Fibromyalgia (fibromyalgia syndrome) is a common neurological problem characterized by widespread pain and increased sensation in the body. Common complaints also include increased fatigue and sleep disturbances. Pain and tenderness may come and go and move throughout the body.
Fibromyalgia occurs in 4 out of 100 people. Women suffer from it 8-10 times more often than men. The disease usually begins in adulthood (between 20 and 50 years), but can occur in both adolescents and older people. At risk are patients with chronic diseases of the joints and connective tissue, such as osteoarthritis, systemic lupus erythematosus, rheumatoid arthritis, and ankylosing spondylitis.
Causes of fibromyalgia
The causes of the disease have not been clearly established. It is assumed that they may be different for different people. It is clear that fibromyalgia is not the result of an autoimmune, inflammatory, joint or muscle disease. Fibromyalgia can be inherited. There are likely certain genes that may make people more prone to fibromyalgia and other health problems that come with it. However, fibromyalgia itself is not a genetic disease.
Most often, there is a trigger factor that “starts” fibromyalgia. This could be a spinal problem, arthritis, injury, or other physical stress. Emotional stress can also be a trigger.
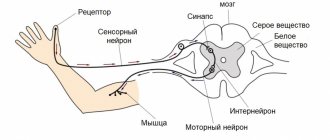
More recently, fibromyalgia has been described as a central pain enhancement disorder, which means that the level of pain sensation in the brain is too high. It is believed that the brain and nervous system are unable to process pain signals in the normal way, resulting in increased pain. In some studies, changes in pain processing in people with fibromyalgia have been confirmed by scan results. The researchers also found insufficient levels of serotonin in the nervous system and a subsequent imbalance in the cerebrospinal fluid, which is involved in pain signaling.
Although fibromyalgia can affect quality of life, it is still considered benign from a medical perspective. It does not cause heart attacks, strokes, cancer, physical deformities or death.
Fibromyalgia: myths and reality
Author:
Mingalieva Dina
3 minutes
3286
Fibromyalgia is a disease that causes severe tenderness and pain in the muscles and joints. People diagnosed with this condition experience constant pain, but the severity of the condition varies. The symptoms of fibromyalgia were first described in the early 19th century when the disease was called “muscular rheumatism,” but today fibromyalgia is still a mystery to the medical community. There are many myths and misconceptions around this disease; some doctors do not consider it a disease at all. A lot of material is devoted to this topic in Medical News Today.
THREE MAIN MYTHS
1. This disease does not exist
Pain is subjective and sometimes difficult to measure. Therefore, the most important misconception about fibromyalgia is that it does not exist. However, experienced doctors and people suffering from this disease say that this statement is completely untrue.
“We still don’t know the exact mechanism of development of the disease, but we do know that it is a diffuse complex pain syndrome,” the publication quotes Donnica Moore, head of the Sapphire Women’s Health Group. “Sometimes illness occurs for no apparent reason. In other cases, secondary fibromyalgia develops as a result of chronic sleep deprivation, viral infections, Lyme disease, arthritis, hypothyroidism and other diseases.”
Charlene Hoffman was diagnosed with fibromyalgia in 2014. She says: “I met people who said that I made it all up. Not all doctors know enough about this disease and rarely understand how to treat it, let alone diagnose it. I simply ignore those who do not understand what I am sick with. True friends accept me for who I am. As for doctors... Whenever I go to a new doctor, I take all my medical records and reference information with me.”
2. The disease only affects older women
Another common myth surrounding this disease is that it only affects older people, and most often women. According to the American National Institute of Arthritis and Musculoskeletal and Skin Diseases, about 80-90% of fibromyalgia sufferers are actually women. However, men can also get sick - and young ones at that. Journalist and blogger Emily Trimnall, 28, was diagnosed with fibromyalgia at age 13. She says: “The best way to combat misconceptions is to educate people. I talk openly about my problems."
3. The pain is not severe and does not affect daily life
Some people with fibromyalgia experience so much pain that they are unable to do anything. This accordingly affects the quality of life. “I'm a good artist, but drawing pains me because it's a repetitive motion,” says Heidi Moseley, who was also diagnosed as a child.
“I feel a lot of pain after drawing for several hours. It can take weeks to get back to normal,” Heidi shares.
In addition to pain, fibromyalgia causes other problems, for example:
- chronic fatigue
- depression
- headache and migraine
- painful periods
- irritable bowel syndrome
- morning stiffness (rigidity).
Combined with pain and tenderness, these symptoms can seriously interfere with normal life.
CAUSES AND DIAGNOSIS
Fibromyalgia is truly difficult to diagnose because there is no obvious cause for the disease. The main symptom is pain and tenderness throughout the body, but fatigue, insomnia and problems with memory and alertness are also common.
Experts identify several factors that can increase the risk of developing the disease:
- physically or emotionally difficult events, such as a car accident
- multiple injuries
- genetics
- problems with the central nervous system.
To diagnose fibromyalgia, doctors most often ask patients to describe their pain. Tests such as x-rays or blood tests are not required, but your doctor may order them to rule out another condition. Many patients see many doctors before receiving this diagnosis. It is important to find a knowledgeable specialist.
However, this does not mean that the disease cannot be diagnosed in principle. The American College of Rheumatology identifies several criteria that are used by the medical community to define the disease
- Pain and symptoms in the past week based on total number of painful locations
- Symptoms have lasted for at least three months
- There are no other health problems that could explain the pain and other symptoms.
Other symptoms include fatigue, feeling groggy in the morning, problems with memory or thinking, and other general physical problems.
TREATMENT
In 2004, the US Food and Drug Administration (FDA) approved the drug pregabalin (in Russia, trade name Lyrica) for the treatment of fibromyalgia. This medicine is also used in the treatment of other pain syndromes and epilepsy.
Doctors may also recommend a number of other medications to relieve pain, such as:
- paracetamol
- ibuprofen
- naproxen.
Your doctor may also prescribe medications such as tramadol. However, many such drugs can increase pain in the long term and lead to addiction. Some antidepressants, such as duloxetine and milnacepran, may also be helpful in managing pain and fatigue.
Experts also advise regular exercise, a healthy diet and good sleep. In addition to traditional treatment, alternative treatments may also relieve the condition. Donnika Moore recommends aerobics, yoga and Chinese gymnastics tai chi (tai chi) - as well as acupuncture and massage.
Manifestations of fibromyalgia
The main manifestation of fibromyalgia is increased sensitivity of the body (even pain). People may complain of musculoskeletal pain, tenderness and stiffness in various parts of the body, as well as sleep disturbances and fatigue. Some patients report that fatigue is the most frustrating aspect of fibromyalgia, as it can affect mood, concentration, memory and the ability to think clearly.
The full list of possible fibromyalgia symptoms also includes:
- headache;
- joint disorders;
- irritable bowel syndrome;
- poor circulation and tingling in the periphery;
- urgent urge to urinate;
- allergic reactions.
The pain of fibromyalgia tends to spread and usually feels like an aching or burning sensation. It varies in severity, but is generally more severe on the most frequently used areas of the body. Fatigue also varies in severity - up to complete exhaustion.
Many people may experience periodic flare-ups, where symptoms suddenly become worse. Some people with fibromyalgia report that their pain gets worse in very damp, cold or hot weather.
With mild or moderate symptoms, people can continue to live their lives as normal. However, when severe, fibromyalgia can affect people to such an extent that maintaining a job or having a normal social life seems impossible.
Symptoms of fibromyalgia
- The main symptom of the disease is pain. Moreover, patients complain of pain in various parts of the body. That is, pain sensations do not have any specific localization; they can appear simultaneously in the lower and upper parts of the body, on the right and on the left. The pain is long-lasting, that is, it bothers the patient for more than 3 months. Often the pain intensifies after performing any usual actions or moderate physical activity. But massage, rest, and being in a warm room, on the contrary, relieve pain, albeit for a short time. It should be noted that after resting for too long, the pain may become more intense.
- There is increased sensitivity at certain points in the body. These areas include: the back of the head, the upper spine, and the inside of the knee joint.
- Deterioration of mobility. This symptom is especially pronounced in the morning, however, slight stiffness can also occur during the day.
- Increased fatigue. The patient complains of constant fatigue, which does not go away even after rest (sometimes, on the contrary, the patient wakes up even more tired than before going to bed).
- Unpleasant sensations in certain parts of the body (especially in the limbs). Such sensations manifest themselves in the form of burning, tingling.
- Feeling of swelling in the knees and hands.
- Sleep disorders. Light sleep does not give a feeling of recuperation.
- Headaches, sometimes very intense.
- Unpleasant (sometimes painful) sensations in the legs, cramps, heaviness.
- Raynaud's syndrome. Most often it manifests itself in the form of numbness in the fingers.
- Mental disorders, manifested in the form of pain in the area of internal organs, without any reason that could cause them.
- Frequent depression, attention and memory problems.
Diagnosis of fibromyalgia
There are currently no specific tests to diagnose fibromyalgia, and many people with the condition have normal blood tests, x-rays and scan results. However, these studies may still be necessary, as they will allow the doctor to exclude other causes of complaints.
Currently, the diagnosis of fibromyalgia is established based on a combination of the following factors:
- pain throughout the body is felt for at least 3 months;
- there are cognitive problems such as poor memory and difficulty understanding;
- sleep does not help restore strength, fatigue accumulates.
Fibromyalgia
G.R. Tabeeva, A.M. Wayne
Department of Nervous Diseases FPPO
Moscow Medical Academy named after. THEM. Sechenov
In the last two decades, fibromyalgia (FM) has taken a strong place among the most pressing issues of modern medicine. Interest in FM is associated primarily with the evolution of views on its nature and the refusal of most researchers to consider it as an inflammatory disease of muscle tissue, which is why FM has been displaced from the narrow framework of rheumatological problems and is becoming increasingly an interdisciplinary problem. At the same time, research in recent years has identified a number of psychiatric and neurological aspects in it.
The disease acquired the term “fibromyalgia” only in recent years, although it has a history of more than 150 years, i.e. since the time when the terms “fibrositis”, “fibromyositis”, “tendomyopathy”, “myofibrillosis”, “muscular rheumatism”, “psychogenic rheumatism” began to be used to denote musculoskeletal pain, and on the other hand, to associate these disorders with the concepts pain points and trigger zones.
Criteria of the American College of Rheumatology (N. Smyth, M. Yunus, 1990):
1. The presence of generalized symmetrical pain (spreading to the right and left, upper and lower halves of the body, or axial), lasting for at least the last 3 months.
2. Pain on palpation of at least 11 out of 18 (9 pairs) of specific sensitive points. The following points are used:
- occipital region - place of attachment of m. suboccipitalis;
- neck region - anterior sections of the space between the transverse processes CV - CVII;
- trapezius muscle - middle of the upper edge;
- supraspinatus muscle at its insertion site;
- zone of articulation of the second rib with the sternum along its upper edge;
- a point located 2 cm distal to the external epicondyle of the shoulder;
- in the gluteal region - the upper outer quadrant of the buttock along the anterior edge of the muscle;
- greater trochanter of the femur;
- in the area of the knee joint - the medial fat pad.
Although the question of the nosological essence of FM is debatable, one should recognize its distinct not only clinical, but also pathophysiological independence, which was the reason for discussing FM as a possible primary disease.
The result of multicenter research from leading institutions studying this disease was the creation of diagnostic criteria for the positive diagnosis of FM, which combined all previously existing criteria (see sidebar).
The use of these criteria allows for a “reliable” (if all criteria are present) and “possible” (if there is an insufficient number of sensitive points) diagnosis of FM. The presence of other clinical pathology does not exclude the diagnosis of FM. Therefore, strictly speaking, the existing criteria for the diagnosis of FM imply syndromic diagnosis of FM with the exclusion of all possible other causes of a similar symptom complex. Thus, FM can be considered, on the one hand, a syndromic diagnosis, and on the other, a diagnosis of exclusion.
The concept of “sensitive point” (SP), used in all modern criteria, is generally accepted for FM. CT is practically the only specific sign of this disease. Although the number of positive points in patients with FM can be very different (up to 70 PTs have been described in one patient), their location and number is a unified system that facilitates the process of diagnosing this symptom complex. Therefore, the importance of CT for FM verification is very high. In addition, CTs have their own characteristic features: firstly, to cause pain, a slight effort is enough; secondly, with palpation you can get the pain that occurs spontaneously in patients (the phenomenon of “pain reproducibility”); thirdly, CTs are located in strictly defined anatomical zones, i.e. there is a specific map of their localization, which is given in modern criteria.
FM is a chronic disease that lasts for years and even decades, sharply worsening the quality of life of patients and, as a result, leading to severe maladjustment. This is not only a medical problem, but also a major social problem, the damage from which, particularly in the United States, amounts to tens of millions of dollars a year. As a result of this disease, about 30% of patients lose their ability to work, and about 5% become maladapted in everyday life.
FM is considered one of the most common forms of chronic pain syndromes. Epidemiological studies indicate a high prevalence of FM (2-6% in the population) among all ethnic, social and age groups.
Due to established traditions, patients with FM are most represented in rheumatological practice. In neurological practice, this is also a fairly common pathology. Nevertheless, there is a paradoxical situation in which the actual diagnosis of FM, even syndromic, is, in principle, absent in the daily practice of medical specialists. The reason for this, on the one hand, most likely lies in the variety of clinical manifestations of FM. Neurologists most often evaluate such patients in accordance with the leading comorbid manifestations (“panic attacks”, tension headaches, widespread osteochondrosis, myofascial syndrome, osteoarthritis, etc.). On the other hand, the reason lies in the underestimation of the significance of mental disorders and stress for these patients and the lack of generally established ideas and views on this symptom complex as a single suffering. Undoubtedly, such patients are also encountered in the practice of psychiatrists, who, however, do not diagnose patients with FM, since they do not subject the patient’s somatic state to a detailed analysis and do not examine their sensitive points.
Clinical picture
FM is defined as non-rheumatic non-articular diffuse (widespread) symmetrical pain, which is chronic in nature and accompanied by stiffness, depression, sleep disturbances and the presence of characteristic pain points.
The disease can occur at any age, but prevails in people of the most working age (25-45 years). There is a significant predominance of women among patients (10:1).
The course of the disease is chronic. Symptoms of FM may fluctuate as a result of exposure to triggering factors. Such factors are physical fatigue, prolonged postural loads, being immobile, emotional distress, as well as cold and humidity. The pain is relieved by heat, massage, and after rest, alternating with short periods of physical activity.
The basis of all clinical manifestations of FM is pain, which is present in 100% of patients, has characteristic features and is an obligate sign of FM. Pain is the main reason for such patients to visit doctors, and it is for this reason that they often go to rheumatologists. Along with the fact that this is, as a rule, generalized pain, painful sensations can also have a predominant localization, and therefore patients complain of pain in the neck, head, etc. The phenomenon of “pain everywhere” is characteristic - when, with active questioning of the patient, it is not possible to identify a pain-free zone. Interestingly, there is an obvious dissociation between the intensity of pain (which patients themselves assess) and the degree to which these sensations are experienced. By nature, this pain is often monotonous, debilitating and has all the features of chronic pain. Its intensity, however, can increase sharply, then this condition is referred to as a “fibrositis storm.” Cases have been described in which patients underwent surgical interventions due to these pains.
A special place in the overall picture of clinical manifestations of FM is occupied by depressive disorders, which are almost obligate for it. Depression is the main cause of deterioration in the quality of life of patients. Quite typical in these cases are complaints of depressed mood, narrowing of the range of interests and loss of a sense of pleasure. But this clinically obvious variant of depressive disorders is observed only in half of the patients. In other cases, depression is hidden under the guise of a variety of vegetative, somatic and numerous algic manifestations. In these cases, it is more appropriate to talk about the presence of hidden or somatized depression in FM. The high association between chronic pain and depression is especially typical for FM in its main clinical manifestations, type of course, and response to all types of antidepressant therapy.
One of the most striking clinical manifestations of FM is sleep disturbances. In the literature, sleep with FM has received the characteristic name “non-restorative” due to a peculiar set of typical complaints about the lack of sensations of rest after sleep, when patients wake up with a feeling of fatigue, and their sleep is described as superficial and restless. Actually, one of the reasons for the increased interest in the problem of FM was the research of the Canadian researcher H. Moldofsry, who in 1975 described a phenomenon characteristic of FM, called “alpha-delta sleep.” It lies in the fact that the structure of the deep stage of sleep, characterized by low-frequency, high-amplitude delta waves, includes fragments of high-frequency oscillations of alpha waves. Subsequently, this phenomenon was confirmed by the results of most studies and became characteristic of FM. Although it is not absolutely specific for FM, since previously in some studies it was shown in patients with depressive disorders, which perhaps once again demonstrates the similarity of their pathophysiology with FM.
FM is also characterized by the presence of morning stiffness, which is observed in 91% of patients. Its duration ranges from several minutes to several hours. To get rid of this feeling, patients often use heat and physical exercise. However, the presence of asthenia, which is also characteristic of these patients, limits the ability of patients to be physically active and forces them to remain motionless for a long time, which further aggravates stiffness and pain.
In addition to the described obligate symptoms, FM is characterized by a whole symptom complex of psychovegetative, psychosomatic and various algic disorders, which occur in FM several times more often than in the population. The high association with FM allows us to consider them as comorbid. The most common among them are the following: “panic attacks”, hyperventilation syndrome, tension headaches, migraines, lipothymic conditions, irritable bowel syndrome, cardialgia, abdominalgia, Raynaud’s syndrome, myofascial pain, etc. It should be emphasized that one patient, as a rule, one can detect a whole symptom complex of the mentioned disorders, the dominance of which in the clinical picture often makes it difficult to identify “fibromyalgic phenomena proper,” which is reflected in the interpretation of these patients and, as a consequence, in the leading diagnosis (tension headaches, chronic myofascial syndrome, etc.).
The relationship of FM with myofascial pain syndromes of a predominantly chronic course is especially discussed. There are several views on the nature of these relationships - both recognizing the fundamental differences between them, and considering one as a clinical variant of the other.
Our team (headed by S.B. Korotkova) studied 60 patients with FM and 20 patients with chronic myofascial syndromes (MCS). The diagnosis of FM was established in accordance with the main generally accepted criteria (1990). 87% of patients with FM abandoned their usual professional activities, and 67% had a disability group for the underlying disease. The degree of maladjustment of these patients was confirmed by the use of special tests. In accordance with the results of the MMPI test, the average personality profile of the patients could be characterized as anxious-depressive with hypochondriacal tendencies, and according to the Beck test, it was possible to state the average degree of depression in these patients. When studying data from a test of pain coping strategies, it was shown that among the complex of emotional and behavioral reactions that arise in response to pain, passive strategies predominated in patients with FM (catastrophizing, desire for social support, hopelessness and helplessness, restrictive behavior). Along with this, in patients with FM it was possible to note significantly higher rates of reactive and personal anxiety according to the results of the Spielbeger test, as well as a higher prevalence of autonomic dystonia syndrome. All of these disorders reliably distinguished patients with FM from the control group, and the corresponding indicators of patients with MFS were within normal limits.
Clinically, it was possible to distinguish fundamental differences between these two groups of patients. In FM, the onset of the disease was significantly more likely to occur after a stressful situation (87%) and much less frequently the disease was preceded by injury and prolonged stress caused by posture (in patients with MFS, the opposite ratios were observed). Pain with FM in all patients was chronic, diffuse, symmetrical, and its intensity depended on the emotional state of the patients, quality of sleep, and meteorological factors. Pain with MFS was often local in nature and was strictly associated with postural strain and correlated with a particular muscle group. Fundamental differences were characterized by CT in patients with FM and trigger points in patients with MFS. Palpation of trigger points is characterized by the presence of a pain pattern and a zone of reflected pain, often located far from the trigger (this pain does not obey the principles of either radicular or segmental irradiation), and is also accompanied by a “jumping symptom.”
These groups are fundamentally distinguished by the results of the study of the nociceptive flexor reflex, which makes it possible to generally assess the state of pain and analgesic systems. In patients with FM, there is a gross decrease in the thresholds of subjective assessment of pain and the threshold of the flexor reflex, which indicates a disruption in the interaction of noci- and antinociceptive mechanisms. These results are also consistent with the results of studies of somatosensory evoked potentials (SSEPs). In patients with FM, a significant increase in the amplitudes of the early (H0, N0, H1) components was obtained, which reflects an increase in the activity of specific afferentation mechanisms, and in conditions of decreased pain thresholds, it may indicate an insufficiency of the mechanisms that control the intensity of sensory afferentation. This complex of clinical and psychophysiological features of FM allows us to speak in general about the special independence of this symptom complex, in which mental, vegetative processes and systems that control pain mechanisms interact in a special way at the clinical and psychophysiological level. This fundamentally distinguishes FM in general and from MFS in particular.
Such attempts to strictly differentiate between MPS and FM are not always justified in practice, since it is often possible to identify signs of FM in the same patient in the presence of local pain phenomena that bear all the features of myofascial pain. This is not paradoxical, since in the light of the concept of FM as a model of chronic pain-depression, in which the functioning of the systems that control pain sensations is impaired. From these positions, it becomes clear that in patients with reduced tolerance to pain, habitual stress, as well as stress caused by posture, ceteris paribus, can more quickly and easily form various algic phenomena, including myofascial pain.
Treatment
Treatment of patients with FM is difficult. Non-pharmacological treatment methods include various modifications of psychotherapeutic approaches, autogenic training, and biofeedback methods.
Since FM is a chronic disease that lasts for decades, patients usually have a long history of using various analgesic drugs that have disappointing results. Therefore, the prescription of analgesics should be justified. Among this group, preference should be given primarily to non-steroidal anti-inflammatory drugs, which can be used long-term and which are safer (ibuprofen). These drugs are best used in the form of creams and ointments. In some cases, drugs that have a muscle relaxant effect - tizanidine - are used. However, it is clear that such treatment is symptomatic.
Among all groups of pharmacological agents, the most justified is the use of antidepressants. Tricyclic antidepressants (amitriptyline, nortriptyline), serotonin-increasing drugs: sertraline, fluoxetine, paroxetine and other classes of antidepressants are widely used. Benzodiazepines (alprazolam) are considered less effective. In recent years, attempts have been made to use botulinum toxin drugs to treat patients with FM. However, their effectiveness is still difficult to assess. Our experience in treating patients with FM allows us to highlight some features of approaches to treatment tactics and the selection of the most effective pharmacological and non-pharmacological methods. The first group of patients was treated for 6 weeks with the selective serotonin reuptake inhibitor fluoxetine at a dose of 20 mg/day. The second group received a 6-week course of treatment with the four-cyclic antidepressant mianserin at a dose of 30 mg/day. The third group of patients received a 2-week course of treatment with the nonsteroidal anti-inflammatory drug ibuprofen at a dose of 800 mg/day. The fourth group received a 10-day course of melatonin at a dose of 1.5 mg at night to correct sleep disorders. The fifth group received phototherapy (treatment with bright white light, a course of 10 procedures). This method has proven itself well for treating patients with seasonal affective disorder.
Assessing the overall comparative effectiveness of these treatment methods, we can say that the most pronounced antidepressant and analgesic effect was the use of fluoxetine and phototherapy, and to a lesser extent, mianserin. Other methods of pharmacological treatment had a selective effect (ibuprofen had only some analgesic effect, and melatonin had a positive effect on night sleep characteristics), so patients assessed their use as ineffective. Thus, we can conclude that the choice of treatment method for patients with FM should be based on the potential for analgesic and antidepressant effects, i.e. influence the main core - depression-pain. In this sense, the greatest results can be achieved with complex therapy.
Literature:
1. Fedorova I.E. Fibromyalgia syndrome. Ross. honey. magazine 1996; 1:21-5.
2. Autonomic disorders. Ed. A.M.Veina. M., 1998, pp. 597-603.
3. Chichasova N.V. Primary fibromyalgia: clinical manifestations, diagnosis, treatment. Ter archive, 1994; 66(11):89-92.
4. Kennedy M, Felson D. A prospective long-term study of FMS. Arthritis Rheum 1996; 39:682-5.
5. Moldofsky H. Sleep and fibrositis syndrome. Rheum Dis Clin North Am 1989; 15:91-103.
6. Wolfe F, Ross K, Anderson J. The prevalence and characteristics of FM in the general population. Arthritis Rheum 1995; 38:19-28.
7. Wolfe F, Smyth H, Yunus M. The American College of Rheumatology 1990 Criteria for the classification of FM. Arthritis Rheum 1990; 33:160-72.
8. Yunus M, Masi AN, Calabro JJ. Primary FM. Semin Arthritis Rheum 1981; 11:151-71.
Published with permission from the administration of the Russian Medical Journal.
Management and treatment
Currently, this painful condition is considered incurable. Treatment is aimed at reducing and relieving symptoms and maximizing overall health.
Fibromyalgia does not cause permanent damage to connective tissue, but staying healthy and active can help muscles stay in good condition and prevent potential problems associated with weakened muscles.
The treatment of fibromyalgia uses both medications (these can be over-the-counter painkillers, painkillers, and even antidepressants) and non-drug techniques, including massage, reflexology, cognitive behavioral therapy, exercise, walks in the fresh air, monitoring sleep patterns, etc. .d.
Rate how useful the material was
thank you for rating
Treatment methods
Drug treatment
Antidepressants are recommended as initial medications for treating symptoms of fatigue. These drugs affect symptoms such as pain, fatigue, and depressed mood. The best known tricyclic antidepressants, such as amitriptyline, provide effective symptom relief. But these drugs cannot completely eliminate the pain syndrome. Anticonvulsant medications, such as Lyrica, have been shown to be quite effective in some patients. But this drug can cause side effects such as drowsiness, dizziness, swelling, and weight gain. Other drugs in this group are also used.
In recent years, antidepressants from the class of drugs known as serotonin and norepinephrine reuptake inhibitors, such as Cymbalta or Savella, have become quite widely used. Drugs from this group help reduce pain and improve overall well-being in patients with fibromyalgia. Side effects of these drugs may include nausea, dizziness, and insomnia.
Medicines that increase sleep duration may help treat fibromyalgia symptoms. It is possible to use low doses of a drug such as amitriptyline. Anti-inflammatory drugs - including ibuprofen and naproxen - do not have much therapeutic effect, since there is no inflammation in fibromyalgia. In addition, drugs from the NSAID group have a number of side effects such as stomach irritation, bleeding, and increased blood pressure. It is possible to use drugs such as paracetamol, because the irritant effect on the stomach is not very great, and it potentiates the effect of other drugs used to treat fibromyalgia. Muscle relaxants (mydocalm, sirdalud) can reduce muscle spasms and improve sleep, especially if used in the evening.
Steroids are usually used in cases where there are concomitant rheumatological diseases.
It is also possible to inject steroids into tender points, but the effectiveness of this method is quite controversial.
The introduction of Botox into tender points has become widespread recently, and studies have shown the fairly high effectiveness of this treatment method. Non-drug treatment methods:
- Acupuncture. Research has shown that the use of acupuncture changes brain metabolism and increases tolerance to the perception of pain.
- Manual therapy helps reduce muscle pain and increase range of motion in the spine.
- Massage, both classical and acupressure, can stimulate blood circulation and reduce muscle spasms.
- Biofeedback . This treatment method allows the patient to learn to control their sensations and reduce chronic pain.