Poliomyelitis is a highly contagious viral disease that causes paralysis of the arms, legs, and breathing, and can also cause death. Poliomyelitis pathogens penetrate the oral mucosa mainly through contaminated water. Infection by airborne droplets is also possible.
Poor hygiene conditions favor transmission. The incubation period ranges from 3 to 35 days. After a person gets sick, he develops lifelong immunity (protection against infection) to one viral type (but there are polioviruses types 1, 2 and 3). Only vaccination completely protects against infections of all three types. You can get vaccinated against polio at the RebenOK clinic at the best prices in Moscow.
Why is polio dangerous?
Most infections (>95%) are asymptomatic, but antibodies are produced. If there are signs of illness, there are different pictures of the disease:
· Abortive polio: inflammation of the gastrointestinal tract (gastroenteritis), fever, nausea, sore throat, muscle pain and headaches without central nervous system involvement.
· Non-paralytic poliomyelitis (aseptic meningitis): inflammation of the meninges without paralysis.
· Paralytic polio (1 in 200 infections) with typical symptoms of paralysis: independent breathing may become impossible and lifelong use of mechanical ventilation may be required. Paralysis can also lead to death.
Even decades after infection, post-poliotic syndrome may occur. There is no cure for polio. Only symptomatic therapy is prescribed to eliminate discomfort.
Types of vaccines
Various vaccines are available, which are administered by a doctor using a syringe in several single doses. Polio vaccination for infants is often combined with other vaccines. The combination vaccine is distributed over four single doses: the first is given to infants at the age of 3 months, the last - in the second year of life.
Types of polio vaccines:
· Vaccination with OPV (oral polio vaccine).
It comes in the form of drops and contains weakened forms of two types of viruses. Passive immunity is produced in the intestines.
· Vaccination IPV (inactivated vaccine).
It has the form of a homogeneous suspension, available in disposable 0.5 ml syringes. It contains three types of “dead” viruses.
OPV is cheaper. The drug is produced in Russia and has good reviews. Inactivated polio vaccine is an imported product. The drugs have certain differences and have their own side effects and positive aspects.
The RebenOK clinic uses several drugs. Names of the polio vaccine:
· "Pentaxim". Designed for children from three months of age. The national vaccination schedule involves three injections with an interval of one and a half months and further revaccination after a year. The second revaccination (fifth administration of the drug) is carried out with OPV or IPV.
· "Bivouac Polio". Live polio vaccine, which consists of three doses of a weakened oral vaccine and two doses of an inactivated vaccine. It is carried out in the first year of life. Booster vaccination against polio is carried out one year after receiving the first dose.
· "Infarix Hexa". A combined drug that does not have strict preparation requirements. The vaccine is effective against polio, tetanus, diphtheria, whooping cough, Haemophilus influenzae, and hepatitis B.
· "Polimilex". A single drug that is widely used for the prevention of polio. Injected subcutaneously or intramuscularly. The drug is “dead”, so it cannot cause the development of the disease.
The choice of drug remains with the doctor. Many experts prefer to use combination vaccines. If a child has contraindications, then single medications are prescribed.
Vaccination against polio
Specific prevention is vaccination against polio. There are 2 types of polio vaccines:
- Sebin live vaccine (OPV - contains live attenuated viruses)
- inactivated (IPV - contains polioviruses of all three serotypes killed by formaldehyde).
OPV vaccine
OPV vaccination is carried out for children starting from 2 months of age by instilling 2-4 drops (depending on the concentration of the vaccine) onto the lymphoid tissue of the pharynx in infants and onto the surface of the tonsils in older children.
The first vaccination is carried out at 3, 4, 5 and 6 months, then revaccination is required at 18, 20 months and 14 years.
After vaccination with OPV, the child should not be fed or given water for an hour, as the vaccine will be washed into the stomach with food and water. If the child burps, it is necessary to repeat the vaccination (for the same reason).
Before vaccination and immediately after it, new foods cannot be introduced into the child’s diet, as allergic reactions may occur that are mistakenly taken for side effects of the vaccine.
The day before vaccination, you should make sure that you have antipyretic and antiallergic drugs in your home medicine cabinet.
Precautionary measures after OPV vaccination: do not kiss the child on the lips and wash your hands after washing the baby.
Contraindications for OPV vaccination:
- children with congenital immunodeficiency or HIV (also not possible if family members have the same problems);
- the presence of pregnant women around the child;
- pregnancy or planning it;
- breast-feeding;
- unusual reaction to a previous vaccination;
- allergy to neomycin, streptomycin and polymyxin B (included in the vaccine);
- acute infectious diseases (vaccination after recovery).
IPV vaccine
IPV vaccination is carried out
- children (weak, with a pregnant mother and/or intestinal disorders)
- adults (medical workers who have close contact with patients, travel to endemic areas, unvaccinated people).
IPV is administered subcutaneously or intramuscularly:
- children: primary vaccination at 2, then at 4 months, then revaccination at 6-18 months and at 4-6 years;
- adults: first vaccination (0.5 ml), repeat after 4-8 weeks and third dose after 6-12 months.
Side effects of vaccination:
Possible side effects that do not require emergency medical intervention:
- nervousness,
- temperature rise to 38.5°C,
- swelling,
- pain at the injection site,
- nausea, single vomiting or diarrhea.
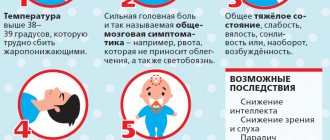
Contact your doctor immediately if:
- adynamic and lethargic child;
- difficulty breathing, shortness of breath;
- temperature above 39C;
- convulsions;
- urticaria, itching;
- drowsiness;
- swelling of the face, eyes;
- difficulty swallowing.
After vaccination with IPV, walking and bathing the child are not prohibited.
Refusal of vaccination
First of all, unvaccinated people are at risk of polio with all the ensuing consequences.
In addition, if they refuse vaccination, they are prohibited from traveling to countries that require vaccination against polio and are temporarily (during the epidemic) not hired in educational and health institutions.
Advantages and disadvantages
Polio vaccination is usually given in infancy as part of basic immunization, along with the other five routine vaccinations. Poliomyelitis is a serious infectious disease, which in its development stage leads to disability if the gray matter of the spinal cord is damaged. Benefits of polio vaccination:
· allows you to avoid infection and prevent disability, skeletal deformities and paralysis;
· the vaccinated person develops immunity from the disease, so even if infected, the child will tolerate the disease much easier;
· Adverse reactions after vaccination are mostly absent.
Many believe that the vaccine has shortcomings that result in the development of the disease polio. But the probability of such an outcome is no more than 1 case in 2.7 million people.
Vaccination is not dangerous to the life and health of the child. The goal is to protect against future infection by creating a barrier against infection. The most harmless is the inactive vaccine.
Adverse reactions
The combination polio vaccine, often used in infants, is generally well tolerated. There may be redness or painful swelling at the injection site. Allergic reactions are also possible.
As the immune system reacts to the vaccine, it may temporarily cause various illnesses. These include, for example:
· headaches and aches;
· gastrointestinal discomfort;
· fever and fatigue;
· irritability and chills.
These vaccination reactions usually resolve on their own within 1-3 days.
Common side effects of the polio vaccine in children
Polio vaccination is, as a rule, quite easily tolerated, without causing negative consequences in children of different ages, however, reactions are possible, and we will talk about them further.
There are two types of vaccinations:
- IPV or inactivated. Contains killed viruses;
- OPV or “live”.
Popular vaccines against infection:
- Poliorix . Contains three types of inactivated viruses. Produced in Belgium. Approved for use in children starting from the age of 2 months. Administered as an injection;
- Imovax polio . Produced in France, the composition is similar to Poliorix. The method of application is identical;
- Oral polio vaccine (Russia) . Contains live polio viruses. Available in the form of a liquid that is dripped into the mouth.
In Europe, exclusively inactivated types of vaccines are used. In Russia, for some time, only IPV vaccinations were also used, but after polio outbreaks recorded in Tajikistan in 2010, the Russian Ministry of Health decided to include OPV vaccines in the National Calendar, which provide more reliable protection.
Poliorix vaccine
Comparative characteristics of vaccinations:
| Side effects/incidence | Poliorix | Imovax polio | Oral polio vaccine |
| General reactions (increase in body temperature) | often | from often to very often | none |
| Local skin manifestations (redness and pain at the injection site) | often | often | none |
| Nervous system (excitability, anxiety, drowsiness) | often | often | none |
| Reaction from the gastrointestinal tract (diarrhea, vomiting, loss of appetite) | often | rarely | none |
| Allergic reactions, including shock, angioedema, bronchospasm | rarely | rarely | rarely |
| Vaccine-associated paralytic polio (VAP) | no risk | no risk | isolated cases (1 in 3 million vaccinated) |
Vaccine Pentaxim
In addition, the polio antigen is found in several other vaccines, such vaccinations include:
- Pentaxim. Multicomponent French vaccine containing antigens to whooping cough, diphtheria, tetanus, as well as polio and hemophilus influenzae;
- Tetrakok;
- Infanrix IPV.
Reactions to them may differ from those listed above due to the presence of a larger number of components.
Is there a fever after vaccination?
Children may develop a fever after receiving the polio vaccine. This reaction is considered normal and indicates that the body has begun to produce antibodies necessary to fight the virus. A slight increase in body temperature is observed in 1-4% of patients. The temperature may rise to 37.5-38.6 degrees. If the readings exceed a moderate level, then you should take an antipyretic drug.
Does the polio vaccine cause side effects that are life-threatening?
Post-vaccination reactions can be life-threatening in case of severe individual intolerance by the body to any components of the immunodrug.
Despite the fact that shock and angioedema, as a generalized allergic reaction to the polio vaccine, occur extremely rarely, this is not excluded.
Since in most cases they occur in the first half hour after administration of the drug, it is worth staying in a medical facility during this period.
What other conditions should promptly consult a doctor: fever above 39 degrees, swelling of the face, hives, shortness of breath or difficulty breathing, prolonged lethargy, problems with swallowing.
How many vaccinations are given against polio?
The Russian national vaccination calendar provides the following polio vaccination schedule:
· in the 1st year of life – at 3,4,5 and 6 months;
· in the 2nd year of life – at 18 and 20 months;
· at the age of 14 – once.
In accordance with the Russian calendar, the first two vaccinations are carried out with IPV, the third – with OPV. The vaccination course involves the use of only inactivated vaccines. When two doses of OPV are administered, it is possible to provide high local protection in the intestine. With continued use of live vaccines, the risk of developing vaccine-associated poliomyelitis is reduced.
Polio vaccinations - contraindications
Preventive polio vaccination is an effective measure to protect the body from infection with a dangerous virus. This procedure is recommended for absolutely everyone, but in some cases immunization is unacceptable.
Polio vaccination contraindications:
- pregnancy (only in case of urgent need and only with the permission of the local obstetrician);
- viral and infectious diseases occurring in the patient’s body;
- You cannot vaccinate during exacerbation of chronic processes;
- individual intolerance to the components included in the vaccine.
It is also not recommended to give the vaccine to children who have had serious side effects from a previous polio vaccine.
A doctor can accurately determine the possibility of safely administering a vaccine against a viral disease after visually examining the patient and studying the results of preliminary tests.
If any adverse reactions are detected after vaccination, you must immediately inform your local doctor or call an ambulance! Such complications are extremely rare. The main reason for adverse effects is incorrect administration of the vaccine, a weakened child’s body, or failure to comply with the interval between vaccinations. To prevent such complications, properly prepare your child for the upcoming polio vaccination.
Tips for parents
If a child often has allergic reactions or is allergic, then vaccination is possible only during the period of remission. There is no need to use any medications before administering the vaccine.
If your child experiences the following symptoms after vaccination, you should consult a doctor:
· appearance of signs of acute respiratory infections (runny nose, cough, etc.);
· dysfunction of the gastrointestinal tract;
· shortness of breath, decreased muscle tone of the limbs.
We are talking about signs of vaccine-associated polio, which may appear 4-30 days after OPV administration. A visit to the pediatrician is necessary if there is an irregular heartbeat, urticaria or severe headaches.
After vaccination, it is recommended to avoid visiting crowded places. The child should be given more purified water to drink, and allergenic foods should be excluded from the diet.
Warning for the unvaccinated
The stated goal of the World Health Organization (WHO) is to eradicate polio, and Russia is also committed to this goal. However, polio is still found in Pakistan, Afghanistan or Nigeria and can also be carried by tourists into the Russian Federation. Therefore, polio vaccination is still recommended, important and necessary.
Everyone should be vaccinated against polio, ideally as early as infancy. People who were not vaccinated as children, or whose vaccination status is unknown, should catch up on polio vaccination.