In neurosurgical practice, brain tumors are divided into primary and secondary. Primary ones include those that are formed in brain tissue, nearby lymph nodes, cranial nerves, and blood vessels. Secondary (daughter) are the result of metastasis of cancer cells from other organs.
The choice of therapy depends on the histological type and location of the tumor. The main methods of treatment include scalpel or laser operations, chemotherapy and radiotherapy. Very often all these methods are combined with each other.
Surgical intervention
Brain surgery is a complex, time-consuming process, the consequences of which are unpredictable and determined by the location of the tumor. Any complications, such as bleeding, infections, damage to blood vessels and nerve fibers, swelling, can lead to negative cognitive and motor changes:
- paresis - loss of muscle strength with impaired coordination and gait, tremors of the limbs;
- apraxia - the inability to perform habitual or consistent movements necessary to carry out goal-directed tasks;
- agnosia – the inability to identify objects through the senses due to disorders of information perception: auditory, visual, gustatory, olfactory, tactile, spatial;
- hemianopsia – loss of visual fields;
- aphasia – complete or partial loss of speech;
- dysarthria – distorted and difficult pronunciation of certain sounds and words;
- alexia – difficulties in recognizing letters and understanding the meaning of what is read;
- agraphia – loss of writing skills, coordination of letters, prepositions, syllables, even with preserved intelligence;
- deterioration of memory, attention, thinking.
Mental dysfunction may also occur for another reason. During the period of tumor growth, the brain was subjected to compression of certain sections responsible for certain functions, to which it managed to adapt. But as a result of the removal of the neoplasm, the tissues find themselves in an unusual position for them, and this also becomes the basis for disruptions in cerebral activity.
Priority is given to the surgical method when the malignant tumor has clear boundaries. Contraindications for surgery are:
- multiple foci of the tumor process;
- severe chronic diseases in the acute stage;
- metastatic lesions of surrounding tissues;
- cachexia – extreme exhaustion.
Increasing headaches in the postoperative period are rare and should be reported to medical staff immediately, as they signal intracranial edema. In such a situation, drips with analgesics are prescribed and steroids are added.
Consequences of brain tumors
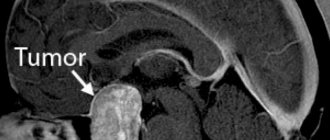
Brain tumors are a group of intracranial neoplasms of a benign or malignant nature, the formation of which is caused by uncontrolled cell division.
There are primary and secondary brain tumors. Primary tumors are formed in the tissues of the brain and nearby structures (vessels, cranial nerves, meninges, lymphatic tissue), secondary tumors are the result of metastasis from other affected organs.
Treatment of brain cancer depends on the location of the tumor and its histological type. The main methods of treating brain tumors are surgery (scalpel or laser surgery), radiotherapy and chemotherapy. Most often, treatment methods are combined. For example, the use of radiation therapy is combined with chemotherapy.
Consequences
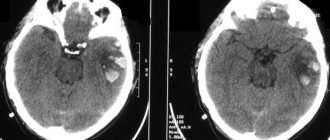
Brain surgery is a complex, time-consuming process. The consequences of the operation directly depend on the location of the tumor. Complications such as bleeding (hemorrhagic penetration of brain tissue), cyst formation, possible infectious lesions and swelling, lead to motor and cognitive disorders: paresis, apraxia, agnosia (impaired visual, tactile, spatial and auditory perception), speech disorders (aphasia, dysarthria), memory, attention and thinking disorders. Primary visual and hearing impairments, loss of visual fields, and impaired ability to read (alexia) and write (agraphia) are also possible. Another mechanism leading to disruption of higher mental functions is that during the growth of the tumor in the brain, compression of certain structures and sections responsible for a particular function occurred. However, during the course of the illness, the body manages to gradually adapt to this condition, and cognitive impairment becomes less pronounced. But after surgical removal of the tumor, the brain tissue suddenly gets rid of the pressure exerted, and at this moment, an exacerbation of brain dysfunction is possible.
After radiation therapy, the patient may also experience radiation reactions due to the damage and breakdown of cells in the surrounding brain tissue by gamma rays. Increased fatigue, weakness and lethargy, appetite disturbances, headaches, convulsions, and distortion of taste sensations are possible.
Chemotherapy, and especially drugs from the anthracycline group, can have a neurotoxic effect on the human brain, which is expressed in disorders of higher mental functions, memory disorders and intellect.
Three-stage therapy for brain cancer (surgery + radiotherapy + chemotherapy) is a very effective regimen. However, treating a tumor is a complex process that requires a lot of mental and physical strength, so it is important to professionally help the patient restore their quality of life and overcome the consequences of the disease and its treatment.
Treatment
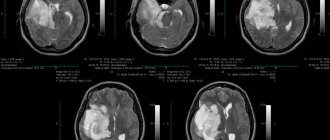
The recovery process after cancer therapy can take a long time. It is necessary to begin neurorehabilitation of such a patient as early as possible in order to effectively restore lost brain functions. In our clinic, neurorehabilitation is an interdisciplinary approach to restoring higher mental functions with the involvement of doctors and specialists in related fields - the department of therapeutic pedagogy. A neurological examination and the results of functional diagnostic methods (MRI, CT) allow a neurorehabilitation specialist to clearly establish the nature and extent of postoperative and post-radiation consequences.
Next, the neurorehabilitation specialist develops an individual rehabilitation training program with a neuropsychologist, speech therapist, and speech pathologist, combined with drug neurological therapy and other treatment methods. The neurorehabilitation specialist supervises the work of each specialist and combines their efforts in order to treat the patient as effectively as possible.
In our clinic, the Neurorehabilitation program is used for both adults and children.
Chemotherapy
Chemotherapy drugs can have a neurotoxic effect on the central nervous system, resulting in cognitive impairment. The effect of cytostatics is expressed in the cessation of the processes of growth, development, and the mechanism of cell division, unfortunately, not only malignant, but also normal. Antitumor agents are administered in various ways:
- orally – through the mouth;
- parenterally - by administering intramuscular, intravenous, intra-arterial injections;
- directly into the tumor itself or surrounding tissues;
- in the cavities remaining after removal;
- into the epidural space (cerebrospinal fluid).
Since all these drugs are substances with high biological activity and lack of selectivity, the bone marrow, mucous membranes of the digestive system, and hair follicles are affected. The severity and frequency of adverse events depend on the type of cytostatic, dosage used, administration regimen, and general condition of the patient. The most common side effects:
- inhibition of hematopoiesis (leukopenia, thrombocytopenia, anemia);
- symptoms of intoxication – nausea, vomiting, diarrhea;
- stomatitis;
- alopecia – loss of hair on all parts of the body;
- allergic reactions - rash, skin itching, erythema;
- development of cardiomyopathy;
- neurotoxicity;
- hepatotoxicity;
- nephrotoxicity;
- thrombophlebitis and phlebosclerosis;
- local irritating effect with necrosis and ulceration up to exposure of tendons and muscles;
- flu-like syndrome - chills, fever, weakness, headache and muscle pain.
The selection of a specific drug depends on the sensitivity of living cancer cells taken from the human body to it. Resistance is determined through testing, which makes it possible to avoid taking ineffective drugs and not waste time.
Radiation therapy
At the end of its implementation, undesirable reactions may also occur due to the effect of gamma rays on nearby tissues, damage and decay of destructive cells. They develop 1-2 weeks after treatment, manifesting themselves in the form of:
- reduction of leukocytes, platelets, red blood cells;
- general intoxication – nausea and vomiting;
- dryness, peeling, itching of the skin of the head and neck, red spots, blistering rashes;
- hemorrhages, ulcers, soft tissue burns;
- hearing loss due to swelling of the auditory canal;
- diplopia (double vision);
- hair loss;
- loss of appetite;
- feelings of fatigue and malaise;
- impaired coordination and seizures.
This treatment is used both individually and in the postoperative period to remove residual structures growing into surrounding tissues.
One of the methods of radiation therapy is stereotactic radiosurgery, the principle of which consists in a single irradiation of pathological foci with high doses using the Gamma Knife and CyberKnife devices. It is an alternative to traditional operations and allows manipulations to be performed without general anesthesia, tissue excision and craniotomy. It is characterized by high accuracy and low risk of complications. The big disadvantage of the technique is the delay in the result, so in cases of acute symptoms it is not used.
Contraindications after surgery
Despite the great successes of modern medicine in creating new protocols and equipment, treating pathology is a rather complex process that requires physical and mental effort. Rehabilitation after removal of a brain tumor under the guidance of professionals will help you overcome the consequences of the disease and return to your previous lifestyle. And it begins with a number of prohibitions under which the following are unacceptable:
- drinking alcohol for a long period;
- visits to the sauna, bathhouse;
- air travel for three months;
- active sports throughout the year, which pose a risk of head injury (hockey, football, boxing);
- exposure to the sun and solarium;
- jogging. It is better to replace them with brisk walking;
- sankur and mud therapy.
Rehabilitation
After removal of a brain tumor, a long period of rehabilitation begins, the goal of which is to maximize the restoration of the lost functions of the patient’s body.
It is very important to be constantly vigilant after treatment for a brain tumor in order to detect a possible relapse of the disease in time.
Purpose of rehabilitation
The most important thing is to achieve the maximum possible restoration of lost functions in the patient and return him to everyday and work life independent of others. Even if a complete restoration of functions is not possible, the primary goal is to adapt the patient to the limitations that have arisen in order to significantly make his life easier.
The rehabilitation process should begin as early as possible to prevent a person from becoming disabled.
Recovery is carried out by a multidisciplinary team, which includes a surgeon, chemotherapy, radiologist, psychologist, exercise therapy doctor, physiotherapist, exercise therapy instructor, speech therapist, nurses and junior medical staff. Only a multidisciplinary approach will ensure a comprehensive, high-quality rehabilitation process.
Recovery takes on average 3-4 months.
Rehabilitation goals:
- adaptation to the consequences of the operation and to a new lifestyle;
- restoration of lost functions;
- training in certain skills.
A rehabilitation program is drawn up for each patient and short-term and long-term goals are established. Short-term goals are tasks that can be accomplished in a short period of time, for example, learning to sit up in bed independently. Once this goal is achieved, a new one is set. Setting short-term goals divides the long process of rehabilitation into certain stages, allowing the patient and doctors to assess the dynamics of the condition.
It must be remembered that the disease is a difficult period for the patient and his relatives, because treating tumors is a difficult process that requires a lot of physical and mental strength. That is why the role of a psychologist (neuropsychologist) in this pathology should not be underestimated, and his professional help is usually needed not only by the patient, but also by relatives.
Physiotherapy
Exposure to physical factors after surgery is possible; treatment in this case is symptomatic.
In the presence of paresis, myostimulation is used, in case of pain and swelling, magnetic therapy is used. Phototherapy is also often used.
The possibility of using laser therapy in the postoperative period should be discussed by attending physicians and rehabilitation specialists. However, do not forget that laser is a powerful biostimulator. So it should be used extremely carefully.
Massage
If the patient develops paresis of the limbs, massage is prescribed. When it is carried out, the blood supply to the muscles, the outflow of blood and lymph improves, the joint-muscular feeling and sensitivity, as well as neuromuscular conduction, increase.
What is included in rehabilitation
Recovery takes quite a long time, and in order to restore previous brain functions, you need to start neurorehabilitation as early as possible. For this purpose, specialists from many fields and various equipment are involved. A multidisciplinary team of doctors, teachers, and nursing staff develops an individual program adapted to each patient. Drug neurological therapy is combined with the services of a defectologist, neuropsychologist, and speech therapist. Among the methods used:
- physiotherapy using inductothermy, laser therapy, UHF, electrophoresis, magnetic therapy to stimulate metabolism, relieve pain, accelerate regeneration, etc.;
- Exercise therapy with special simulators aimed at increasing the mobility of the limbs, fine motor skills of the hands, reducing swelling and stiffness in them. Exercises will help restore body balance, the ability to sit, stand and walk;
- kinesiotherapy and acupuncture - influencing bioactive points to stimulate all kinds of biological processes;
- psychotherapeutic assistance - relieving signs of depression, overcoming fears and complexes, acquiring a positive attitude;
- therapeutic massage – improving blood supply, elasticity and muscle tone, increasing immunity;
- occupational therapy – training in self-care, personal hygiene, acquisition of housekeeping skills, use of household appliances without outside participation;
- diet therapy – balanced nutrition optimized for the patient’s characteristics.
In some situations, you will need support from chemotherapists and radiologists and diagnostic monitoring.
Today, cancer treatment has reached a new level. The developed unique technique, the degree of effectiveness of which has been proven by more than twenty years of practice, gives hope to many patients. The action of a unique technique used in our clinic by Dr. Borisov, called Selective Chronophototherapy (SPT), which is based on photodynamic therapy, is capable of activating a cascade of biochemical and cellular reactions to regulate the level of immune status indicators, demonstrates excellent results both when used independently and in combination with other methods. This significantly reduces the risk of relapse of cancer and the severity of side effects from cytostatic agents, while enhancing their effect on the affected cells.
Dr. Borisov’s gentle technique can be used repeatedly; a course of treatment is recommended. The number of procedures is regulated by the treatment regimen and achievement of the desired result.
We recommend taking VIALIFE capsules or VIALIFE solution, because they contain the highest possible concentration of chlorophyll, which:
- strengthens the immune system;
- enhances cell regeneration;
- saturates tissues with oxygen;
- has antioxidant, anti-inflammatory, detoxifying effects.
Rehabilitation after surgery to remove a tumor in Israel - main approaches
Depending on the type and size of the removed tumor, its location, and the extent of surgical intervention performed, rehabilitation measures may vary.
At the first stages of postoperative rehabilitation, doctors face two main tasks - successful healing of tissue in the operated area and pain relief. Over the course of several days, fluid is released from the wound, which is drained out through drainage tubes. After the fluid stops secreting, the drainage is removed. To relieve pain, the patient is prescribed analgesic drugs.
At subsequent stages of rehabilitation, physiotherapy is carried out. The physiotherapist teaches the patient exercises aimed at restoring freedom of movement and coordination. A set of exercises is selected individually for each patient. First, the patient performs them together with a physiotherapist, and then independently.
- Strength training and physical therapy . The patient can do exercises with dumbbells and other sports equipment, or use special exercise machines.
- Improving limb mobility - exercises aimed at gradually increasing freedom of movement in the limbs, reducing pain and swelling in them.
- Exercises aimed at restoring coordination. The patient learns to control the balance of his body, trains to stand, sit, walk (with and without support).
In addition to the physiotherapist, other specialists may also be involved in the rehabilitation process.
- An occupational therapist is engaged in the functional and social rehabilitation of the patient, teaches him to independently care for himself in everyday life, helps to restore or acquire skills in housekeeping and work activities.
- A psychologist conducts classes with patients who are depressed or worried about their state of mind, helps them cope with psychological problems and acquire a positive attitude.
- The massage therapist helps restore freedom of movement in the joints and spine, improve blood supply and elasticity of the muscles, normalize their tone, and increase the overall immunity of the body.
- The reflexologist acts on bioactive points on the patient’s body, thereby stimulating various biological processes. Although reflexology is an alternative medicine, its effectiveness has been repeatedly confirmed in clinical practice.
- A speech therapist helps restore speech skills to patients who have had a brain tumor removed.
- The nutritionist creates a diet optimized for the characteristics of the patient’s condition.
The rehabilitation period after tumor removal in Israel can be significantly reduced through the use of modern methods of hardware physiotherapy.
- Diadynamic therapy – the use of diadynamic therapy devices allows the use of currents of various frequencies to relieve pain and relieve swelling.
- Inductothermy is a method of electrotherapy that has anti-inflammatory and analgesic effects. When performing inductothermy, the recovering tissues are warmed up and their blood supply improves.
- Laser therapy is the use of low-energy laser systems to improve metabolism in tissues and organs and activate regenerative processes in them.
- Electrophoresis is the introduction of drugs into the body through an electric field. Electrophoresis makes it possible to use small doses of the drug, ensure the duration of its action, and create a high local concentration of the drug in the recovering tissues.
- Magnetotherapy is the effect of an alternating magnetic field on the entire body or its individual parts. Magnetotherapy has a wide range of effects and allows you to stimulate metabolic processes and influence the nervous, endocrine, and lymphatic systems.
- UHF therapy - the use of an ultra-high frequency electromagnetic field, allows to cause the effect of heat generation in tissues, remove inflammatory processes, stimulate cell proliferation, relieve spasms of smooth muscle tissue, and activate regeneration.
- Ultrasound therapy: thanks to the influence of ultrasound, redox processes in the patient’s tissues are accelerated, and the biosynthesis of various neurotransmitters is enhanced. The ultrasound therapy devices used in our clinic can provide an anti-inflammatory and antispasmodic effect, improve tissue nutrition, and stimulate blood circulation in them.
Rehabilitation goals
The objectives of the program include preventing metastasis and relapse of cancer, reviving lost functions, and activating thought processes. Fortunately, the human brain has great potential for recovery if its structures are not permanently damaged. For example, a violation of the part of the cortex responsible for speech is compensated by training fine motor skills. At the time of brain regeneration, growth factors are produced, which not only recreate damaged fragments, but also stimulate the growth of new ones. Therefore, the main mission of neurorehabilitation is to provide the brain with external stimuli and appropriate medical support.
Cognitive rehabilitation is aimed at renewing conversation skills, long-term and short-term memory, and the ability to concentrate and maintain attention. For this, nootropic drugs are used in conjunction with gaming techniques (putting words together from puzzles, writing diaries). If complete restoration of functions is impossible, every effort must be made to adapt the person to the limitations that have arisen, which will make his life much easier.
Physical activity
In the first postoperative days, light breathing exercises are performed to prevent hospital-acquired pneumonia, blood clots and other complications associated with physical inactivity. After the patient is transferred from intensive care and the condition is stabilized, attention is paid to restoring lost movements. If there are no contraindications, you are allowed to stand on your feet and try to walk. Then additional devices are added - weights, balls. Exercises should be performed without pain or fatigue.
It is important to constantly emphasize and praise patients in order to motivate them to achieve new successes, since most of them are prone to denial and depression. Positive dynamics will make it possible to understand that life is not over and a return to the previous existence is quite achievable.
Doctors at Doctor Borisov's Clinic provide assistance to people with disabilities of varying degrees of complexity. This is a difficult period both for those undergoing surgery and for their family members. But you need to be prepared for the fact that it will take a lot of time for a complete recovery or it will be impossible to achieve the previous level of condition. Our specialists try to do everything to get the most positive results. We invite you to a free initial consultation, where we can get acquainted with your problem and together find ways to solve it.
Read also
Consequences of traumatic injuries to the skull, spine, brain and spinal cord
Traumatic brain injuries, or traumatic brain injuries, are damage to the brain that impair brain function.
Brain injuries are divided into two large groups - closed… Read more
Myasthenia gravis
MYASTHENIAS – a disease associated with a disruption of the immune system, as a result of which antibodies are produced against the body’s own tissues involved in the transmission of nerve impulses, which...
More details
Fainting
The term “fainting” (syncope, syncope) comes from the Greek word syncope, which means “to interrupt”, “to turn off”. Fainting is a spontaneous loss of consciousness with a rapid onset associated with a decrease in...
More details
Multiple sclerosis
Multiple sclerosis (MS) is a chronic disease, contrary to popular belief, completely unrelated to attention disorders and senile sclerosis. In this case, the term “sclerosis” means...
More details
Herpes zoster
Varicella zoster first enters the human body at an early age and manifests itself as chickenpox, most often in children. Then follows the latent phase of circulation of the pathogen in the body and under certain conditions...
More details