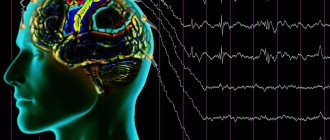
The main methods for diagnosing epilepsy are magnetic resonance imaging and electroencephalogram. The article will talk about EEG of the brain: what it is, decoding in children.
An encephalogram is a method for studying the bioelectrical activity of the brain. This study allows us to determine the activity of neurons in various parts of the brain, the presence of pathological patterns (discharges) that indicate pathology. The harmlessness of the diagnosis allows it to be widely used in childhood. Based on the results of the study, epileptiform activity, indications for MRI and the direction of further treatment are determined.
Epileptiform activity on the EEG in a child - what does it mean? The term epileptiform activity refers to electrical oscillations recorded on the EEG in the form of sharp waves and peaks that differ from the general activity by more than 50%. The presence of epileptiform activity on the EEG may indicate the presence of epilepsy.
Indications for research in children
A study is prescribed to diagnose various neurological and psychiatric diseases of children. Such diseases include:
- Delayed speech development: differential diagnosis between dysarthria (disturbance in the speech apparatus) and pathology of the speech centers of the brain.
- Different types of epilepsy, from generalized to myoclonus in individual muscle groups.
- Tics: to exclude the central genesis of the disease and disturbances in the electrical activity of the brain.
- Autism, child behavior disorders (aggression, etc.), attention deficit hyperactivity disorder.
- Enuresis or bedwetting.
- Sleep disorders, including somnambulism (sleepwalking - sleepwalking): it is necessary to conduct an EEG during night sleep.
- Brain injuries (concussions, bruises, etc.) - to identify foci of abnormal bioelectrical activity.
- If a child's brain is suspected of having cancer, the lesion will show pathological signals, although it may not yet be visualized on MRI.
- Frequent headaches for which no explanation has been found.
- Cognitive disorders: poor memory, poor school performance, attention deficit, excessive absent-mindedness, and so on.
Symptoms of cortical dysarthria in children
Characteristic symptoms of cortical dysarthria are disturbances in the tempo-rhythmic component of speech: there is a slow pace of expressive speech, lack of fluency and automatism. From the outside it seems that it is difficult for the child to move his tongue and lips.
The most difficult sounds are the anterior lingual sounds. The baby replaces or skips problematic sounds. Because of this, speech is blurred and slurred. But there are no problems with the semantic part, that is, the vocabulary is sufficient, children correctly use words in sentences and correctly express their thoughts.
Cortical-subcortical dysarthria is characterized by violent involuntary movements at rest and during conversation.
Afferent cortical dysarthria
Signs of this variant of cortical dysarthria are the search for the correct articulatory structure when pronouncing sounds, which causes pauses. The voice, due to stress during conversation, is loud with a decrease in voiced consonants. Due to the slowness of speech, intercalary sounds appear.
The baby pronounces affricates (consonants made of two sounds) separately or pronounces only a separate part. For example, “t” or “s” or the prolonged “ts” from instead of the sound “ts”. It also replaces some sounds with others: fricative consonants with stop consonants. The child cannot name the place on the face that the speech therapist touches.
Efferent cortical dysarthria
Cortical kinetic dysarthria is characterized by slowness of speech due to problematic transitions between sounds. Stressed vowels are lengthened, and consonants, if they are at the beginning and end of a word, too. The pronunciation of “l”, “sh”, “r”, “zh” suffers: this requires the participation of the tongue, and the child’s tongue movements are difficult. He can replace them with “d” or “t”.
It is difficult for a child to fix the desired articulatory position, so there are unnecessary insertions and omissions of sounds. Children may wrinkle their forehead, stick out their tongue, close their eyes, and lick their lips when talking.
How is the research conducted?
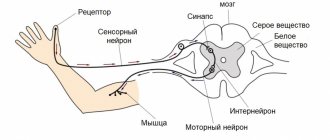
Electrodes are installed on the scalp in the projection of different parts of the brain; there are usually 19 of them in total; they are attached symmetrically on both sides of the head and in the center; a “cap” can be immediately put on, without the need to attach each electrode separately. An ECG sensor is also attached to the chest area; additional sensors (myographic) are often needed. At the same time, the child leads a normal lifestyle: walks, eats, plays sedentary games (mosaics, dolls, etc.), and smart technology records the activity of the baby’s brain.
The day before, the mother needs to prepare the child for the examination:
- Wash your hair, as excess sebum disrupts the tight contact of the electrode with the scalp and distorts the examination result.
- Remove jewelry (earrings, hair clips, piercings).
- If the child is very small or shows aggression or is too restless, then it is recommended to premedicate, which includes sedatives.
- Sometimes sleep deprivation is recommended, which is carried out in order to increase the information content of the study.
- It is not recommended to feed your child energy foods on the eve of the test: chocolate, strong tea, coffee, energy drinks, and so on.
- Warn the functional diagnostics doctor about all medications that the child receives in detailed dosages and frequency of use.
Complications in children
Speech defects affect the development of speech in general, the state of the nervous system and cognitive functions. Children do not develop their vocabulary well, and they have a general underdevelopment of speech. Attention and memory deteriorate. A pronunciation defect causes a deterioration in the perception of phonemes. Such violations are fraught with learning problems: written speech and reading suffer.
At older ages, the likelihood of psychological problems is high. School-age children have a hard time with speech disorders, become withdrawn, and may show aggression and irritability. Depression may develop. The situation becomes more complicated if there is a lack of understanding and help from parents.
How is it deciphered and what can you see?
Deciphering brain EEG readings in children takes quite a lot of time. Results are usually provided within a few days. Since electrical indicators from all leads are analyzed, all peaks and waves, their synchrony, and symmetry are assessed.
Parents are given a conclusion, a printout of the fragments of the recording selected by the doctor, and, in specialized centers, a disk with a recording of the entire study. Sometimes your doctor can make recommendations for further testing.
It will not be possible to independently understand how to decipher the EEG of the brain in children, even with a very strong desire. Only a specialist can decipher waves of electrical activity, especially in children, for whom even the norm has many variations, depending on the age of the child.
It is customary to distinguish the following main rhythms of electrical activity on the EEG:
- Alpha rhythm (or precursor of alpha rhythm in children under 5 years old). It is recorded in a state of rest, in which the child sits or lies with his eyes closed and does nothing.
- Beta rhythm. It is detected with maximum concentration of attention: fast waves indicate active wakefulness.
- Theta rhythm. With a normal picture, the EEG in healthy children 2-8 years old is one of the main rhythms; it consists of waves whose amplitude is slightly higher than the alpha rhythm. The appearance of such indicators in adulthood may indicate a delay in mental development; genetic consultation may be required.
Also, when deciphering EEG in children, the synchrony of electrical potentials in both hemispheres is assessed. Disturbance in synchronization indicates the presence of a pathological focus. It can be represented by a tumor, an epileptic focus, a vascular malformation, and so on.
Recording epileptiform patterns is an important part of the study. Benign epileptiform patterns of childhood are now considered as a variant of the norm in the absence of epileptic seizures and regression in the child’s development.
If multiple discharges appear on the EEG, it is necessary to evaluate the clinic; it may be necessary to consult the baby with a psychologist and psychiatrist. It is necessary to decipher such results and make a diagnosis taking into account additional research methods.
EEG of the brain in children
The procedure is somewhat troublesome when you have to examine a small child.
It is impossible to prevent small children from moving, so parents are given instructions on how to hold the child and distract his attention with the help of toys. Of course, when recording EEG in children, one has to put up with inevitable interference (artifacts). Performing functional tests is also difficult. Hyperventilation is only performed in children who are able to follow instructions.
An encephalogram in children under 3 years of age is sometimes recorded only during the sleep stage. Older guys may not sleep. The main thing is that the child should be calm during the procedure, so it is advisable to occupy him with a book or toy. Electroencephalography of brain structures helps determine the level of mental, speech, mental and physical development of children, and the risk of epilepsy.
Should you trust the research?
An encephalogram is a functional research method, so often the results largely depend on the condition of the child at the time of the examination. If, for example, a doctor sees dysrhythmia and the presence of a large number of theta waves when deciphering the EEG of the brain in a child over 8 years old, you should not immediately try to make a diagnosis. Perhaps the baby simply reacted negatively to the study, because children are quite emotional.
Of course, if serious deviations are detected, with the formation of foci of abnormal activity, indicating the presence of an epileptic focus, further examination is required. The electrical method will only indicate the approximate location of the lesion (lobe of the brain). It is possible to most accurately determine the localization of the process and the possible cause (vascular, neoplastic, atrophy due to intrauterine oxygen deprivation of the brain, etc.) only by using neuroimaging methods, primarily MRI.
Treatment of cortical dysarthria in children
Correction of cortical dysarthria begins with pathogenetic treatment of the disease that led to a speech defect. Without this step, no amount of speech therapy help will help restore speech.
Complex treatment includes:
- drug therapy aimed at stimulating metabolism in the brain and restoring its functions. Prescribe nootropic drugs, vitamins, metabolites. In difficult cases, sedatives, tranquilizers, and antidepressants may be needed;
- speech therapy correction of cortical dysarthria - speech therapy massage, articulation gymnastics, development of fine motor skills of the hands, production of sounds. If necessary, a psychologist is involved in the treatment process;
- physiotherapeutic procedures, reflexology, massage, physical therapy help eliminate muscle paresis and improve blood flow throughout the body;
- Relaxation techniques - art therapy, aromatherapy, music therapy help relieve stress and improve the emotional background.
Conventional treatment is long-term. Specialists prescribe several courses of therapy, during which they can adjust the program taking into account the body’s response to therapeutic measures.
How often should the study be repeated?
If the diagnosis did not show significant changes in brain electrical activity, then the study may not be repeated in the absence of new symptoms.
When epileptiform activity is detected, the encephalogram will become the main objective diagnostic criterion for the effectiveness of the prescribed therapy.
The study should be repeated at least every year, preferably once every 6 months. Assessing the dynamics will allow you to adjust therapy to prevent recurrent attacks (increasing or decreasing doses of antiepileptic drugs).
Even after the diagnosis of epilepsy is removed, it is necessary to repeat the encephalogram for another 1-5 years (depending on the diagnosis) to prevent a possible relapse. After surgery, annual examination is also recommended for several years. This will avoid many complications.
How to prepare for an EEG
On the eve of the study, it is recommended to wash (and, of course, dry) your hair.
Do not use hair styling products, undo your braids, remove jewelry and hair clips from your head.
In some cases, the attending physician may ask you to limit sleep on the eve of the test, most often this is necessary so that the patient can fall asleep during the EEG. By limiting sleep we mean a significant reduction in its duration - by several hours (at least 3-4 hours).
It is usually not recommended to administer sedatives before the study, as they change the EEG pattern.
If a child is going to undergo an EEG, then it is better for him to present this procedure as an exciting game. You need to describe to him in advance what will happen, clarify that it is not painful or scary, and even interesting.
It is worth taking it with you on a towel so that after the examination you can clear your head of traces of the electrode gel. Young children may require feeding during recording.
The duration of the study may vary in different laboratories depending on the patient’s diagnosis, his condition, the presence of epileptic seizures during the study, etc. It is often possible to obtain the necessary information in about half an hour, but the doctor or laboratory technician can increase or decrease the recording time if necessary.
Long-term (usually many hours) recording of electroencephalography is called
EEG monitoring. There is no exact timing for this test; it is decided by the attending physician and EEG laboratory personnel depending on the specific situation.
When simultaneously recording the patient's behavior on a video camera, the study will be called EEG video monitoring (or video EEG monitoring). EEG monitoring is prescribed if necessary:
- see the patient’s troubling conditions and clarify their nature
- record a long-term EEG if a short standard recording does not reveal specific changes
- evaluate the EEG pattern during wakefulness and sleep.