The problem of vascular diseases of the brain is socially significant. The main cause of cerebrovascular pathology (from initial signs of cerebrovascular insufficiency to strokes) remains arterial hypertension and atherosclerosis. Yusupov's disease neurologists diagnose cerebral ischemia, ACA hypoplasia and asymmetry of cerebral blood flow using the latest equipment from the world's leading manufacturers.
Doctors at the neurology clinic use the latest medications to treat patients. With ischemia in the area of the ACA basin, the duration of recovery depends on the degree of disruption of the blood supply to the brain and the adequacy of rehabilitation measures. Rehabilitation clinic specialists use physiotherapeutic procedures, massage, acupuncture, and alternative methods of restorative therapy to restore blood flow through the PMA.
Asymmetry of blood flow in the MCA and ACA can result in ischemic stroke. At the Yusupov Hospital, complex therapy for pathology is carried out, as a result of which blood flow is restored and the brain tissue receives a sufficient amount of nutrients and oxygen. Severe cases of ischemia in the ACA basin are discussed at a meeting of the Expert Council with the participation of professors and doctors of the highest category. Leading neurologists are collectively developing tactics for managing patients with circulatory disorders due to ACA hypoplasia. The medical staff is attentive to the wishes of patients.
Segments
What is PMA of the brain? ACA stands for anterior cerebral artery in medicine. The blood supply to the brain is quite complex. Blood enters the brain through two internal carotid and two vertebral arteries. The carotid arteries form the carotid basin. They begin in the chest cavity: the right one from the brachiocephalic trunk, the left one from the aortic arch. The vertebral arteries form the vertebrobasilar basin. Through them, blood flows into the vessels that provide nutrition to the medulla oblongata, cervical spinal cord and cerebellum. As a result of fusion, the vertebral arteries form the main basilar artery.
The ACA (anterior cerebral artery) begins at the site where the internal carotid artery divides into its terminal branches. At the beginning of its journey, it gives off a number of small branches that penetrate through the anterior perforated substance to the basal nuclei of the base of the cerebrum. At the level of the optic chiasm, the anterior cerebral artery forms an anastomosis (ostium) with the artery of the same name on the opposite side through the anterior communicating artery.
Hypoplasia of the ACA
The cause of sudden blockage of a cerebral vessel is often an abnormal decrease in its lumen. The reason for this is not cholesterol plaques, but hypoplasia of the cerebral artery - a pathological narrowing of the vessel. The disease is observed in 80% of older people. In addition to their congenital defect, age-related changes in blood vessels are added.
PMA hypoplasia – what is it and how does it manifest? ACA hypoplasia manifests itself in insufficient development of the right cerebral artery. The vessel has an abnormal shape. With this pathology, the structure of the blood vessels supplying intracranial structures may be disrupted. ACA hypoplasia is a congenital pathology that occurs in utero. With hypoplasia of the ACA, the nutrition of the cerebellum, brainstem and occipital lobes is disrupted. As a result of the pathology, the risk of aneurysm formation or stroke increases. Hypoplasia of the ACA is a dangerous condition, to which neurologists at the Yusupov Hospital and neurosurgeons at partner clinics pay special attention.
Causes, symptoms and treatment
The process of formation of cerebral arteries, including the ACA, is negatively affected by the following factors:
- Drug or alcohol addiction in a pregnant woman;
- Infection of the fetus during intrauterine development;
- Intoxication of a woman’s body during gestation;
- Burdened heredity;
- Pregnant women taking medications that have a teratogenic effect.
Symptoms of the disease and their severity depend on the degree of underdevelopment of the vessel that supplies the brain. Symptoms may present differently in each patient. Some people only find out that they have hypoplastic ACA during a medical examination. Often the disease is asymptomatic.
Hypoplasia of the PMA can manifest itself with the following symptoms:
- Headaches of varying intensity;
- Frequent dizziness;
- Decreased or loss of sensitivity of the skin;
- Instability of blood pressure;
- Emotional disorders;
- Disorders of perception and sensations.
All of the listed symptoms indicate insufficient cerebral circulation, so if they occur, contact the neurologists of the Yusupov Hospital. Doctors will first conduct a comprehensive examination, which includes the following diagnostic procedures:
- Ultrasound examination and Dopplerography of cerebral vessels;
- Contrast angiography;
- Computed or magnetic resonance imaging.
Sonologists use modern ultrasound machines that combine a triplex scanner and a Doppler unit. They make it possible to visualize the extracranial and intracranial sections of the arteries of the vertebral-basilar region and identify the asymmetry of blood flow in the MCA and ACA. To determine the state of neurons during cerebral ischemia, magnetic resonance and computed tomography are performed using premium devices. CT angiography of cerebral vessels at the Yusupov Hospital is performed on a modern scanner. Using it, not only step-by-step images of cerebral vessels are obtained, but also their three-dimensional model. These images can be viewed on a computer monitor, printed on film, or transferred to a DVD+R disc.
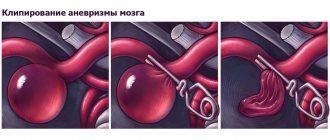
If the symptoms of cerebrovascular accident caused by dysplasia of the ACA are mild, therapy is carried out with drugs that dilate the arteries and normalize cerebral blood flow. Conservative therapy helps reduce the intensity of headaches and improve the functioning of the vestibular apparatus. When a blood clot is detected in an abnormal vessel, the doctor prescribes medications to dissolve it. Neurosurgeons at partner clinics of the Yusupov Hospital carry out correction of the pathology of the ACA in cases where there is no positive dynamics with drug treatment. The stenting technique is mainly used for ACA hypoplasia.
Signs and symptoms of vertebral artery hypoplasia
The clinical picture can begin to form at any age. Often a predisposing factor for this is cervical osteochondrosis or poor posture. After the next attack of exacerbation, the patient begins to feel headaches, absent-mindedness, decreased ability to concentrate, drowsiness, increased or decreased blood pressure.
In older age, the trigger is the deposition of cholesterol on the inner wall of the cerebral blood vessel. It narrows and loses its functional capacity. In such situations, among the patients' complaints, various tinnitus, dizziness, pain in the back of the head, disturbed night sleep, and depression come to the fore.
There are no signs of vertebral artery hypoplasia that would help distinguish left-sided pathology from right-sided localization. Both forms of the disease proceed in exactly the same way. Differences may appear in the case of a pronounced narrowing of the internal lumen of the blood vessel. Visual acuity in the left or right eye may sharply decrease, hearing in one ear may deteriorate, noise may appear in one ear, etc.
An experienced neurologist asks the patient to take a few steps forward with his eyes closed. If the movement trajectory deviates to one side or the other, vascular pathology can be diagnosed in the left or right hemisphere. The fact is that the vertebral arteries are responsible for the blood supply to the vestibular apparatus. This structure provides balance when walking upright. If the blood supply is impaired, the patient begins to deviate to the left or right when walking.
The first signs of vertebral artery hypoplasia may appear some time after serious deformation of the blood vessel. Typically, pronounced clinical symptoms of vertebral artery hypoplasia appear in people over 40 years of age. At a younger age, signs may appear against the background of degenerative dystrophic damage to the cartilage tissue of the intervertebral discs.
It is worth paying attention to the following negative manifestations of the disease:
- orthostatic dizziness (when suddenly rising to your feet from a sitting or lying position);
- dysfunction of the vestibular apparatus (expressed in the fact that it is difficult to maintain balance);
- muscle weakness, fatigue;
- decreased general and mental performance;
- frequent depression;
- sleep disorders;
- severe headaches in the morning.
With a long course of the disease, a person develops irritability, lack of interest in the world around him, and constant apathy. A persistent increase in blood pressure that cannot be corrected with antihypertensive pharmacological drugs is another pronounced clinical sign. A comprehensive diagnosis is required - duplex scanning of cerebral blood vessels.
Cerebral vasospasm
Elderly people, middle-aged and brain-aged people are often bothered by headaches, noise and dizziness, increased fatigue, memory impairment, and decreased performance. Often patients do not take such complaints very seriously. Meanwhile, these may be signs of vasospasm in the left cerebral arteries, MCA (middle cerebral artery) and ACA (anterior cerebral artery). Cerebral vasospasm (narrowing of the lumen of the arteries at the base of the brain after subarachnoid hemorrhage due to rupture of a saccular aneurysm) can secondary cause cerebral ischemia.
After an aneurysm ruptures, the patient experiences a temporary period of improvement or stabilization until symptomatic vasospasm occurs. Neurological symptoms of cerebral spasm from the fourth to the fourteenth day after the first rupture of the aneurysm. The resulting neurological symptoms correspond to cerebral ischemia in specific arterial territories. The severity of cerebral vasospasm determines the likelihood of developing cerebral ischemia and infarction.
Signs of vasospasm in the left arteries of the brain, MCA and ACA often occur in those patients in whom early magnetic resonance or computed tomography of the brain showed layers of coagulated blood 1 mm thick or more in the sulci of the brain or spherical blood clots larger than 5 mm3 in the basal cisterns.
Doctors at the Yusupov Hospital determine the localization and severity of vasospasm in the ACA and MCA using magnetic resonance or computed tomography. To ensure an accurate prognosis, a CT scan of the brain is performed between 24 and 96 hours after subarachnoid hemorrhage.
Clinically pronounced cerebral vasospasm is manifested by symptoms that relate to one or another pool of blood supply to the brain of a certain artery. When the trunk or main branches of the middle cerebral artery (MCA) are involved, the patient develops the following symptoms:
- Contralateral hemiparesis - weakness of the muscles of half the body on the side opposite to the intracerebral hemorrhage;
- Dysphasia is a speech disorder due to spasm of the arteries of the dominant hemisphere of the brain;
- Anosognosia, apraktoagnosia - a recognition disorder due to spasm of the arteries of the non-dominant hemisphere of the brain.
Signs of vasospasm in the left cerebral arteries, MCA and ACA may not be pronounced due to the fact that collateral blood flow is formed in the brain through fusion of areas of adjacent cerebral blood supply.
Ischemia due to vasospasm of the ACA is manifested by abulia. The patient is awake, lies with his eyes closed or open, and responds to instructions with a delay. He cannot actively conduct a conversation, but answers questions with short phrases that he pronounces in a whisper, chews food for a long time and often holds it between his gums and cheek. All focal neurological symptoms resulting from cerebral vasospasm in patients may occur suddenly, reaching maximum severity within a few minutes, or develop over several days.
If the entire brain area in the MCA basin (middle cerebral artery) is subject to ischemia or infarction, its edema develops, which can lead to increased intracranial pressure. Early magnetic resonance or computed tomography of the brain can predict an unfavorable outcome if a large blood clot is detected in the Sylvian cistern or in the lumen of the Sylvian fissure and a second significant clot in the basal frontal fissure, located between the cerebral hemispheres. The simultaneous presence of clotted blood in these areas is combined with severe symptomatic spasm of the MCA and ACA. In such a situation, superficial collaterals in the cerebral cortex from the ACA are not able to compensate for ischemia in the MCA territory.
If spasm of the cerebral arteries occurs against the background of subarachnoid hemorrhage, drug prevention and treatment are ineffective.
Because patients with cerebral vasospasm have increased blood volume and swelling of the brain parenchyma, even the small increase in intracranial volume that occurs with vasodilator exposure can aggravate neurological disorders. If a patient has severe symptomatic cerebral vasospasm, neurologists do not prescribe vasodilators.
All efforts of doctors are aimed at increasing cerebral perfusion pressure by increasing mean arterial pressure. This is achieved by increasing plasma volume and prescribing vasopressor drugs (phenylephrine, dopamine). Since treatment aimed at increasing perfusion pressure leads to an improvement in the picture of the neurological status in some patients, but high blood pressure is associated with the risk of recurrent hemorrhage, when using this method of treatment, neurologists at the Yusupov Hospital determine cerebral perfusion pressure and cardiac output, and conduct a direct study of the central venous pressure. In severe cases, the patient's intracranial pressure and pulmonary artery wedge pressure are measured.
Administration of the osmotic diuretic mannitol, while maintaining adequate intravascular volume and mean arterial pressure, increases the patient's serum osmolarity. In severe cases, barbiturate coma is used to reduce intracranial pressure.
Types of brain malformations
There are many similar anomalies. Among them there are both very rare and more common diseases. Common developmental defects include:
- micro- and macrocephaly - decrease and increase in the size and mass of the brain, respectively;
- anencephaly - its complete absence;
- agyria - absence of convolutions of the cerebral cortex;
- holoprosencephaly - absence of the central sulcus, which divides the brain into two hemispheres;
- underdevelopment of the corpus callosum.
These disorders are accompanied by various disorders of the psychoemotional sphere, speech, motor functions, and in severe cases can lead to death. Some disorders respond well to correction, while others remain with the patient for life.