Heart symptoms
With cardioneurosis, the main discomfort for patients comes from attacks of pain in the heart. Their intensity varies, as does the duration, which varies from 15 minutes to 2-3 days. An attack occurs mainly after stress. Its frequency is individual in each case. Suspicious people can experience discomfort 5 times a day. Other patients suffer from attacks of heart pain only 1-2 times a year due to nervous exhaustion.
Patients remember the manifested pain in the heart well and begin to worry greatly about their condition. The situation reaches the point of an obsession about imminent death. Cardiologists and therapists have to deal with particularly suspicious patients. Doctors try to explain to the patient that no organic lesions have been identified and recommend contacting a psychotherapist.
It is problematic to draw an overall clinical picture, since patients describe their condition in different ways. We have to focus on the most common cardiac symptoms of cardioneurosis:
- aching and throbbing pain combined with increased sensitivity of the skin on the part of the heart;
- feeling of emptiness in the chest;
- pain throughout the left half of the body with a focus in the heart area;
- pain radiating to the back, head, neck and genitals;
- pressing sensation in the chest;
- stabbing and cutting sensations in the chest, preventing deep breathing.
Pain in the chest is not relieved by Nitroglycerin tablets and other cardiac medications and decreases only after rest. You can distinguish an attack of cardioneurosis from heart disease by the following nuances in the patient’s behavior:
- When describing the symptoms of heart neurosis, the patient tries to embellish it and each time the story changes a little.
- An attack of cardioneurosis causes a person to have obsessive thoughts about imminent death and the “severity” of cardiac pathology. He becomes overly concerned about his health and often experiences panic attacks.
- An attack causes a person to fuss excessively, actively gesticulate, alternately apply cold and heat to the chest, and take all kinds of heart medications.
People who actually suffer from diseases of the cardiovascular system behave with restraint. They can take the medication recommended by the doctor and call an ambulance if necessary. With neurosis, a person is excessively fussy, which reveals his real illness. Calling an ambulance during an attack is often provoked by obsessive thoughts. Visiting doctors must distinguish real cardiac pathology from a panic attack and advise how to treat cardiac neurosis.
Cardioneurosis: symptoms
Neurotic disorders also include cardioneurosis (neurosis of the heart). This is not an independent disease. We speak of “neurosis of the heart” when cardiac symptoms predominate in a person with a neurotic disorder. This:
- pain in the heart area;
- heart rhythm disturbances (palpitations, “fading heart”);
- feeling of lack of air and shortness of breath;
- cold sweat, trembling, chills, etc.
Pain in the heart (sharp or aching, squeezing or bursting, throbbing, stabbing, etc.) often occurs at rest and does not intensify with physical activity. It can radiate to the neck, shoulder blade, back, and genitals. Cannot be removed by nitroglycerin.
Symptoms of cardioneurosis may not be accompanied by cardiac pathology for a long time and reflect only functional disorders of cardiac activity. But there is always a risk of their “materialization” and the development of serious heart diseases (coronary heart disease and its complications - myocardial infarction). Moreover, with cardiac neurosis, the activity of not only the cardiovascular, but also other vital systems in the body suffers.
General clinical picture
The cardiac symptoms of cardioneurosis worry patients most of all, but other manifestations are also characteristic of the disease. Their intensity varies depending on the individual characteristics of the person. General symptoms of cardiac neurosis during an attack are usually the following:
- a feeling of anxiety that develops into panic;
- obsessive thoughts (obsessive syndrome) about imminent death and the development of fatal pathologies;
- feeling of a lump in the throat;
- lack of oxygen;
- frequent shallow breathing;
- feeling tired even with the slightest overload;
- inability to take a deep breath;
- headache;
- excessive sweating;
- alternating sensations of heat and cold throughout the body;
- loss of consciousness or faintness.
After the attack ends, the person feels a loss of strength and drowsiness. Heavy thoughts appear in your head that prevent you from falling asleep at night.
Symptoms and diagnosis of cardioneurosis
Doctors diagnose cardioneurosis as an independent disease only in the absence of signs of somatic pathology. To identify cardioneurosis, in addition to carefully collecting anamnesis and physical examination of the patient, cardiologists at the Yusupov Hospital conduct a number of studies depending on the complaints:
- Blood and urine tests;
- Registration of electrocardiogram;
- Echocardiography;
- 24-hour Holter electrocardiogram and blood pressure monitoring;
- Load tests (bicycle ergometry, treadmill test);
- Study of external respiration function (peak expiratory flow, capnography, blood gas composition, voluntary hyperventilation test, spirometry);
- Esophagogastroduodenoscopy.
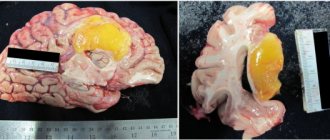
Patients are advised by related specialists: neurologist, ophthalmologist, otolaryngologist, endocrinologist and psychiatrist. To exclude organic pathology of the brain, electroencephalography and magnetic resonance imaging are performed.
Patients with cardioneurosis are characterized by the presence of the following manifestations of the disease over two consecutive years:
- A variety of somatoform disorders that occur continuously or occur episodically and mimic the symptoms of a disease of the cardiovascular system (bodily fantasies, heart pain, heart pain);
- Anxiety-phobic disorders (fear of heart attack, stroke, death from cardiac arrest), which are accompanied by sensations of irregular heartbeat with a tendency to increase heart rate, lability of blood pressure, acute vegetative symptom complexes that imitate urgent cardiovascular pathology (impaired consciousness when standing up suddenly, dizziness , fainting);
- Affective symptom complexes (hypomania, depression).
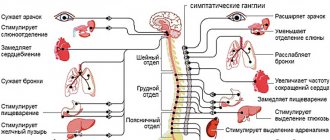
Other signs of cardioneurosis are symptoms of autonomic dysfunction:
- Local sweating;
- Coldness or marbling of the extremities;
- Persistent white dermographism.
In 30% of patients suffering from cardioneurosis, instrumental research methods reveal congenital morphological anomalies of the heart that do not have clinical manifestations (additional chord, mitral valve prolapse), lability and nonspecific changes in the final part of the ventricular complex. Cardiologists believe that the detected functional and minor morphological deviations from the norm do not explain the patients’ complaints.
Cardiologists distinguish the following types of cardioneurosis:
- Cardialgic (manifested by discomfort in the chest, pain in the heart area, strong heartbeat or pulsation throughout the body, attacks of palpitations, fading in the heart, interruptions in the heart);
- Respiratory (the patient feels short of air, has rapid breathing, cannot take a full inhalation or exhalation, feels a “lump” in the throat, suddenly takes deep breaths);
- Dysdynamic (high blood pressure is replaced by low blood pressure);
- Thermoregulatory (body temperature constantly or intermittently rises to 37-38°C or drops to 35°C);
- Dyspeptic (abdominal pain, belching, nausea, vomiting, impaired intestinal motor function);
- Asthenic (concerns about weakness, irritability, fatigue, sleep disorders, headaches).
Many patients experience vegetative crises. They manifest themselves as trembling, unaccountable fear, chills, a feeling of lack of air, dizziness, and a feeling of internal tension. Patients feel hot or cold flashes, their blood pressure increases or decreases, redness or paleness of the skin occurs, sweating, chilliness, numbness of the hands and feet appear.
Causes
The development of cardioneurosis is influenced not only by external factors, but also by internal ones. A full list of reasons can be seen below:
- hormonal surges associated with illness, adolescence, pregnancy, menopause, taking medications;
- long-term course of pathology without improvement;
- constant feeling of stress;
- insomnia;
- frequent physical and mental overload;
- intoxication due to the effects of chemical compounds on the body;
- bad habits;
- poorly designed diet.
In childhood, the cardiac type of neurosis occurs against a background of stress during school or due to quarrels in the family, parental divorce and other factors that negatively affect the fragile psyche. In adolescence, the reasons remain the same, but the situation is aggravated by hormonal changes.
Causes of cardiac neurosis
In cardioneurosis, pain attacks are not associated with pathology of the cardiovascular system. Excessive worries, stress and other types of psycho-emotional stress put stress on the heart. They are the ones that cause unpleasant symptoms.
The following factors can provoke neurosis:
- Hormonal changes during adolescence and pregnancy.
- Endocrine diseases, in particular thyrotoxicosis.
- Chronic lack of sleep.
- Long-term stressful conditions, depression.
- Protracted illnesses, long-term treatment, especially in a hospital.
- Overwork at school or at work, irregular work schedule.
- Intense, exhausting physical activity.
- Chronic poisoning with alcohol and nicotine.
- Poor nutrition.
Heart neurosis is often diagnosed in people with a certain type of behavior. Thus, patients are characterized by the following features:
- Suspiciousness.
- Conflict.
- Excessive self-control.
- Mood swings.
- Tendency to panic and hysterics.
Attacks of cardioneurosis can begin against the background of various phobias. Risk factors most often include fear of the dark, claustrophobia, being in a crowd, fear of death, etc.
First aid
The manifestation of cardioneurosis is difficult to predict, especially if a person has not previously experienced such discomfort. You can find out how to get rid of an attack of heart neurosis from the information below:
- During an attack, it is better for the patient to find a well-ventilated room to compensate for the lack of oxygen.
If possible, it is advisable to lie down on a sofa or bed. If they are missing, the floor will do.- Take any mild drug with a sedative (calming) effect (Valocardin, alcohol tinctures of motherwort, lemon balm, valerian).
- Take your pulse. If it can be easily felt and does not malfunction, this means that there are no severe functional impairments.
- Calm down and lie down, trying not to think about anything. Excessive fuss, constant measurements of pressure, pulse and calls to relatives and friends will only increase anxiety.
Relief occurs in about 15-20 minutes. To prevent further attacks, it is advisable to consult a therapist. He will send you for an examination and, based on its results, will draw up a list of recommendations. Drug treatment is required only in severe cases. In most cases, you can get by with lifestyle correction and traditional medicine. If the pain in the heart does not go away or the patient is in a pre-fainting state, then it is necessary to call an ambulance.
Drug treatment
Drugs are prescribed to relieve pain, normalize heart rhythm, relieve shortness of breath and calm the nervous system. The following groups of medications are mainly used:
- It is advisable to use sedative medications for a course lasting at least 1-2 months to obtain a lasting effect. Alcohol tinctures of herbs (motherwort, peppermint, valerian) and medications with a sedative effect (Valocordin, Validol, Persen) are used.
- Antidepressants (Pyrazidol, Amitriptyline, Imizin) suppress depression, improve mood and stimulate the nervous system. Initially, they often cause drowsiness due to the strong sedative effect, but the side effect gradually wears off.
- Tranquilizers (Seduxen, Phenazepam, Nitrazepam) relieve nervous tension and eliminate anxiety and fear. If the patient is more concerned about phobias that arose against the background of an attack of cardioneurosis, then it is better to take Seduxen. Nitrazepam effectively helps with insomnia, and Phenazepam is used to suppress depression.
- Associated headaches can be eliminated with analgesics (Citramon, Spazgan, Drotaverine).
- Vitamin complexes with a high concentration of B vitamins (“Neurovitan”, “Neuromultivit”) are used to improve the condition of the nervous system.
Potassium-containing drugs (Asparkam, Orocomag) are used to stimulate the conductive function of the heart and normalize the transmission of nerve impulses.
Vitamins, potassium-containing preparations and alcohol tinctures with a sedative effect can be taken without any particular concern. For chemical-based analgesics and sedatives, it is necessary to study the contraindications. It is prohibited to take antidepressants and tranquilizers on your own. They have a strong effect on the nervous system, so they are sold by prescription.
The exceptions are children under 18 years of age and women during pregnancy and breastfeeding. For these groups, drug therapy is selected only by the attending physician, who, after the examination, will tell you how to treat cardiac neurosis and advise safe methods. In other cases, you can self-medicate only at your own peril and risk.
Cardioneurosis: symptoms and course
The presence of hormonal imbalance, the use of psychotropic substances, alcohol, physical stress on the body, which manifests itself in the form of lack of sleep, a fair amount of workaholism - all this can serve as a catalyst for the appearance of cardioneurosis. This happens because the vital organ works more intensely in order to maintain homeostasis and restore the human body and leads to a disruption in comfort in the chest area, when various pains, spasms and other unpleasant sensations appear. For a person who has experienced this, an incredible fear “for his health” appears; he begins to suspect that he has a serious heart pathology and fears for his life; a fear of death appears. But when the patient understands the essence of what is happening and the causes of pain in the heart area, it becomes easier for him to endure this condition.
Anxious, psychosthenic, individuals prone to hypochondriacal fixation may focus too much of their attention on these symptoms, which will only hinder them in the future, and the symptoms will manifest themselves more often and more intensely. In these cases, patients associate pain in the heart area with panic attacks and all kinds of phobic disorders that can accompany cardiac neurosis. And this further contributes to the occurrence of vegetative crises without a physical cause. And the circle closes! A person experiences real fear and panic before a repetition of this condition, automatically “triggering” the symptoms of cardioneurosis. This can be repeated several times throughout the day!
With cardioneurosis, neurosis-like symptoms are observed, similar to the manifestation of a hypertensive crisis, and pronounced vegetative symptoms.
With cardioneurosis, the following conversion and psychopathological manifestations are observed:
- instability when moving,
- general weakness and lethargy in the body,
- inner restlessness
- failure of sleep-wake processes,
- pressing pain in the chest, in the region of the heart, etc.,
- there is a lump and tightness in the throat,
- limbs go numb like “gloves and socks”,
- difficulty breathing, feeling suffocated,
Autonomic manifestations of cardioneurosis:
- increased heart rate,
- irregular pulse,
- increased sweating,
- feeling of chills, intermittent flashes of cold and heat, etc.
It should be noted that the severity of typical complaints in cardioneurosis, characteristic of patients with hypertensive crisis (dizziness, chest discomfort, throbbing headache, sensation of “floaters in the eyes,” feeling of nausea), often do not correspond to the symptoms that should manifest themselves in low or moderate blood pressure levels.
During an “attack” of cardioneurosis, chest pain of various colors (cardialgia) can also be observed: stabbing, burning, squeezing, pressing pain behind the sternum and under the scapula. Patients can characterize these pain-sensations as “a feeling of emptiness in the chest”, “a heart squeezed in a vice.” Some patients experience “cardiac arrest.” And very significant for correct diagnosis, of course, is the fact that such painful, unpleasant and often numerous complaints and sensations manifest themselves without the presence of heart pathologies.
With cardioneurosis, panic and anxiety-phobic symptoms are often present (fear of dying, having a heart attack or stroke). And it is no longer clear what is true - high blood pressure (BP) causes anxiety, panic and fear, or, rather, they “catch up” with the BP numbers.
Such a panic attack, which is accompanied by elevated blood pressure numbers, usually lasts up to half an hour or even less. This requires the use of psychotropic therapy, since only the use of antihypertensive drugs has no effect. A panic attack can often “feel like” a hypertensive crisis, which “passes at the tip of a needle” when tranquilizers are administered intravenously.
Non-drug therapy
Treatment of cardioneurosis is possible without pills. The essence of non-drug treatment is lifestyle correction:
- try not to get into stressful situations;
- maintain a positive attitude;
- work no more than 7-8 hours a day and take 5 minute breaks once every hour and a half;
- devote at least 6-8 hours to sleep;
- do not overwork physically and mentally;
- walk in the fresh air for 1-2 hours every day;
- exercise (moderately), do morning exercises;
- give up bad habits (smoking, drinking alcohol).
Gymnastics for cardioneurosis should be moderate and aimed at strengthening the heart muscle. Running, swimming and aerobic exercise are good options.
The patient will have to change his diet to get rid of heart neurosis. By giving up fast food, sweets, spices and other unhealthy foods in favor of healthy foods, you can significantly improve your overall health. The daily menu should include more vegetables and fruits. It is advisable to eat at least 4-5 times a day, in small portions. The last meal should be 3-4 hours before bedtime.
People who spend most of their time working need to dilute their busy schedule. You should rest at least 2-3 hours a day, doing your favorite hobby, listening to music or going to a massage.
Psychotherapy
Taking medications alone can stop the manifestations of the disease, but cannot eliminate its cause. To completely cure cardioneurosis, you will have to normalize the functioning of the nervous system with the help of a psychologist or psychotherapist. Communication with a specialist will eliminate the feeling of anxiety, clear your head of obsessive thoughts and strengthen your psyche to effectively resist panic attacks.
Specialists mainly use the following methods of psychotherapy:
- Rational treatment. The doctor helps the patient understand why attacks occur and then teaches him how to effectively deal with them.
- Cognitive behavioral therapy. During the conversation, the psychotherapist talks about the patient’s actions that provoke the development of cardioneurosis and points out his mistakes in order to prevent their recurrence in the future.
- Family sessions. You can come to a conversation with a specialist with close people with whom the patient spends most of his time. Family psychotherapy is most effective for treating couples and children. During the sessions, the doctor will learn about problems and recommend methods to eliminate them.
- Hypnosis is used if the patient is unwilling or unable to share the hidden reasons for his condition. The specialist will put him to sleep and learn about all the problems on a subconscious level.
To achieve noticeable results, it usually takes about 10-15 sessions. It is advisable to combine them with lifestyle correction. The doctor will recommend drug treatment if necessary.
Folk remedies
Folk remedies help with the treatment and relief of symptoms of heart neurosis. In most cases, herbal teas with a sedative effect are used. They actually have no contraindications, except for individual intolerance, but during preparation it is important to follow the dosages indicated in the recipe. If you exceed them or underestimate them, the effect will be too strong or completely absent. As a standard, 1-2 tbsp is taken for preparing the decoction. l. main ingredient per 500 ml of water or alcohol. Then the resulting mixture is thoroughly mixed and left to infuse.
The following folk remedies are the most effective for treating and relieving symptoms of heart neurosis:
- A decoction of mint and valerian roots calms the nerves well. You can prepare the medicine by taking 1 herb or both in equal proportions. It is taken instead of tea, 2 times a day.
- The combination of dried apricots, raisins and hawthorn, viburnum and rowan fruits will saturate the body with the microelements necessary for the normal functioning of the heart and nervous system. Prepare like a regular decoction. You can drink it instead of tea 2-3 times a day.
- Drink warm milk at night with the addition of 1 tsp. honey improves sleep and calms the nervous system.
The following fees can be used as a remedy for the treatment of cardioneurosis:
- mint, valerian roots, hop cones, three-leaf watch;
- hawthorn fruits, oregano, motherwort;
- hop cones, yarrow, valerian roots, lemon balm.
After preparing one of the decoctions, it should be taken 3 times a day, 100 ml. Course duration – 1 month. If allergy symptoms occur, treatment of heart neurosis with folk remedies is stopped, and you should consult a doctor as soon as possible.
Symptoms
Cardiac neurosis manifests itself mainly by two signs: pain in the heart area and cardiac arrhythmia. But behind the apparent simplicity of the symptoms there are many pitfalls.
Pain syndrome
A painful attack during cardioneurosis can have a different duration and character.
Heart neurosis is characterized by paroxysmal pain. The appearance of pain can be triggered by excitement (for example, a quarrel with a loved one, passing an exam) or physical activity. Less commonly, pain due to cardiac neurosis occurs for no apparent reason. The duration of the attack can vary: from several minutes (which happens less often) to several hours. The pain may bother the patient only a few times a year, or it may recur more than once a day.
One of the features of the pain syndrome in cardiac neurosis is the wide variety of its nature. What does this mean? And the fact is that the pain with heart neurosis can, by and large, be anything: aching, shooting, stabbing, squeezing or squeezing, and burning. At the same time, there is no pattern in the nature of the pain syndrome in one patient. The attacks of pain may be the same, or they may occur differently each time. The only thing that unites them is almost always a bright emotional coloring. The feeling of pain in the area of the heart or chest with cardiac neurosis almost always makes the patient fear for his life. Often the appearance of pain is associated with a feeling of lack of air, which aggravates already negative emotions. Sometimes a painful attack leads to a panic attack. Patients with cardiac neurosis are characterized by fussiness during an attack, which manifests itself not only in emotions (“something must be done”), but also in excessive movements. Patients rush around in unsuccessful attempts to take a position that will relieve the pain. In this way, the pain syndrome during neurosis differs from true pain in the heart during an attack of angina, when patients, on the contrary, freeze, trying to make as little movements as possible, because the latter can increase the pain.
In fact, any pain in the heart area due to its neurosis is quite harmless, because it is not at all life-threatening. Apart from unpleasant sensations and emotional experiences, this pain does not cause anything else, because the heart muscle itself remains completely healthy, and blood flow through the vessels of the heart is not disturbed. But this fact is very difficult to convey to the patient himself. A person with heart neurosis may be so scared at the time of an attack that nothing can convince him otherwise.
When a patient with neurosis describes his feelings during an attack of pain in the heart area, one can often hear such colorful formulations as:
- “the heart is squeezed in a vice”;
- “the heart grows numb”;
- “the heart is covered with ice”;
- “my heart is about to burst”;
- "The heart is on fire."
The occurrence of pain may be accompanied by profuse sweating and a feeling of a lump in the throat. The pain itself can have different localization, that is, it can be felt not only in the heart area. Often patients indicate irradiation of pain in the area of the left shoulder blade, left arm, lower jaw, teeth, spine and even genitals.
Almost every person knows that if pain occurs in the heart area, you should try taking Nitroglycerin or Validol under the tongue. So, with heart neurosis, these drugs will not have any effect on pain. And this fact is one of the criteria for differentiating the causes of pain in the heart. Nitroglycerin and Validol reduce pain during angina pectoris by dilating the blood vessels of the heart and causing increased blood flow.
Heart rhythm disturbances
This sign of cardiac neurosis is less diverse than pain syndrome. In most cases, an attack of pain in the heart area is accompanied by a feeling of palpitations, that is, an increase in heart rate. At the same time, sometimes there is a feeling as if a heart is beating in every cell of the body, pulsation can be heard everywhere. Sometimes similar sensations can be present without an increase in heart rate.
The second variant of heart rhythm disturbances in cardiac neurosis is arrhythmia, that is, a violation of the regularity of heart contractions (when different time intervals occur between individual heartbeats). At such a moment, the patient may say that it seems to him as if his heart has stopped (“heart has stopped”).
Both types of heart rhythm disturbances can be recorded using an ECG or Holter monitoring (24-hour ECG recording). With cardiac neurosis, single extrasystoles (extraordinary contractions of the heart) may occur. If, during an ECG, other heart rhythm disturbances are recorded (for example, bundle branch blocks, atrial fibrillation, frequent extrasystoles, and others), then the diagnosis of cardiac neurosis becomes unlikely, because these heart rhythm disturbances are provoked by other (real) heart problems. What type of heart rhythm disturbance is present in a patient can only be judged by the results of additional examination methods (in particular, ECG and Holter monitoring).
Often the pain syndrome is combined with a feeling of palpitations.
Heart neurosis can occur at any age. Those at risk are workaholics and emotionally unstable individuals. Neurosis is more common in women than in men.
As you can see, symptoms of cardiac neurosis are not so rare. But the whole problem is to distinguish pain due to heart neurosis (that is, when it is essentially healthy) from those due to true heart disease. And this is where the difficulties begin, because it’s not enough to just go to the doctor for an appointment and talk about your feelings. And under no circumstances should you self-diagnose. Pain in the heart area is always a reason to visit a doctor. And in order to determine what causes the pain syndrome, the doctor will need both a thorough collection of complaints and a careful examination, as well as the appointment of additional research methods. The minimum set of additional research methods in the presence of pain in the heart area includes an ECG and ultrasound of the heart. Other examinations are prescribed as necessary and taking into account changes detected by ECG and ultrasound.
All this is necessary primarily in order not to miss real cardiac pathology. A diagnosis such as “heart neurosis” has the right to exist only if additional research methods have proven the absence of other heart diseases. Because, for example, an attack of compressive pain behind the sternum may indicate angina pectoris, which is a harbinger of myocardial infarction. And this is already a life-threatening condition. And there can be many such examples. Therefore, the primary task when pain in the heart occurs is to exclude other, more severe and dangerous diseases (heart defects, myocarditis, coronary heart disease, and so on). And only if a comprehensive examination does not reveal any problems, then the most likely diagnosis becomes “heart neurosis.”
Forecast
Cardioneurosis is successfully eliminated in the early stages. Residual effects and relapses do not occur with an integrated approach to treatment.
In its advanced state, the disease has a detrimental effect on the patient’s psycho-emotional background. He becomes suspicious, overly irritable and fearful. A constant feeling of anxiety negatively affects all internal processes. Basically, the stool is disrupted, hypertension and angina develop. Treatment will be aimed at reducing nervous excitability and stabilizing the digestive and cardiovascular systems.
Cardioneurosis is a psychosomatic disease. Its development is provoked by frequent stress and overwork. The main problem arises in the diagnostic process. To differentiate cardiac neurosis, the therapist will have to exclude all similar pathological processes. After successful diagnosis, the patient is given recommendations for lifestyle correction. In advanced stages, medication may be prescribed. Psychotherapy and folk recipes are successfully used to complement the course of treatment.