Oculomotor nerve (n. oculomotorius, III pair of cranial nerves)
Motor neurons of the oculomotor nerves (n. oculomotorius, III pair of cranial nerves) are located on both sides of the midline in the rostral part of the midbrain. These nuclei of the oculomotor nerve innervate the five extrinsic muscles of the eyeball, including the levator palpebral muscle. The nuclei of the oculomotor nerve also contain parasympathetic neurons (Edinger-Westphal nucleus), which are involved in the processes of pupil constriction and accommodation.
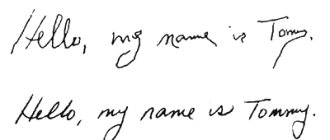
The normal position of the eyeballs and divergent strabismus are shown with weakness of the medial (internal) rectus muscle of the eye on the right (n. oculomotorius, III pair of cranial nerves).
There is a division of supranuclear groups of motor neurons for each individual eye muscle. The fibers of the oculomotor nerve innervating the medial rectus, inferior oblique and inferior rectus muscles of the eye are located on the side of the same name. The subnucleus of the oculomotor nerve for the superior rectus muscle is located on the contralateral side. The levator palpebrae superioris muscle is innervated by the central group of cells of the oculomotor nerve.
Trochlear nerve (n. trochlearis, IV pair of cranial nerves)
The motor neurons of the trochlear nerve (n. trochlearis, IV pair of cranial nerves) are closely adjacent to the main part of the complex of nuclei of the oculomotor nerve. The left nucleus of the trochlear nerve innervates the right superior oblique muscle of the eye, the right nucleus innervates the left superior oblique muscle of the eye.
Abducens nerve (n. abducens, VI pair of cranial nerves)
Motor neurons of the abducens nerve (n. abducens, VI pair of cranial nerves), innervating the lateral (external) rectus muscle of the eye on the side of the same name, are located in the nucleus of the abducens nerve in the caudal part of the pons. All three oculomotor nerves, leaving the brain stem, pass through the cavernous sinus and enter the orbit through the superior orbital fissure.
Clear binocular vision is ensured precisely by the joint activity of individual muscles of the eye (oculomotor muscles). Conjugate movements of the eyeballs are controlled by the supranuclear gaze centers and their connections. Functionally, there are five different supranuclear systems. These systems provide various types of eyeball movements. Among them there are centers that control:
- saccadic (rapid) eye movements
- purposeful eye movements
- convergent eye movements
- holding the gaze in a certain position
- vestibular centers
Weakness of the lateral (external) rectus muscle of the right eye (n. abducens, VI pair of cranial nerves) was shown before and after treatment.
Saccadic (rapid) eye movements
Saccadic (fast) movements of the eyeball occur as a command in the opposite visual field of the cortex of the frontal region of the brain (field 8). The exception is fast (saccadic) movements that occur when the central fovea of the retina is irritated, which originate from the occipital-parietal region of the brain. These frontal and occipital control centers in the brain have projections on both sides in the supranuclear brainstem centers. The activity of these supranuclear brain stem centers of vision is also influenced by the cerebellum and the vestibular nuclei complex. The paracentral sections of the reticular formation of the bridge are the stem center, providing friendly rapid (saccadic) movements of the eyeballs. Simultaneous innervation of the internal (medial) rectus and opposite external (lateral) rectus muscles when moving the eyeballs horizontally is provided by the medial longitudinal fasciculus. This medial longitudinal fasciculus connects the nucleus of the abducens nerve with the subnucleus of the complex of oculomotor nuclei, which are responsible for innervation of the opposite internal (medial) rectus muscle of the eye. To initiate vertical rapid (saccadic) eye movements, bilateral stimulation of the paracentral sections of the pontine reticular formation is required from the cortical structures of the brain. The paracentral sections of the pontine reticular formation transmit signals from the brain stem to the supranuclear centers that control the vertical movements of the eyeballs. This supranuclear eye movement center includes the rostral interstitial nucleus of the medial longitudinal fasciculus, located in the midbrain.
Purposeful eye movements
The cortical center for smooth targeted or tracking movements of the eyeballs is located in the occipital-parietal region of the brain. Control is carried out from the side of the same name, i.e. the right occipital-parietal region of the brain controls smooth, targeted eye movements to the right.
Testing of targeted eye movements is carried out by tracking an object from the center to the periphery with the patient's head motionless.
Eye movement with changes in gravity and acceleration
Coordination of the movements of the eyeballs in response to changes in gravity and acceleration is carried out by the vestibular system (vestibular-ocular reflex). When the coordination of movements of both eyes is disturbed, double vision develops, since images are projected onto disparate (inappropriate) areas of the retina. In congenital strabismus, or strabismus, a muscle imbalance that causes the eyeballs to be misaligned (nonparalytic strabismus) may cause the brain to suppress one of the images. This decrease in visual acuity in the non-fixing eye is called amblyopia without anopia. In paralytic strabismus, double vision occurs as a result of paralysis of the muscles of the eyeball, usually due to damage to the oculomotor (III), trochlear (IV) or abducens (VI) cranial nerves.
Treatment of the optic nerve
Causes of development and classification of pathologies
Depending on the etiology of development, all diseases can be divided into the following types:
- congenital anomalies
. These include coloboma, hypergliosis, hypoplasia (underdevelopment), etc.; - vascular
. Pathologies develop against the background of acute circulatory disorders in the vessels supplying the nerve. The cause of such changes may be the formation of blood clots, atherosclerosis, hypertension or hypotension, bleeding, etc. An example is ischemic neuroopticopathy, congestive optic disc; - oncological
_ Most often, tumors are benign in nature, for example, meningioma, glioma. Malignant formations are rare and, as a rule, are metastases; - toxic
. As a result of intoxication, a degenerative process develops in the nervous tissue. Most often, toxic lesions occur due to poisoning with lead, carbon sulphide, methanol, denatured alcohol, as well as overdose of certain medications or abuse of alcoholic beverages and smoking. In the case of alcohol and nicotine addiction, in addition to the direct negative effect on nerve cells, the synthesis and absorption of B vitamins is disrupted, which gradually leads to descending atrophy of the optic nerve; - inflammatory
. Most often, neuritis, papillitis, opto-chiasmatic arachnoiditis, etc. are diagnosed; - traumatic
. Pathologies arise as a result of various head injuries, for example, a fracture of the skull bones in the area where the nerve passes, a cerebral hematoma (due to the compression effect, the functions of the visual organs are impaired); - infectious.
The pathological process can develop as complications of the underlying disease caused by pathogenic microorganisms (tuberculosis, typhus, toxoplasmosis, syphilis, malaria, etc.).
Timely diagnosis of the disease allows you to speed up the recovery process and reduce the risk of possible relapses. Only timely medical care can fully restore lost visual acuity.
The effectiveness of the prescribed therapy depends on making an accurate diagnosis and identifying the causes that caused the development of the disease. The following examination methods are used in neuro-ophthalmological practice:
- visometry
- determination of visual acuity using special tables; - perimetry
- an instrumental method for studying the visual field; - ophthalmoscopy
- examination of the fundus of the eye using instruments; - fluorescein angiography of the retina (FAG)
is a method that allows you to assess the condition of the vessels of the retina and choroid; - Ultrasound
of the orbit is a study that provides highly informative data on the state of the structures of the eyeball; - Magnetic resonance imaging
of the brain is a diagnostic method that allows you to obtain high-quality images of the anatomical area under study, which show the slightest pathological changes; - Heidelberg retinal tomography (HRT)
is one of the ways to visualize the optic disc.
Treatment methods
There are a number of reasons that cause pathologies of the optic nerve. Treatment of diseases, first of all, should be aimed at eliminating the relevant negative factors that led to the development of the disease.
Depending on the nature, form and stage of the pathological process, the following types of treatment may be prescribed:
- neurosurgical operation.
Indications for surgical intervention are intracranial tumors, cerebral aneurysm, etc.; - drug therapy.
Depending on the etiology of the disease, various medications are used: antibacterial, antiviral, corticosteroids, antispasmodics, thrombolytics and antihistamines, anticoagulants, vitamins C and B, etc.; - physiotherapeutic treatment.
Includes various physiotherapeutic procedures (for example, photoelectromagnetic stimulation of the optic nerve), which have a positive effect on the healing process and prevent the development of relapses.
Inflammatory diseases require emergency hospitalization of the patient. The chronic course of the pathology is usually treated on an outpatient basis.
Request a call back
Eyeball muscles and gaze palsies
There are three types of paralysis of the external muscles of the eyeball:
- paralysis of individual eye muscles
- paralysis of friendly movements (gaze)
- mixed paralysis
Paralysis of individual eye muscles
Characteristic clinical manifestations occur with isolated damage to the oculomotor (III), trochlear (IV) or abducens (VI) nerve.
Complete damage to the oculomotor (III) nerve leads to ptosis. Ptosis manifests itself in the form of weakening (paresis) of the muscle that lifts the upper eyelid and disruption of voluntary movements of the eyeball upward, downward and inward, as well as divergent strabismus due to the preservation of the functions of the lateral (lateral) rectus muscle. When the oculomotor (III) nerve is damaged, pupil dilation and lack of reaction to light (iridoplegia) and paralysis of accommodation (cycloplegia) also occur. Isolated paralysis of the muscles of the iris and ciliary body is called internal ophthalmoplegia.
The normal position of the eyeballs and convergent strabismus are shown with weakness of the lateral (external) rectus muscle of the eye on the right (n. abducens, VI pair of cranial nerves).
Injuries to the trochlear (IV) nerve cause paralysis of the superior oblique muscle of the eye. Such damage to the trochlear (IV) nerve leads to outward deviation of the eyeball and difficulty moving (paresis) downward gaze. Paresis of downward gaze is most clearly manifested when turning the eyes inward. Diplopia (double vision) disappears when the head is tilted to the opposite shoulder, which causes a compensatory inward deviation of the intact eyeball.
Damage to the abducens (VI) nerve leads to paralysis of the muscles that abduct the eyeball to the side. When the abducens (VI) nerve is damaged, convergent strabismus develops due to the predominance of the influence of the tone of the normally working internal (medial) rectus muscle of the eye. With incomplete paralysis of the abducens (VI) nerve, the patient can turn his head towards the affected abductor muscle of the eye in order to eliminate the existing double vision using a compensatory effect on the weakened lateral rectus muscle of the eye.
The severity of the above symptoms in cases of damage to the oculomotor (III), trochlear (IV) or abducens (VI) nerve will depend on the severity of the lesion and its location in the patient.
Friendly gaze paralysis
Companionate gaze is the simultaneous movement of both eyes in the same direction. Acute damage to one of the frontal lobes, for example, during cerebral infarction (ischemic stroke), can lead to transient paralysis of voluntary conjugate movements of the eyeballs in the horizontal direction. At the same time, independent eye movements in all directions will be completely preserved. Paralysis of voluntary conjugate movements of the eyeballs in the horizontal direction is detected using the doll eye phenomenon when passively turning the head of a horizontally lying person or using caloric stimulation (infusion of cold water into the external auditory canal).
Unilateral damage to the inferiorly located paracentral section of the reticular formation of the pons at the level of the nucleus of the abducens nerve causes persistent paralysis of gaze in the direction of the lesion and loss of the oculocephalic reflex. The oculocephalic reflex is a motor reaction of the eyes to irritation of the vestibular apparatus, as with the phenomenon of the head and eyes of a doll or caloric stimulation of the walls of the external auditory canal with cold water.
Damage to the rostral interstitial nucleus of the medial longitudinal fasciculus in the anterior midbrain and/or damage to the posterior commissure causes supranuclear upward gaze palsy. Added to this focal neurological symptom is the dissociated reaction of the patient’s pupils to light:
- sluggish pupil reaction to light
- rapid reaction of the pupils to accommodation (changing the focal length of the eye) and looking at nearby objects
In some cases, the patient also develops convergence paralysis (movement of the eyes towards each other, in which the gaze will focus on the bridge of the nose). This symptom complex is called Parinaud's syndrome. Parinaud's syndrome occurs with tumors in the pineal gland, in some cases with cerebral infarction (ischemic stroke), multiple sclerosis and hydrocephalus.
Isolated downward gaze palsy is rare in patients. When this occurs, the cause is most often blockage (occlusion) of the penetrating arteries in the midline and bilateral infarctions (ischemic strokes) of the midbrain. Some hereditary extrapyramidal diseases (Huntington's chorea, progressive supranuclear palsy) can cause restrictions in the movement of the eyeballs in all directions, especially upward.
Mixed paralysis of gaze and individual muscles of the eyeball
The simultaneous combination of gaze paralysis and paralysis of individual muscles that move the eyeball in a patient is usually a sign of damage to the midbrain or pons. Damage to the lower parts of the pons with destruction of the abducens nerve nucleus located there can lead to paralysis of rapid (saccadic) horizontal movements of the eyeballs and paralysis of the lateral (external) rectus muscle of the eye (abducens nerve, VI) on the affected side.
With lesions of the medial longitudinal fasciculus, various gaze disturbances occur in the horizontal direction (internuclear ophthalmoplegia).
Unilateral damage to the medial longitudinal fasciculus caused by infarction (ischemic stroke) or demyelination leads to disruption of the inward adduction of the eyeball (to the bridge of the nose). This can manifest clinically as complete paralysis with the inability to move the eyeball inward from the midline, or as a moderate paresis, which will manifest itself as a decrease in the speed of adducting rapid (saccadic) eye movements to the bridge of the nose (adductive delay). On the side opposite to the lesion of the medial longitudinal fasciculus, as a rule, abduction nystagmus is observed: nystagmus that occurs when the eyeballs are abducted outward with a slow phase directed towards the midline and fast horizontal saccadic movements. An asymmetrical arrangement of the eyeballs relative to the vertical line often develops with unilateral internuclear ophthalmoplegia. On the affected side, the eye will be positioned higher (hypertropia).
Bilateral internuclear ophthalmoplegia occurs with demyelinating processes, tumors, infarction, or arteriovenous malformations. Bilateral internuclear ophthalmoplegia leads to a more complete syndrome of eyeball movement disorders, which are manifested by bilateral paresis of the muscles that lead the eyeball to the bridge of the nose, impaired vertical movements, purposeful tracking movements and movements caused by the influence of the vestibular system. There is a disturbance of gaze along a vertical line, upward nystagmus when looking up and downward nystagmus when looking down. Lesions of the medial longitudinal fasciculus in the overlying (rostral) parts of the midbrain are accompanied by a violation of convergence (convergent movement of the eyes towards each other, towards the bridge of the nose).
Symptoms and clinical picture of ophthalmoplegia
The clinical picture of ophthalmoplegia consists of the following, partly determined objectively, partly subjective disorders:
• Limitation of eye mobility.
• More significant secondary ocular deviation.
• Diplopia.
• Visual dizziness and unsteady gait.
• Incorrect head position.
Limitation of eye mobility
It can be caused primarily mechanically, due to a tumor in the orbit, tenonitis, symblepharon, muscle disease, and so on; Of course, these causes must first be excluded so that a diagnosis of ophthalmoplegia due to loss or limitation of motor innervation can be made with complete certainty.
The most striking sign of ophthalmoplegia is a lack of eye mobility in one direction. Mobility can be completely lost (paralysis) or only weakened (paresis). Lack of mobility can, however, only be imaginary, due to the fact that the size and configuration of the palpebral fissure, the position of the lacrimal caruncle, and finally, the structure of the eye itself simulate it.
The (absolute) mobility of the eye is examined in such a way that one eye is closed and the other is forced to follow the movements of an object, for example a finger, in all directions to the most extreme physiological limits. The normal border is considered to be reached: outwardly, if the outer edge of the cornea touches the outer commissure of the eyelids, inwardly, if the inner edge of the cornea slightly extends beyond the lacrimal caruncle or if the lacrimal punctum approximately corresponds to the center of the pupil; up and down there are no definite boundaries, mobility in these two directions is individually very different, but with some skill here too you can soon find reference points for assessing mobility. With minor restrictions on mobility, clear results cannot be obtained in this way and therefore it is better to examine the (relative) mobility of both eyes together using the method just indicated. If at the same time one eye lags behind the other, then one can quite reasonably assume a disorder in the movement of this eye. Often, paralysis of the eye muscles is indicated by a peculiar twitching movement of the eye and even clear nystagmus, especially with extreme deviation of the eye to the side. Sometimes the mobility of both eyes may also be limited symmetrically in one or more directions; This especially happens when looking up, while such a restriction of friendly or associated movements to the right and left is rarely observed.
Finally, in all cases where ophthalmoplegia can be suspected, it is necessary to examine the ability of convergence, forcing the patient to fix the tip of the finger, which is increasingly brought closer to the tip of his nose; the lag of one eye, although it does not necessarily indicate paralysis, is still important for the assessment of other established symptoms.
More significant secondary eye deviation
If, when studying the relative mobility of both eyes, you move the fixed finger in the direction of the paralyzed muscle, it turns out that the paralyzed eye, due to the limitation of its mobility, cannot follow the finger beyond a certain limit, so only the healthy eye fixes. The visual lines of both eyes in this case are no longer set to the same fixation point; the visual line of the squinting eye is deviated, it converges or diverges with the visual line of the healthy eye, that is, the paralyzed eye squints. The degree of deviation, called primary, is measured by angle. If you now cover the healthy eye with frosted glass, then the paralyzed eye takes over the fixation, as far as possible. The paralyzed muscle now receives a stronger impulse, but is unable to follow it or only partially follows it. Half of this impulse is transmitted to the other, normally mobile eye, which therefore represents a very strong deviation, much more significant than the deviation of the other eye, limited by the limits of mobility of the affected muscle. This deviation, which can be accurately determined behind ground glass, is called secondary and, as follows from the above, in ophthalmoplegia it is greater than the primary deviation.
Diplopia
This is the most important symptom of ophthalmoplegia. At first it is often noticed only occasionally, but subsequently it always occurs when the eyes deviate in a certain direction. Diplopia, of course, does not occur when one eye is blind; Further, it should be noted that some patients very quickly learn to suppress the imaginary image.
Visual dizziness and unsteady gait
Vertigo is called visual dizziness because it is of peripheral origin, that is, caused by paralysis of the eye muscle, as opposed to cerebral dizziness. The named phenomena interfere especially with paralysis of the muscles that lower the eyes, and immediately disappear if the affected eye is closed. Usually the patient does this himself. In such cases, you can also place a prism with the base down in front of the diseased eye, and a prism with the base up in front of the healthy eye.
Incorrect head position
To relieve the affected muscle from a stronger contraction and prevent diplopia, the patient, every time he wants to look in a direction that requires a special action from the paralyzed muscle, completely impossible or only partially possible, turns his head so that his eyes are directed to the side, the opposite of diplopia. This head rotation is called “vicarious” because the neck muscles act instead of the paralyzed eye muscle.
The position of the head is pathognomonic for almost every paralysis and often this symptom alone can make a probable diagnosis. When turning the head to the left, the muscle that turns the eye to the left is paralyzed, for example, the left external rectus muscle; when turning and lowering to the left and slightly tilting the head forward, the superior oblique muscle is paralyzed.