodies against proteins contained in the myelin sheath of neurons. There is an assumption that in some cases, idiopathic myelitis arose as a consequence of a viral disease that did not manifest itself.
Pathology often accompanies multiple sclerosis.