How to treat dyscirculatory encephalopathy of the brain
Discirculatory encephalopathy is a chronic damage to the nervous tissue of the brain, the cause of which is a circulatory disorder.
This is a progressive pathology. Irreversible changes in the brain lead not only to instability of the emotional state and changes in behavior (thinking), but in some cases to loss of ability to work and the inability to perform usual everyday tasks. We will talk further about how to treat dyscirculatory encephalopathy of the brain. Types of disease:
- atherosclerotic;
- hypertensive;
- venous;
- mixed.
Based on the nature of the course, discirculatory encephalopathy (DEP) can be classic (sluggish), remitting with a gradual increase in symptoms, and progressive. The main causes of the disease, according to experts, are hypertension and atherosclerosis. Important: medications for dyscirculatory hypertensive encephalopathy will help improve metabolism and blood supply to the brain.
How to treat
For grade 2 DEP, treatment is selected taking into account the individual characteristics of the body. At this stage of the disease, patients may be unable to follow the doctor's orders, so they need help from relatives.
Non-drug therapy
Physiotherapeutic procedures help improve blood circulation in the head and neck areas. Depending on the causes of the disease, the following are used:
- electrosleep;
- exposure to galvanic currents;
- shock wave therapy;
- laser exposure.
Doctors recommend reconsidering your lifestyle. The patient’s recovery is accelerated by the following measures:
- exclusion of stressful and conflict situations;
- regular walks in the fresh air;
- introduction to a regime of light physical activity (the neurologist selects a set of exercises that need to be performed daily);
- quitting smoking and drinking alcohol;
- normalization of body weight.
Drug treatment
The following drugs are used to eliminate the causes and symptoms of the disease:
- Nootropics (Nootropil, Piracetam). The drugs in this group normalize blood circulation, restore connections between neurons, and increase the brain’s resistance to hypoxia.
- Metabolic stimulants (Cerebrolysin). Restore the processes of transporting nutrients to the nervous system.
- Neuroprotectors (Gliatilin). Prevents the destruction of nerve cells, slowing the development of encephalopathy.
- Statins (Lovastatin). Prescribed for cerebral atherosclerosis. The drugs reduce the level of low-density lipoproteins, suppressing the formation of cholesterol plaques.
- ACE inhibitors (Fosinopril). Used for encephalopathy of hypertensive origin. Taking the pills regularly helps maintain blood pressure within normal limits.
- Antiplatelet agents (Dipyridamole). Prescribed in the presence of blood clots in the cerebral and carotid arteries.
- Antihyperglycemic agents (Metformin). Used for diabetic discirculatory encephalopathy.
- Glucocorticoids (Prednisolone). Indicated for patients with inflammatory vascular diseases.
Folk remedies
The following folk recipes are used to treat the disease:
- Hawthorn infusion. The product helps strengthen blood vessels, get rid of headaches and dizziness. To prepare the infusion 2 tbsp. l. pour 0.5 liters of boiling water over the berries and leave overnight. The finished product is taken 50 ml 3 times a day.
- Clover infusion. Helps with tinnitus, which often occurs against the background of encephalopathy. 50 g of flowers are placed in a thermos and filled with 300 ml of hot water. The product is infused for 2 hours, filtered and consumed 100 ml before each meal.
- Rose hip. The berries are used to prepare a decoction. 100 g of fruits are poured into 1 liter of water and boiled for 15 minutes. Before use, the decoction is diluted with water.
- A collection of chamomile, valerian root and lemon zest. The ingredients are mixed in equal proportions. 1 tbsp. l. The collection is brewed in a glass of boiling water. After half an hour, the infusion is filtered. The product is taken 200 ml in the morning and evening.
Important information: How to treat von Willebrand-Diana disease
Diet
A special diet increases the effectiveness of medications and prevents recurrence of the disease. It is necessary to avoid foods that contribute to the development of atherosclerosis. The list of prohibited products includes:
- fatty and fried foods;
- alcohol;
- strong tea and coffee;
- sweet carbonated drinks;
- semi-finished products;
- fatty meat and dairy products.
The diet includes fresh vegetables and fruits, onions and garlic, dietary meat, herbs, and seafood.
Who's at risk
It was previously thought that older people were more susceptible to DEP. Currently, the disease has become significantly “younger” and quite often it is diagnosed in patients who are under 50 years of age. In most cases, these are people of creative professions and mental work. The most severe consequences of discirculatory encephalopathy include senile dementia and ischemic stroke.
Factors that provoke the disease are: poor diet with a predominance of fatty and smoked foods, alcohol abuse, smoking, excess weight, hormonal disorders, high blood pressure, head injuries.
What it is
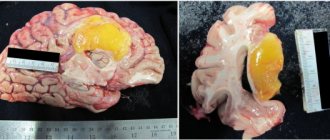
Discirculatory encephalopathy of the 2nd degree is a pathology, with the progression of which accelerated damage to all brain tissues is observed. This occurs due to a decrease in the functioning of blood vessels. Therefore, in certain areas of the brain, gradual tissue death begins to occur, which covers increasingly larger areas.
Neighboring areas of the brain begin to take on additional functions. If no treatment is carried out, then such connections will not be able to build. The quality of life gradually decreases; the patient feels unwell all the time and cannot work or rest normally. Often patients are assigned a disability. In total, there are 3 stages of the disease:
- First
The changes that occur in the brain are minor, but characteristic symptoms are observed. At this stage, the disease is easily confused with other pathologies of the central nervous system. Patients complain of decreased performance, constant fatigue and drowsiness.
Headaches and constant tinnitus may occur. It becomes difficult for patients to fall asleep, causeless nervousness and depressive moods, and depressive states are increasingly occurring.
- Second
In some cases, it is not distinguished from the first stage. This happens in cases where characteristic symptoms persist for six months. At this stage, there is a progression of negative manifestations of the disease.
Functional disorders of the brain are clearly noticeable, but the patient can still take care of himself and does not need constant monitoring.
- Third
At this stage, changes in grade 2 DEP are irreversible and pronounced. The patient requires care and control, since he cannot take care of himself, and his actions pose a danger to others.
At this stage, disability is usually assigned, and therapeutic treatment is aimed at prolonging life, but its quality does not improve.
Life expectancy with dyscirculatory encephalopathy stage 2. depends not only on the speed and quality of the treatment, but also on the health status and individual characteristics of the patient.
The disease, diagnosed at a young age, develops rapidly, but is also quickly cured. In elderly patients, the disease develops slowly, but leads to disability in the vast majority of cases.
Causes of dyscirculatory encephalopathy
Atherosclerosis. Metabolic disorders lead to a decrease in the lumen of blood vessels, as a result of which the brain does not receive the required amount of oxygen and nutrients. Signs of discirculatory atherosclerotic encephalopathy:
- High blood pressure (hypertension) and low blood pressure (hypotension): in the first case, the vessels are excessively filled with blood, and insufficient filling is a consequence of hypotension.
- Osteocondritis of the spine. As a result of compression of the artery, the brain does not receive the amount of nutrients it needs.
- Injuries to the head and spine can cause hematomas that compress blood vessels, disrupting the nutrition of nerve cells.
- Smoking causes a narrowing of blood vessels, especially capillaries.
- Congenital pathologies.
- Vascular diseases.
- Hormonal disorders.
Symptoms of dyscirculatory encephalopathy of the brain, stage 1
The stage is characterized by a gradual increase in symptoms. Obvious manifestations of the disease are complaints of mood instability (from complete depression to sudden joy), apathy and depression. Unreasonable crying, headache, sleep disturbances, forgetfulness and attacks of aggression towards others are symptoms of stage 1 DEP of the brain. In some cases, patients may experience minor pain in the joints, back and stomach area.
On our website Dobrobut.com you will find more detailed information on this issue. You can make an appointment for a consultation by calling the numbers listed on the pages. At a personal appointment, the doctor will answer all questions and talk about the treatment of dyscirculatory encephalopathy of the 2nd degree of mixed origin.
Diagnostics
To identify dyscirculatory encephalopathy stage 2, the following diagnostic procedures are used:
- Examination of the patient. The doctor pays attention to the condition of the skin and the presence of tendon reflexes. Using special tests, a neurologist identifies impaired coordination of movements, memory impairment and decreased intellectual abilities.
- Rheoencephalography. A safe and painless diagnostic procedure allows you to assess the condition of blood vessels and the bioelectrical activity of the brain. An important role in making a diagnosis is played by determining the tone and blood supply of the arteries.
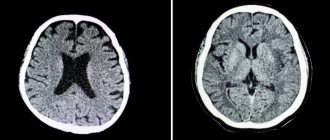
- CT scan. A non-invasive research method allows you to obtain information about the state of brain tissue. CT can detect tumors, thrombosis, and ischemic lesions.
- Doppler ultrasound examination of the vessels of the head and neck areas. Helps determine the speed of blood flow in veins and arteries.
- Neuropsychological research. It is considered the main method for assessing the patient's mental state. During the procedure, a violation of the higher functions of the nervous system is detected.
Important information: How to treat marble disease (deadly marble disease) in children and symptoms of osteopetrosis
Discirculatory encephalopathy 2nd degree - clinical manifestations
Without proper treatment, DEP of the 1st degree progresses to the second with all the ensuing consequences. Symptoms of grade 1 dyscirculatory encephalopathy of the brain include attention and memory disorders, and spatial orientation is disturbed. Complete apathy towards the outside world appears. In some cases, loss of ability to work may occur.
Stage 3 DEP is a severe degree of the disease, in which the patient loses the ability to perform purposeful actions and needs constant care. Characteristic manifestations are disturbances in speech and pelvic organ function, seizures, and movement disorders. The patient receives disability due to the diagnosis of dyscirculatory encephalopathy of the 3rd degree.
Causes
The diagnosis of stage 2 DEP is a disease that belongs to the group of cerebrovascular diseases (CVD), which indicates a decisive role in the pathogenesis of vascular pathologies. Among the common causes of dyscirculatory encephalopathy stage 2, it is worth noting thrombosis of arteries and veins, atherosclerosis, pathologies of the main cerebral arteries, accompanied by stenosis (persistent narrowing of the vascular lumen).
Violation of neurohumoral regulation, weakening of the tone of the walls of veins and arteries, blockage of blood vessels cause a deterioration in the blood supply to the brain structures. The result of insufficient blood flow is ischemic processes. Risk factors for developing stage 2 DEP:
- Arterial hypertension occurring in a chronic form.
- Arterial hypotension, long-term.
- Hypercholesterolemia (persistent increase in blood cholesterol levels).
- Atrial fibrillation (scattered, uncoordinated contraction).
- Diabetes.
- Ischemic heart damage.
- History of myocardial infarction.
- Hyperhomocysteinemia (increased blood levels of homocysteine, a non-protein sulfhydryl amino acid).
- Violation of hemostasis (self-regulation of the circulatory system - maintaining the liquid state of the blood, stopping bleeding, dissolving blood clots that have clogged the damaged vessel wall).
Grade 2 cerebral encephalopathy often develops as a result of long-term arterial hypertension. Pathogenesis includes several sequential processes and mechanisms:
- Persistent increase in blood pressure values.
- Microangiopathy (damage to small-diameter cerebral arteries).
- Arteriolosclerosis (thickening of the walls of arterioles).
- Lipohyalinosis (vascular protein dystrophy with the replacement of normal tissue of the vascular wall with cartilaginous structures in combination with lipoproteins - complex proteins with a fat fraction in the composition).
- Structural changes in the endothelial layer of the vessel.
- Predisposition to thrombosis.
- Leukoaraiosis (diffuse damage to white matter).
The pathogenesis of stage 2 DEP, which arose as a result of atherosclerotic damage to extracerebral (located outside the brain) and intracerebral (lying inside the brain) vessels, suggests a sequence of pathological processes and conditions:
- Episodes of acute ischemia, manifested in the form of transient ischemic attacks and ischemic strokes.
- Progression of atherosclerotic encephalopathy without the development of strokes.
- Deterioration of cerebral blood flow due to microembolism - the appearance and circulation in the bloodstream of foreign microparticles detached from the atherosclerotic plaque. The pathological process provokes blockage of small-diameter vessels, which leads to disruption of the local blood supply.
Risk factors for the development of microembolism include increased blood viscosity, activation of blood clot formation processes, and an increase in the ability of platelets to aggregate (attach). Discirculatory encephalopathy of the 2nd degree of mixed origin is a form of pathology that develops as a result of several pathogenetic factors, which necessitates a careful differential diagnosis.
Treatment of DEP
The main goal of drug therapy is to restore vascular function, improve blood flow to the brain and normalize the functioning of the nervous system. For this purpose, the patient is prescribed beta-blockers, calcium antagonists, vasodilators, neuroprotectors, and anticoagulants. This is general therapy. Symptomatic treatment is aimed at eliminating individual clinical manifestations, namely depression and behavioral lability.
Surgical intervention is recommended for severe progressive DEP (the degree of vasoconstriction is more than 70%).
Treatment methods
The doctor will tell you how to treat the disease, based on the results of a physical examination and diagnostic examination. Discirculatory encephalopathy of the 2nd degree belongs to the group of CVD (cerebrovascular diseases), which determines the nature of treatment. Therapy is carried out comprehensively and is focused on the primary disease of the vascular system. Main objectives of treatment:
- Preventing recurrent disruption of blood flow in brain tissue.
- Restoration of cerebral circulation.
- Normalization of functional brain activity.
Correction of blood pressure indicators is one of the primary directions of therapy. Stabilization of blood pressure values prevents the progression of cerebrovascular diseases. The treatment program includes medications and non-drug measures. The main directions of non-drug treatment:
- Correction of body weight.
- Limiting salt intake.
- Getting enough important microelements from food.
- Quitting bad habits (drinking alcohol, smoking).
- Dosed physical activity.
The disease, which occurs in stage 2, must be treated with medications. Drug and non-drug prevention of stroke development is of great importance.
In complex therapy, drugs are used that stimulate cellular metabolism, improve blood supply to brain tissue, and prevent damage to neurons. Treatment of grade 2 dyscirculatory encephalopathy involves taking medications that stabilize blood pressure:
- ACE inhibitors (angiotensin-converting enzyme).
- Beta blockers.
- Angiotensin receptor blockers.
- Calcium channel blockers.
- Diuretics.
Statistics show that normalizing blood pressure slows down the progression of pathology by 40%. In the absence of pronounced stenosis and occlusion of the carotid arteries, the doctor strives to achieve normal values.
In case of carotid artery stenosis, normalization of blood pressure values is ineffective. If hypercholesterolemia is detected, statins are prescribed, which normalize the level of lipids in the blood. With long-term use of statins, complete regression of atherosclerotic plaques is often observed.
Long-term use of thrombolytics reduces the risk of stroke by 30%. Nootropic agents that improve the transmission of nerve impulses and neuroprotectors that protect neurons from damage and slow down the development of cerebrovascular insufficiency are indicated. Taking medications must be combined with non-drug treatments. Nutrition should be complete and balanced, including foods recommended by the doctor.
How long can you live with dyscirculatory encephalopathy of complex origin?
There is no clear answer. It all depends on the degree of the disease, symptoms, drug therapy, etc. The prognosis is favorable if DEP is detected early. Timely treatment and strict adherence to the doctor’s recommendations will help slow down the development of pathology, and in some cases, stop it.
If you are interested in the question of how long you can live with discirculatory encephalopathy of complex origin, make an appointment with our specialist.
Related services: Computed tomography Encephalogram of the brain
Symptoms of pathology
The pathology is characterized by an increase in neurological symptoms, which is associated with the aggravation and spread of destructive processes in the nervous tissue. Symptoms of dyscirculatory encephalopathy grade 2:
- Cephalgic syndrome. Pain in the head area is usually throbbing, intense, irregular, and is often accompanied by nausea and tinnitus.
- Dizziness, transient, short-term confusion.
- Deterioration of cognitive abilities (memory, mental activity).
- Decreased performance, increased fatigue.
- Sudden mood swings (emotional lability).
- Sleep disorder.
Discirculatory encephalopathy of the 1st degree can be asymptomatic or manifest itself with subtle signs. With grade 2 DEP, the symptoms are clearly visible; determining the pathology of this stage suggests the need for drug treatment. Signs of neurological disorders depend on the stage (degree) of the disease:
- 1st degree (compensation stage). Compensation mechanisms restore balance and normal activity of brain structures. The disease does not manifest itself with severe symptoms. Typical symptoms for this stage are asthenia, anxiety, development of depression and phobias. Neurological disorders are manifested by anisoreflexia, motor coordination disorder, visual dysfunction, and oral automatism.
- 2nd degree (stage of subcompensation - pronounced clinical symptoms gradually increase due to the worsening of pathological processes and weakening of compensation mechanisms). Focal neurological symptoms are partially reversible. When 1-2 lesions form, damage to the pyramidal system is observed with the development of motor (fine motor skills, complex movements) disorders. Other typical signs: ataxia (inconsistency of movements), amyostatic syndrome (limited range of motion, slow motor activity), cranial nerve paresis.
- 3rd degree (stage of decompensation - pronounced disorders that are not amenable to the mechanisms of natural self-regulation). There is a severe neurological deficit - severe ataxia, amyostatic disorders (slowdown and reduction in the volume of motor activity), paresis and paralysis, pseudobulbar and bulbar disorders (dysarthria - speech impairment, dysphonia - change in the quality characteristics of the voice, dysphagia - difficulty swallowing), caused by damage and interruption of cortico-nuclear pathways. Paroxysmal conditions (fainting, falling, epileptic seizures) are typical for this stage.
At stage 3 of the pathology, dementia of vascular origin often develops in combination with apraxia (impaired purposeful movements) and agnosia (impaired visual, auditory, tactile perception). Against the background of cognitive impairment, the volume of patient complaints decreases, and the critical assessment of one’s own condition and actions decreases.