The spinal cord plays no less important role in the body than the brain, so disruption of its blood circulation leads to the development of serious complications and unpleasant consequences. The prevalence of spinal stroke, according to statistics, is less than 1% of all neurological disorders, it is less likely to be fatal and equally often affects both male and female sexes. In this case, a spinal cord stroke, if treatment is delayed, can cause permanent disability, loss of motor activity and disruption of the functioning of internal organs.
Causes of spinal stroke
The causes of spinal stroke are usually divided into two main groups: primary and secondary. Primary ones directly depend on the condition of the vessel responsible for feeding a particular segment of the spinal cord: thrombosis, embolism, developmental anomalies, aneurysms, vasculitis, infectious and inflammatory lesions, etc. Secondary ones are caused by the presence of concomitant diseases that affect the functioning of the cardiovascular system: atherosclerosis, hypertension, osteochondrosis, structural anomalies of the vertebrae, blood diseases, hormonal disorders, oncology, etc. Spinal injuries due to aggressive external influences or surgical intervention should be considered separately.
All these reasons lead to disruption of the blood supply to the spinal cord and its individual structures. Metabolic processes occurring in nerve cells are active, so a lack of oxygen and nutrients leads to their irreversible damage and death.
What is a spinal stroke?
This is an acute circulatory disorder of the spinal cord. It can develop due to compression or blockage of an artery, or perhaps due to rupture of blood vessels. In the first case, blood does not flow, in the second, hemorrhage and swelling of soft tissues occurs.
Spinal cord stroke may be associated with:
- with congenital malformations of the spine: arteriovenous malformations, coagulopathies;
- with acquired diseases: vasculitis, aneurysms, atherosclerosis;
- with consequences of a back injury;
- with complications after disc or aortic surgery, with spinal anesthesia or injections.
Therefore, before an epidural puncture, it is recommended to do an MRI of the spine.
Types of spinal stroke and their signs
Circulatory disorders of the spinal cord can occur in hemorrhagic, ischemic and mixed types. Ischemic stroke is more often recorded in people over 50 years of age; it is formed as a result of compression or blockage of a vessel. Symptoms of ischemia increase gradually, long-term consequences become apparent within a week to several months. Focal symptoms depend on the location of the damage and its volume. The most commonly diagnosed symptoms are:
- Weakness in the limbs that goes away on its own;
- Loss of sensitivity in the limbs;
- Pain in the muscle area;
- Urinary disorders;
- Pain in the spine.
There are certain syndromes that can be used to suggest the location of the damaged area. Ischemia of the spinal and vertebral arteries is manifested by bilateral paralysis of the limbs, sensory disturbances, sphincter paresis, and respiratory distress. Damage to the posterior spinal artery is accompanied by disturbances of superficial sensitivity, tremors of the hands, and paresis of the legs. Damage to the vertebral and radicular arteries causes paresthesia, disruption of muscles and joints, and convulsive muscle twitching. Ischemia of the radicular arteries leads to the appearance of girdle pain, changes in temperature sensitivity, increased knee reflexes, decreased abdominal reflexes and other signs.
A hemorrhagic stroke of the spinal cord is formed due to the rupture of a vessel and further hemorrhage under the membranes (hematorachis) or into the brain tissue. When hemorrhaging into the substance of the spinal cord, the patient experiences girdle pain, paralysis of the limbs of varying degrees, sensitivity disorders, and dysfunction of the pelvic organs. Hemorrhage under the membranes is recorded extremely rarely; it is accompanied by sharp pain and symptoms of brain damage, which lasts several days.
If unfavorable symptoms appear, you should immediately consult a doctor, since the outcome and consequences of the disease depend on the speed and quality of care. You can undergo a full examination, comprehensive treatment and rehabilitation at the neurology clinic of the Yusupov Hospital.
Ischemic spinal stroke
Men and women get sick with equal frequency between the ages of 30 and 70 years and older.
The course of the disease can be divided into several stages:
- stage of harbingers (distant and close);
- stage of stroke development;
- stage of reverse development;
- stage of residual effects (if complete recovery has not occurred).
Precursors of ischemic spinal stroke are paroxysms of transient spinal disorders (myelogenous, caudogenic or combined intermittent claudication, transient pain and paresthesia in the spine or in the projection of the branching of certain spinal roots, disorders of the functions of the pelvic organs).
The rate of occurrence of a stroke varies - from sudden (with embolism or traumatic compression of the vessels supplying the spinal cord) to several hours or even days.
It has already been mentioned that spinal infarction is often preceded by pain in the spine or along individual roots.
It is typical for this pain to cease or significantly subside after the development of myelischemia. This occurs due to an interruption in the passage of pain impulses through sensitive conductors at the level of the focus of spinal cord ischemia.
Clinical picture
ischemic spinal stroke is very polymorphic and depends on the extent of ischemia both along the length and across the diameter of the spinal cord. Depending on the extent of ischemia across the diameter of the spinal cord, the following variants of the clinical picture occur.
Ischemia syndrome of the ventral half of the spinal cord
(
anterior spinal artery occlusion syndrome, Preobrazhensky syndrome
).
It is characterized by the acute development of paralysis of the limbs, dissociated paraesthesia, and dysfunction of the pelvic organs. If ischemia is localized in the cervical segments of the spinal cord, paralysis (paresis) develops in the arms, flaccid, in the legs - spastic. Ischemia of the thoracic segments is manifested by lower spastic paraparesis, myelischemia of the lumbosacral localization is manifested by lower flaccid paraparesis. The upper limit of dissociated paranesthesia helps to navigate the extent of the ischemic focus along the length of the spinal cord. Articular-muscular and tactile sensation is not impaired. Ischemia of the lumbosacral thickening is manifested by lower flaccid paraplegia with areflexia, dissociated paraanesthesia, urinary and fecal retention. This symptom complex is called Stanilovsky-Tanon syndrome.
Anterior ischemic poliomyelopathy syndrome
is one of the variants of partial damage to the structures of the ventral half of the spinal cord. It is characterized by the rapid development of flaccid paresis of certain muscle groups of the upper or lower extremities with areflexia and muscle atrophy and changes in EMG indicating ischemia within the anterior horns of the spinal cord. This syndrome has to be differentiated from polio, in which signs of infection and the stage of gastrointestinal disorders are revealed.
Ischemic Brown-Séquard syndrome
Occurs occasionally. It differs from a typical compression lesion of half of the spinal cord in that during ischemia the posterior cords remain preserved, so joint-muscular sensation on the side of the central limb paralysis is not impaired. The anatomical validity of this variant of myelischemia has already been mentioned; it is due to the fact that individual sulcal-commissural arteries supply only one, right or left, half of the diameter of the spinal cord.
Centromedullary ischemia syndrome
It is characterized by acute or subacute development of segmental dissociated anesthesia with the loss of corresponding segmental deep reflexes and mild peripheral paresis of the same myotomes. The clinical picture resembles syringomyelia ( ischemic syringomyelic syndrome
).
Ischemia syndrome of the marginal zone of the anterior and lateral cords
It manifests itself as spastic paresis of the limbs, cerebellar ataxia and mild conductive parahypesthesia. The acute onset of the disease and the subsequent possibility of an intermittent course resemble the spinal form of multiple sclerosis. Diagnosis is aided by monitoring the further development of the disease.
Ischemic amyotrophic lateral sclerosis syndrome
Most often develops in the upper arterial basin of the spinal cord. The clinical picture is characterized by weakness of the distal parts of the upper extremities, atrophy of the small muscles of the hands, increased deep reflexes, and pathological hand and foot signs. Fascicular twitching of the muscles of the shoulder girdle is possible. With this syndrome, there is no spread of paretic phenomena to the bulbar muscle group (tongue, larynx and pharynx).
Ischemia syndrome of the dorsal part of the spinal cord (Williamson syndrome)
It is rare and is associated with occlusion of the posterior spinal artery. In such patients, sensitive ataxia acutely appears in one, two or more limbs, moderate spastic paresis of the same limbs, segmental hypoesthesia indicating the level of ischemia, vibration sensitivity in the legs is lost.
Spinal cord transverse ischemia syndrome
It develops when the large radiculo-medullary artery, which is involved in the formation of both the anterior and posterior spinal arteries, is turned off. Almost always, such a topography of the lesion is observed when the venous outflow from the spinal cord is disrupted (thrombosis or compression of the spinal and radicular veins). Details of the clinical picture vary depending on the level of involvement (cervical, thoracic or lumbar segments).
Knowledge of typical variations in the distribution of the radicular spinal arteries in some cases makes it possible to clinically determine the affected area of such an artery. Let us give a brief clinical picture of myelischemia when individual spinal arteries are switched off.
Occlusion syndrome of the large anterior cervical radiculo-medullary artery (cervical thickening artery)
It manifests itself as flaccid or mixed paresis of the upper extremities and spastic lower extremities, segmental and conduction sensitivity disorders, dysfunction of the pelvic organs of the central type.
When turning off the superior accessory radiculo-medullary artery
lower paraparesis and dissociated paraesthesia with an upper border on the ThI-LIV segments develop acutely. Urinary retention occurs. Initially, the knee and Achilles reflexes usually fade. However, Babinski's sign is always caused. Over the next 5-6 days, lower paraparesis acquires the features of central paraparesis (muscle tone increases, deep reflexes are revived). Sensory disorders are usually concentrated in the area of the upper thoracic dermatomes. In the residual stage, along with signs of damage to the ThI-ThIV segments, extinction of deep reflexes in the hands and wasting of small muscles of the hands are sometimes observed. Mild signs of peripheral motor neuron damage are confirmed by electromyography. These symptoms can be considered as distant symptoms.
Adamkiewicz artery shutdown syndrome (lumbar enlargement artery)
The clinical picture can be quite varied. It depends on the stage of the disease. In the acute phase of a stroke, flaccid lower paraparesis (paraplegia), dissociated or rarely total paraanesthesia with an upper limit varying from the ThI-SI segment is always detected. The function of the pelvic organs (incontinence or retention of urine and feces) always suffers. Bedsores often quickly develop.
Treatment of spinal stroke
Treatment of a spinal stroke involves a set of measures that depend on the type of injury, the symptoms caused, the patient’s age and his individual characteristics. Treatment of patients at the Yusupov Hospital is carried out in stages; for ischemic types of lesions, therapy is aimed at normalizing the rheological properties of the blood, dissolving blood clots, eliminating vasospasm and swelling of brain tissue. After the acute period, rehabilitation measures are prescribed that help eliminate the consequences and restore lost functions. According to indications, surgical intervention is performed after consultation with a neurosurgeon. Therapy for hemorrhagic stroke of the spinal cord at the Yusupov Hospital is aimed at relieving swelling, stopping bleeding, restoring blood supply and returning lost functions.
Neurologists at the Yusupov Hospital create comprehensive individual treatment and rehabilitation programs for each individual patient, which allows them to reduce the degree of disorders caused, prevent serious consequences, improve the quality of life, and return a person to a full life. You can make an appointment with a doctor and find out detailed information about treatment and rehabilitation by phone.
Spinal cord infarction (spinal stroke)
Spinal cord infarction is rare in clinical practice. It is usually the result of atherosclerosis or dissecting aortic aneurysm, rather than damage to the spinal cord's own arteries. Spinal cord ischemia is often the result of surgery on the aorta or cardiogenic embolism. Sometimes spinal infarction is associated with vasculitis or neurosyphilis. With systemic arterial hypotension, especially in patients with atherosclerosis of the aorta and its main branches, parts of the spinal cord located on the border of the vascular territories and most sensitive to ischemia may be affected, which is manifested by the development of paresis, sometimes mixed, without impaired sensitivity and resembles the picture of ALS. You should always remember that impaired circulation of the spinal cord may be a consequence of compression of the spinal vessels by a tumor or other space-occupying formation.
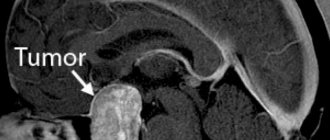
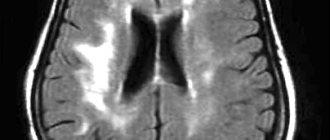
Symptoms usually develop acutely with sudden back pain, sometimes with radicular irradiation, against which bilateral paralysis, impaired superficial (pain and temperature) sensitivity below the level of the lesion, and pelvic disorders are manifested. Since infarction most often occurs in the area supplied by the anterior spinal artery, deep types of sensitivity that conduct the posterior columns remain intact. When the penetrating branch of the spinal artery is damaged, the infarction develops on only one side, which is manifested by monoplegia or hemiplegia on the affected side and impaired superficial sensitivity on the opposite side. Sometimes the onset may be more gradual, with neurological impairment progressing over several hours. Differential diagnosis is made with transverse myelitis, compression of the spinal cord. Spinal infarction may be supported by the acute development of the disease (without previous symptoms), the absence of damage to the posterior columns, the presence of a clear level of damage, and signs of systemic vascular disease. Diagnosis is facilitated by myelography or MRI, and CSF studies. An elevated ESR may indicate vasculitis. Serological testing of blood and CSF for syphilis and HIV infection is important.
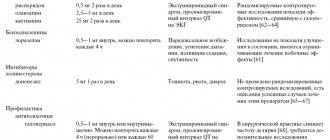
Treatment is carried out with the help of vasoactive drugs, drugs that improve the rheological properties of blood, nootropic drugs and other means. But more important are symptomatic measures, skin care, prevention of pulmonary and urinary infections, early and complete rehabilitation, including therapeutic exercises, massage, and physiotherapeutic procedures.
Symptoms
Acute circulatory disorders are manifested mainly by neurological symptoms. Manifestations depend on the type of pathological process.
Symptoms of ischemia (spinal cord infarction)
Several days and even weeks before acute disorders, the so-called. "harbingers". These include:
- transient weakness in the limbs;
- paresthesia (sensitivity disturbances);
- muscle discomfort;
- dysuria (impaired urination occurs infrequently);
- pain in the spine, radiating (radiating) to the arms and legs.
In the acute stage of development the following are noted:
- loss of sensation and weakness in the limbs;
- pelvic organ dysfunction;
- intense headaches;
- dizziness;
- loss of consciousness.
Paresthesia of the facial area, constriction of the pupil, drooping of the upper eyelid, and retraction of the eyeball cannot be excluded.
At the stabilization stage, with adequate therapy, regression of neurological symptoms is noted. In the residual period there are residual phenomena.
Symptoms of hematomyelia
Signs of hemorrhage in the spinal substance are:
- intense girdle pain;
- flaccid paralysis of the limbs;
- marked decrease in sensation in the affected arm or leg;
- dysfunction of the pelvic organs (with a large lesion).
The severity and combination of clinical signs vary depending on the location and size of the hematoma. If it is large, certain residual effects remain. Small hematomas in some cases resolve without consequences (with timely and competent treatment).
When blood accumulates between the walls of the spinal canal and the dura mater (epidural hematoma), clearly localized, sharp and intense pain is noted. Symptoms often recur; periods of remission range from several days to two or more weeks.
Hematorahis is characterized by the formation of a hematoma in the cavity between the arachnoid and pia mater of the brain. This rare form of stroke is manifested by acute “dagger” or “shooting” pain in the spine and general cerebral symptoms.