Why does angiopathy appear?
There are some diseases that cause the development of such ophthalmological pathology. This means the presence of:
- Diabetes mellitus.
- Hypertension.
- Atherosclerosis.
- Rheumatism.
- Disorders of the thyroid gland.
- Autoimmune vasculitis.
- Anemia.
- Leukemia.
- High intracranial pressure.
- Cervical osteochondrosis.
- Scoliosis.
In addition, retinal angiopathy is a consequence of diseases of the central nervous system, in which vascular tone is impaired, and congenital heart disease. Also, retinal angiopathy can be provoked by excess body weight, smoking, if production activities involve harmful substances, and long-term use of medications that contribute to impaired vascular tone.
Angiopathy can occur due to the penetration of toxins into the body, due to the fact that a person lives in a place where there is a high level of radiation. Another reason for the occurrence of the disease is the presence of a genetic predisposition. The risk zone includes people over 65 years of age and pregnant women.
Angiopathy - Causes
The reasons for the development of angiopathy include the following factors:
- Violation of the nervous regulation of the tone of the vascular wall;
- Traumatic injuries;
- Blood diseases;
- Smoking;
- Occupational hazards;
- Arterial hypertension;
- Elderly age;
- Diabetes;
- Systemic vasculitis of an autoimmune nature;
- Intoxication;
- Congenital structural features of the vascular wall (for example, telangiectasia).
Types of disease
The pathological condition of the body, when the blood supply to the fundus of the eye deteriorates, becomes the main cause of the development of retinal angiopathy. Capillaries in the visual apparatus can change regardless of age, but are often diagnosed in elderly patients. Considering the nature of the origin, retinal angiopathy can be:
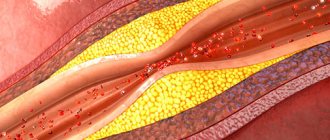
- Hypertensive. Hypertensive angioneuropathy develops due to high blood pressure. As a result of arterial hypertension, the central artery is damaged, blood vessels narrow, veins dilate, and retinal tissue is affected. Branching of the venous bed occurs, pinpoint hemorrhage occurs, and atherosclerosis may develop. If treatment for hypertension is started in a timely manner, there is a high probability of the eye structure returning to normal.
- Hypotonic. Due to low blood pressure, blood flow slows down, the tone of small capillaries decreases, so the blood thickens and blood clots begin to form. At the diagnostic stage, it can be determined that the arterial network has expanded and the veins are pulsating.
- Diabetic. Diabetes mellitus causes damage to all blood vessels, resulting in poor circulation, blockage of blood vessels, swelling of the capillary wall and deterioration of visual function. High glucose levels provoke the formation of blood clots, tissue atrophy, and multiple hemorrhages.
Types of vascular angiopathy of the eyes
Angiopathy is not a separate disease, but a complication of other diseases and conditions.
Types of angiopathy depending on the disease that caused the pathology:
Hypertensive angiopathy
. Develops in chronic hypertension. Due to too high pressure, the arteries of the retina of the eye narrow, the veins dilate, vascular sclerosis occurs, and pinpoint hemorrhages occur in the eye. If angiopathy is detected in time and treatment is started, then these processes are reversible. If the vessels become denser and exudates form in the fundus, you can completely lose your vision.
Hypotonic angiopathy.
It occurs due to low pressure and slow blood flow, causing blood vessels to become overfilled. The arteries of the fundus become dilated, the veins pulsate. High tortuosity of blood vessels is observed.
Diabetic angiopathy.
The pathology develops due to the patient having diabetes mellitus. If the large vessels of the eye are affected, we are talking about macroangiopathy; if the capillaries are affected, microangiopathy is diagnosed. Due to the disruption of metabolic processes in the body in diabetes, microcirculation of blood in the vessels of the eyes is difficult, the retinal tissue does not receive enough oxygen and vision deteriorates.
Traumatic angiopathy.
It develops due to injury to the neck or chest, which disrupts the flow of blood to the brain and increases intraocular pressure, which can lead to rupture of the blood vessels in the eye.
An ophthalmologist must diagnose angiopathy; this usually occurs by examining the fundus.
Stages of development of diabetic angiopathy disease
There are several types of diabetic angiopathy. She may be:
Non-proliferative. The vessels in the fundus are gradually affected, microscopic aneurysms form, and small hemorrhages develop. At this stage, the retina swells and the iris becomes redder.
Preproliferative. The retinal veins are damaged. Rupture of the vessel causes hemorrhage and the formation of venous infiltrate, which causes significant visual impairment.
Proliferative. It is the most difficult stage. New capillaries are formed, which are fragile. As a result, multiple hemorrhages appear, which cause retinal detachment.
Traumatic. If the head, neck or eyes are injured, blood vessels are compressed and intracranial pressure increases. As a result, leukocyte emboli are formed.
Youthful. It is a rare and dangerous form of the disease. The etiology is not fully understood. The development of pathology is observed before the age of 25 years. The manifestation of juvenile angiodystonia is the inflammatory process, hemorrhage, and proliferation of connective tissues. As a result, various complications arise.
Congenital. In most cases, premature babies suffer from this form of the disease due to the fact that their vascular system is underdeveloped.
To make the most accurate diagnosis and begin appropriate treatment, it is necessary to determine the type of retinal angiopathy. Treatment measures should begin when the initial stage is present. Without adequate treatment, the patient may go blind.
Diabetic angiopathy
Diabetes
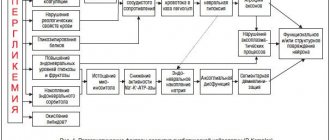
is a set of metabolic disorders characterized by hyperglycemia and disorders of carbohydrate, lipid and protein metabolism. These disorders can cause serious complications, including from the cardiovascular system.
The cause of death in 75-80% of patients with diabetes is coronary heart disease (CHD), cerebrovascular lesions and vascular diseases of the extremities. The main cause of acute heart failure in patients with type 1 diabetes is myocardial dystrophy and diabetic cardiopathy; in type 2 diabetes, the leading pathology is atherosclerosis.
Damage to the great vessels of the lower extremities in patients with diabetes is observed 3-5 times more often than in the population.
Features of diabetic macroangiopathy
(damage to large vessels) of the lower extremities is polysegmental and involvement in the process of arteries of other regions - heart, brain, kidneys, etc., as well as faster progression of the disease compared to classic atherosclerosis.
Risk factors
the development of vascular complications in diabetes are:
- uncontrolled hyperglycemia
(increased blood sugar levels), leading to dysfunction of the endothelium (internal vascular wall), the formation of free radicals that destroy the vascular wall; - obesity
and subsequent dyslipoproteinemia (increased levels of cholesterol, LDL cholesterol, triglycerides); - an increase in the level of insulin in the blood - hyperinsulinemia
- as a consequence of insulin resistance (the inability of insulin to perform its functions - often due to obesity), promoting the deposition of cholesterol plaques in the vascular wall; - hypertonic disease;
- smoking,
which inhibits the body's antioxidant defense, worsens the elastic properties of the arteries, and significantly reduces the oxygen content in the blood
A feature of diabetic angiopathy is also the frequent damage to the middle tunic of the arteries - Mönckeberg sclerosis or mediacalcinosis.
Obliterating atherosclerosis developing against the background of diabetes is also characterized by the fact that the frequency and severity of occlusive-stenotic processes increases in the distal parts of the lower extremities, as a result of which the possibility of collateral compensation (development of additional bypass vessels) is reduced - in contrast to classic “age-related” atherosclerosis.
The most characteristic feature of diabetes is the development of microangiopathy
(lesions of small vessels), which is generalized and manifests itself mainly in damage to the kidneys, retina, and limbs. As a result, the risk of blindness in patients with diabetes increases 25 times. Diabetes is also a leading cause of kidney failure. The average life expectancy of a patient from the onset of microalbuminuria (small protein fractions in the urine) to the development of renal failure is 5-10 years without timely treatment. A consequence of diabetic microangiopathy is also the development and intensification of ischemia (oxygen starvation) of the extremities in the absence of severe hemodynamic disorders (impaired blood flow in large arteries).
Pediatric retinal angiopathy
Complicated childbirth can cause the development of hypertensive angiodystonia of retinal vessels in a newborn child. Also, a provoking factor is birth trauma or impaired intrauterine development of the baby. In addition, there are a number of factors that can cause the development of a pathological condition in a child:
1. The woman did not eat properly while pregnant.
2. Presence of genetic predisposition.
3. Congenital defect of the cardiovascular system.
4. Premature delivery.
5. Hypoxia.
6. The cervical spine was damaged during childbirth.
If the newborn is given timely and correct therapy, the disease disappears within 8-10 weeks. If signs of angioneuropathy appear, you should immediately consult a specialized doctor. Such a disease may indicate the development of diabetes mellitus, glomerulonephritis, renal retinopathy, and impaired blood pressure.
At an older age, the development of childhood angiopathy is the cause of an infectious disease, vegetative-vascular dystonia, impaired material metabolism, and vascular pathology.
Development of angiopathy during pregnancy
This is a common phenomenon that occurs in both new and experienced mothers during the second or third semester. In most cases, the disease appears towards the end of pregnancy.
The appearance of retinal angiodystonia is associated with high blood pressure, atherosclerosis or diabetes mellitus. As the embryo grows, blood volume increases, pressure jumps (especially in a stressful situation), which causes the vascular walls to stretch. As a result, the risk of thrombosis, hemorrhage, retinal detachment, and blindness increases.
It is worth highlighting the characteristic differences of hypertensive angiopathy during pregnancy:
- Periodic narrowing of the arteries. The cause is toxicosis.
- Sclerosis of blood vessels.
- Impaired blood circulation.
- The visual system recovers quickly after the birth of a child.
If such a pathological condition develops during pregnancy, the doctor may prescribe a planned cesarean section. Natural childbirth can cause retinal vessels to rupture, and a woman can completely lose her vision.