Intervertebral hernia is a common pathology associated with the musculoskeletal system. With this disease, protrusion or prolapse of fragments of intervertebral discs into the spinal cavity occurs. The danger of this condition lies in its practically asymptomatic occurrence at an early stage of development. However, if treatment is not started and care is not taken, the disease begins to progress rapidly. You can make an appointment for treatment of a cervical hernia at ArthroMedCenter.
Where does neck pain come from?
The occurrence of painful manifestations in the neck area is most often noted against the background of:
- pathological changes in the spinal column - osteochondrosis, osteoarthrosis, scoliosis, neuralgia, intervertebral hernia;
- injuries associated with vertebrae, discs, joints, ligaments and muscle tissue;
- immune diseases of the ridge;
- infections of the musculoskeletal system;
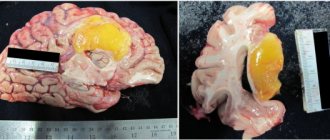
- neoplasms of benign and malignant nature;
- intracranial hemorrhages, tumors and abscesses;
- physical activity, overwork during training, lifting heavy objects.
Causes of lumbago in the neck
Most often, doctors define cervicago as a consequence of progressive osteochondrosis. This disease has a destructive effect on bone tissue, resulting in compression of the nerve roots. This is what leads to severe muscle spasms and acute pain.
There may be other causes of lumbago in the neck on the right or left side:
- formation and growth of intervertebral disc herniation;
- injuries of the spinal column (especially in its upper parts);
- neoplasms of a malignant and benign nature, located in the sternum, neck and collar area of the back;
- any inflammatory processes occurring in the upper parts of the spine.
Types and causes of discogenic pathology in the cervical spine
Any problems with the integrity of the intervertebral disc with the contents moving beyond its boundaries is considered a disease. Protrusion and hernia form against the background of a critical increase in mechanical pressure on a certain area of the disc. As a result, the nucleus pulposus, located inside, protrudes. The nucleus puts pressure on the annulus fibrosus tissue, which can lead to its rupture.
Doctors distinguish the following stages of the disease:
- A slight protrusion of the disc without damage to the fibrous ring with a displacement of a maximum of 2-3 mm. The clinical picture is mild.
- Development of disc protrusion, which is accompanied by more pronounced protrusion of the pulp up to 3-5 mm. The patient begins to complain of periodic pain. Most often, the ability to work at this stage of the disease is preserved.
- The formation of the hernia itself, which is also called prolapse or extrusion. At this stage, the fibrous ring in the intervertebral disc ruptures with the pulp falling out beyond the boundaries of the disc tissue, for example, into the spinal canal. This is due to the localization of the damaged area.
- At the last stage of pathology formation, the prolapsed fragment of the nucleus pulposus is separated from the disc tissues with possible displacement under pressure. The separated element can move along the spinal canal. This leads to damage to the nervous structure and serious complications in the form of compression of the spinal canal. This condition is called sequestration.
Naturally, as the pathology progresses, each of the listed stages is not always observed. Sequestration develops quite rarely, although the mechanism of formation of the pathology is the same. In any case, the producing factor is increased pressure, leading to the destruction of the discs. This is most often associated with injuries, falling in slippery weather and hitting the head.
The most common cause of herniated intervertebral discs in the cervical spine is an accidental blow to the head in a low doorway. Healthy discs will not erode immediately. This will require prolonged exposure to negative factors or a sharp increase in pressure, for example, when hitting your head. This can cause a severe “explosive” fracture of the spinal elements in the neck, damage to the spinal canal, leading to disability of the patient.
Cervical radiculitis (“pinched nerve”)
Radiculitis at the level of the cervical spine most often occurs when the roots of the spinal nerves are compressed.
This usually occurs due to cervical spondylosis or a herniated disc, where the outer portion of the disc (the annulus fibrosus) ruptures and the nucleus pulposus of the disc protrudes into the spinal canal. Sometimes cervical sciatica occurs due to infections (herpes virus infection, Lyme disease).
How does it manifest itself? Often there is pain in the neck, radiating to the arm. Moreover, the hand may become numb or weaken. Typically, the diagnosis of cervical radiculitis can be made after a neurological examination. However, in some cases it may be necessary to perform a computed tomography or electromyography scan.
Risk factors for exacerbation
The formation of an exacerbation during protrusion and hernia in the cervical spine is most often observed against the background of:
- Poor posture, stooping, flat feet or walking in uncomfortable shoes. The spinal column has a powerful compensating mechanism that protects the brain from shock during walking and running. However, any uncompensated shock is transmitted upward with amplification. The occurrence of the greatest amplitude and traumatic potential is observed at a considerable distance from the place where the vibration is localized. As a consequence, poor posture, dehydration in the intervertebral discs with possible destruction form in the cervical region.
- Tonic tension in the deep muscles of the dorsal and cervical region, which is accompanied by muscle spasm with the formation of a protective posture. Due to the increased load on the head and neck muscles caused by wearing high hairstyles in women and heavy winter fur hats, blood circulation in the muscle tissue of the cervical region is impaired. As a result, the nutrition of the intervertebral discs deteriorates and their tissues become dehydrated.
- Over time, osteochondrosis develops and progresses, and osteophytes appear on the elements of the spine. This causes poor blood circulation and the development of muscle spasms with limited motor function in the neck.
As a result, a rapid increase in pressure on the spinal tissue leads to its transmission to the intervertebral disc. Against the background of uneven, eccentric and undistributed pressure, a destructive process in the disc begins. This provokes the formation of a protrusion or a hernia itself.
General characteristics of pain syndrome
A pinched neck is a pathological condition in which turning and tilting the head is accompanied by severe pain. The sensations can persist for a long time, aggravated by referred pain in the back, shoulders and arms. The nature of the pain is often asymmetrical, intensely expressed only on one side. The pain increases with palpation or turning the head.
A characteristic behavior when pinched is the rotation of the head along with the body.
Pain in the cervical spine (cervicalgia) is a signal of a negative process affecting the body from the inside or outside. Pain syndrome develops in response to a number of irritants, including:
- physiological factors;
- some inflammatory and degenerative diseases.
Unpleasant sensations can be nociceptive and neuropathic in nature. The type of pain is determined by the provoking factors.
Symptoms of exacerbation of hernia
Uncomplicated cervical hernias are often accompanied by the following symptoms:
- Shooting pain in the upper extremities, similar to an electric shock, increasing with coughing, moving the arms and sneezing, sometimes radiating to the elbow, wrist or fingers. This is due to the infringement of certain nerve endings, their swelling and inflammation.
- Impaired sensitivity in the form of numbness or hypoesthesia, formication or a sensation as if goosebumps are crawling. Such symptoms often appear at a significant distance from the intervertebral disc, for example, in the area of the fingers of the upper extremities.
- Constant aching pain in the cervical region associated with a muscle reaction. This phenomenon is called secondary myofascial syndrome. The pain syndrome sometimes radiates to the back of the head and manifests itself in the form of cephalgic syndrome - persistent pain in the head.
- Secondary symptoms of a hernia in the form of progressive weakness and muscle hypertrophy in the arms and shoulder girdle on the side where the damage is localized. Peripheral or flaccid paralysis (paresis) may develop.
Due to the close proximity of a large neurovascular network, as well as the autonomic nervous structure, the formation of so-called neurovascular symptoms is possible.
Causes of neck pain when moving the head
Pain in the cervical spine when turning the head can occur under the influence of various factors. Let's look at the most common ones:
- Hypertonicity of the neck muscles. Most often it occurs due to overexertion during sports. When lifting heavy objects, bending and turning the head, microtraumas to muscle fibers can occur in the neck or collar area. This leads to pain that gets worse every time you turn your head. This phenomenon affects not only athletes, but also everyone whose work involves constant overstrain of the neck and arms.
- Lack of load. Static loads are no less harmful to the neck than overexertion. Pain and the inability to turn the neck can develop if a person leads a sedentary lifestyle and spends a long time in an uncomfortable or static position: at the computer, while driving, while sleeping.
- Traumatic injuries. The cervical spine is the most fragile compared to others. Therefore, an excessively sudden movement, impact or fall can lead to injury to this area. It can be:
- injuries to the muscles and ligaments of the neck (sprain, rupture);
- injuries of intervertebral joints;
- cervical vertebrae injuries.
- Diseases. Most often, osteochondrosis, a degenerative change in the intervertebral discs, leads to pain in the cervical spine when turning the head. It is accompanied by a number of symptoms: deterioration of hearing and vision, headache, numbness of the limbs, chronic fatigue, crunching pain in the joints of the neck. Among the diseases of the cervical spine that cause pain when turning the head, one can also list: intervertebral hernia, scoliosis, osteoarthritis, spondylosis, thyroid disease.
Possible complications
Long-term progression of cervical intervertebral hernia can cause the appearance of radicular symptoms, which are accompanied by sensory and motor disorders. It can also cause compression of the spinal canal. As a consequence, compression myelopathy and sometimes tissue necrosis in the spinal cord may develop. This may lead to disability for the patient.
There is information that the development of such a pathology in some cases contributes to compression of the vertebral arterial vessel on the right or left side. This is an auxiliary source in which ischemic stroke can form, especially at a young age.
Often, protrusion and hernia in the acute stage due to sudden movements of the head and neck lead to a significant narrowing of the walls of the vertebral arterial vessel. As a result, an ischemic focus develops in the brain area. The likelihood of the formation of such a condition increases significantly if the patient has a congenital anatomical feature in the structure of the circle of Willis. This is accompanied by its openness and absence of posterior communicating arteries.
With a closed circle of Willis, increased blood flow can be quickly redistributed from the posterior vertebrobasilar bed to the anterior (carotid) or in the opposite direction.
In cases where the posterior communicating arteries are completely absent or are underdeveloped, it will not be possible to quickly redistribute blood flow. This often ends with the transformation of the ischemic focus into a necrotic area, and as a result, the development of a stroke is noted.
Measures for myositis
Myositis is an inflammation of the muscles of the cervical spine, which is accompanied by shooting pain. Pinching due to muscle inflammation prevents you from turning your head, and in some cases makes it difficult to swallow. Severe inflammatory processes are accompanied by high body temperature and tissue swelling. Pathology appears when there is a draft in transport or under air conditioning, as well as as a result of infectious diseases of the upper respiratory tract, traumatic exposure or toxic intoxication. Self-treatment of muscle pinching of inflammatory etiology is aimed at:
- relief of the main symptoms;
- restoration of normal muscle condition.
The medications and methods of home treatment are completely identical to the treatment of physiological pain in the cervical region. In addition to pharmacological agents, exercise therapy and self-massage are used for recovery at home.
Tablets for hyperthermia
With myositis, hyperthermia often occurs, in which the use of combined medications is justified. Adult patients can take Next or Panoxen tablets, which are combined antipyretic and anti-inflammatory drugs. For treating a child, Ibuklin is better suited, as it quickly relieves fever and is suitable for young children.
Diagnostics
The doctor conducts a visual examination of the patient to identify problems with posture and lack of sensitivity in the area where the nerve is pinched. By palpating the spine, the doctor will identify the level of spasm and soreness in the muscles and the location of the disease. The patient may be required to bend and stand to assess for limited mobility. Next, the reflexes of the knee and Achilles tendons are assessed.
To accurately determine the size and location of an intervertebral hernia in the cervical spine, the doctor prescribes a CT, MRI and radiographic examination in 2 projections.
Therapy methods
Typically, patients diagnosed with cervical intervertebral hernia suffer from the pathology for more than one year, and exacerbations and remissions are regularly observed. Often, painful sensations weaken over time or disappear on their own a couple of weeks after a subsequent exacerbation.
Conservative methods of therapy will not help to completely get rid of the problem; it helps to cope with the consequences of the hernia’s impact on the soft tissue, muscles and nerve endings. Often, as a residual phenomenon, the presence of a vegetative reflex effect on the tone of vascular tissue - neurovascular symptoms - is observed.
Complex therapy involves taking the following pharmaceuticals:
- non-steroidal anti-inflammatory drugs (COX-2 inhibitors);
- muscle relaxants with central action;
- As auxiliary methods, medicinal electrophoresis using vitamins and aminophylline is prescribed.
When the exacerbation subsides, the use of physiotherapeutic procedures is indicated. To activate blood circulation in muscle tissue, it is recommended to perform physical therapy and massage of the cervical-collar region (movements must be extremely careful).
Treatment of cervical intervertebral hernia with relatively crude methods, such as manual therapy, traction, can cause a significant aggravation of the condition. This will lead to the development of serious negative consequences.
As an emergency measure, it is recommended to wear a Shants collar if pain occurs. The device is used to support the head and helps prevent sudden bending and turning of the head, which can lead to the development of compression symptoms and sometimes fainting.
After the collar is applied, it is better to immediately consult a neurologist and have an MRI of the neck performed; then you may need to consult with a neurosurgeon. This will help to assess the possible risk for a similar location of the pathology and determine the choice of treatment regimen.
MBST therapy
This modern technique is used for joint pathologies to restore cartilage tissue and discs. The treatment mechanism is based on high-pulse magnetic resonance at the cellular level.
The procedure promotes:
- increasing the volume of cartilage tissue due to cell restoration;
- increased cartilage density due to increased collagen levels;
- relieving pain.
You can treat a hernia of the cervical spine in Moscow at ArthroMedCenter. MBST therapy will help eliminate pain and spasm, as well as the underlying causes of the disease.
Prevention
To prevent the formation of a cervical hernia in patients at risk, you should adhere to these simple rules:
- Avoid forced, uncomfortable head positions.
- If possible, do neck exercises frequently, especially if your job involves spending a lot of time at the computer.
- Walk and sit straight, do not slouch.
- For rest, use a hard mattress and a small, medium-firm pillow.
- Do not overload the spinal region, regardless of which area the load falls on.
A cervical hernia is a rather dangerous disease; it is difficult to treat. You can count on a positive result using only conservative treatment methods only if the patient promptly seeks help from a specialist. In addition, it should be taken into account that for a cervical hernia larger than 6 mm, surgical intervention is required.
Neck pain when turning
Why does my neck hurt?
Pain in the neck when turning the head appears as a result of various pathological processes. Most often it can be provoked by:
- Osteochondrosis
. Degenerative changes that occur in the spine are caused by prolonged stay in one position (working at a computer in an office, at a cash register in a store, or as a driver), especially against the background of reduced physical activity. Due to the thinning of the discs of the intervertebral column, the nerve endings and small blood vessels are compressed - pain occurs. - Muscle inflammation
. With myositis, the muscles swell, lose their elasticity and ability to stretch, resulting in pain, which most often makes itself felt when changing position or after hypothermia. If the scalene muscle is affected, the pain is sharp and piercing. To prevent it, the patient tries to limit the motor activity of the affected area as much as possible. - Vascular atherosclerosis
. The formation of an atherosclerotic plaque leads to disruption of the lumen of the vessel, resulting in pain. - Cancerous tumors and benign neoplasms
. Discomfort and unpleasant sensations in the neck develop gradually and, as a rule, during movements. In this case, the tumor can be located anywhere. - Injury or inflammation of the spinal cord or brain
.
Also, pain in the neck when turning the head may occur if the patient has autoimmune pathologies. This primarily includes systemic lupus erythematosus, ankylosing spondylitis and some other diseases in which the spinal ligaments lose their elasticity and the intervertebral discs decrease in volume, provoking various types of neuralgia.
Clinical picture
Pain syndrome, depending on the causes, can occur suddenly, under the influence of certain factors (lower temperature, movement, etc.) or be present constantly, either fading or exacerbating again.
Along with this, the clinical picture is often supplemented by symptoms such as:
- dizziness;
- headache;
- tinnitus, hearing loss;
- darkening of the eyes;
- nausea and vomiting;
- lack of coordination.
The patient's condition may be aggravated by impaired consciousness, signs of arterial hypertension, fever and general malaise comparable to ARVI.
Diagnostics
If you experience neck pain when turning your head, you should seek help from a qualified professional. The doctor already understands a lot from the conversation. But nevertheless, to make an accurate diagnosis, instrumental studies are mandatory - radiography, magnetic resonance imaging or computed tomography. It is also necessary to donate blood (clinical analysis and biochemistry).
Treatment
Treatment is carried out within the framework of a holistic approach, which involves restoring postural balance, and not targeting only one of the body systems. Manual therapy methods are offered to correct postural disorders. Our medical center offers acupuncture and acupressure treatments. Physiotherapy and exercise therapy can help achieve good results. Therapy is selected individually based on the results of the examination.