Causes of mental illness
The exact cause of schizophrenia has not yet been identified. It is believed that this is a multifactorial disease that develops under the influence of a number of provoking and predisposing factors:
- Burdened heredity. If you have close relatives with schizophrenia, the risk of developing it in your offspring increases by about 20 times.
- Unfavorable social conditions such as poverty and family instability.
- Bad habits. Smoking, drug addiction, substance abuse and alcoholism do not so much cause the disease as accompany schizophrenia, complicating its course.
- Complicated pregnancy (prematurity, intrauterine hypoxia or infections).
- Emotional turmoil, especially in childhood. It has been proven that people who have experienced physical or sexual violence are more likely to develop schizophrenia.
- Anomalies in the development of central nervous system structures. Autopsies of dead patients showed that most of them had dilation of the cerebral ventricles, a decrease in the volume of the frontal lobe, and organic changes in the temporal gyri and hippocampus.
There are other theories of the development of schizophrenia that are not so popular and widespread.
Pharmacotherapy of cognitive impairment
When treating schizophrenia, it is important to pay attention to the state of the cognitive sphere of patients. However, unfortunately, at present there are no medications that can effectively eliminate the manifestations of cognitive deficit.
Unlike traditional antipsychotics, which weaken motivation, some atypical antipsychotics have a positive, although small, effect on memory. At the same time, some atypical antipsychotics open up the possibility of improving memory with the help of special cognitive training , in particular, performing tasks that require accelerating memory.
As noted above, dysfunction of executive functions is registered already in the initial phase of schizophrenia and persists throughout its course. J. Arnt, M. Dendriksen (2006) in their review on the effect of antipsychotics on the cognitive sphere of patients with schizophrenia, came to the conclusion that drugs that intensively bind D2 receptors negatively affect the cognitive abilities of patients with schizophrenia. At the same time, J. Lee et al. (2007) found that in patients naive to any antipsychotics, after 8 weeks of treatment with haloperidol or risperidone, there was no change in executive function ability as measured by the Wisconsin Card Sorting Test (WCST). Both drugs, on the contrary, even improved the performance of the labyrinth test. According to K. Gauggel (2008), in terms of assessing the effect of antipsychotic drugs on the cognitive sphere of patients with schizophrenia, the so-called MATRICS initiative, which was created in 2003 on the basis of a standardized battery of tests, is represented.
The literature devoted to correctors of extrapyramidal disorders that have developed as a result of taking antipsychotics emphasizes that anticholinergic drugs significantly worsen the state of the cognitive sphere of patients with schizophrenia . Due to the above, unreasonable use of these drugs is not recommended, especially for a long period. Taking into account the peculiarities of the interaction between the dopaminergic and cholinergic systems of mediators, it can be assumed that traditional antipsychotics that block D2 receptors and correctors of extrapyramidal symptoms, which have anticholinergic activity, potentiate the negative effect on the cognitive abilities of patients with schizophrenia. Clinical observations indicate that anticholinergic drugs can provoke a relapse of this mental disorder, in particular by causing an exacerbation of productive symptoms. On the other hand, patients often use these medications as psychostimulants to combat apathy and decreased energy potential.
A number of foreign studies have shown that drugs with anticholinergic activity can cause isolated impairments of declarative memory in patients with schizophrenia. At the same time, despite the fact that clozapine, unlike risperidone, exhibits a clear anticholinergic effect, it does not differ from the latter in the degree of influence on the memory of patients with schizophrenia. This can be partly explained by the fact that the main metabolite of clozapine, desmethylclozapine, exhibits antagonism towards M1 muscarinic receptors.
If we rank modern antipsychotics according to the degree of their anticholinergic effect, then clozapine and olanzapine will be in the first positions, and aripiprazole, risperidone and ziprasidone - in the last, with quetiapine likely to occupy an intermediate position. As a result of the above, it can be assumed that clozapine and olanzapine will have a more negative effect on the cognitive sphere of patients with schizophrenia than aripiprazole and ziprasidone.
Currently, various pharmaceutical companies are attempting to synthesize drugs that have a positive effect on the cognitive sphere of patients with schizophrenia. Despite encouraging results, most of these medications are not officially approved. Thus, in particular, in terms of improving cognitive abilities, the new drug tolcapone, which affects the activity of catechol-o-methyltransferase, is of interest. Buspirone and tandospirone, considered partial agonists of 5HT1A receptors, used in combination with antipsychotics, improve the cognitive state of patients with schizophrenia. Glutamate agonists such as glycine and D-serine, as well as the partial agonist D-cycloserine, show positive effects on cognitive function, but do not show this in combination with clozapine. The glycine transporter and inhibitor sarcosine also improves cognitive function, but in combination with clozapine this effect is noticeably weakened. Xanomeline, an agonist of M1 and M2 receptors, is effective in Alzheimer's disease, but in schizophrenia, the ability of this drug to improve the cognitive state of patients is questioned.
Stages
The disease goes through several stages in its development, each of which is characterized by certain typical manifestations.
- Primordial. During this period, a person’s personal qualities and behavior change. The patient becomes distrustful and overly suspicious.
- Prodromal. The patient withdraws into himself, limits himself as much as possible from others, and stops communicating even with the closest people. At this stage, a person often loses his job due to his absent-mindedness, irresponsibility and lack of concentration.
- First mental episode. During this period, the patient is susceptible to obsessions and delusions, and may see hallucinations.
- Remission. This time period can vary in length from a couple of weeks to several years.
After the completion of the first cycle, a periodic change of the 3rd and 4th stages begins. Gradually, the duration of remissions decreases, and exacerbations become longer and more severe.
Signs of schizophrenia
The development of vivid and characteristic clinical manifestations of schizophrenia is preceded by a premorbid period, which can last several years. During this time interval, loved ones note that the person is behaving somehow differently, has become more aggressive, withdrawn and distrustful.
The height of the disease is characterized by the development of two types of symptoms.
Positive symptoms
- Hallucinations. They can be auditory, when the patient hears voices that control his behavior, threaten him, order him to perform this or that action. Visual hallucinations are also possible, but are extremely rare.
- Rave. This symptom is characterized by the patient’s belief that evil spirits or alien beings are influencing him using magic, hypnosis, or any technical devices that do not exist in reality. Delusions of jealousy (confidence of betrayal), persecution (the patient thinks that he is being watched), self-flagellation (the patient is to blame for all earthly troubles), grandeur (a person may introduce himself as the ruler of the world), dysmorphophobia (confidence in his own external ugliness) may also occur.
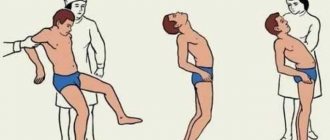
- Obsessions and movements.
- Reasoning and lengthy reasoning. Patients are unable to concentrate on one topic, constantly jump from one to another, and often lose the thread of the story.
Negative symptoms
- Emotional disorders and social isolation. Schizophrenics immerse themselves in themselves and completely isolate themselves from others.
- Drift is the inability to make one's own decisions. Patients copy the behavior of others.
- Hypobulia. Patients' needs are reduced, they don't care what they eat, they refuse to take a shower, and their libido disappears.
Maintenance therapy
Therapy for a patient with schizophrenia should be “supportive”, continuous and long-lasting.
In the process of treating schizophrenia, it is necessary to create and maintain a long-term state of “therapeutic effect”.
From the point of view of a number of psychiatrists, maintenance therapy is necessary for the correction of psychopathological disorders (symptomatic treatment) and the desire to prevent relapse (preventive treatment). However, the differentiation of maintenance therapy into “supportive-blocking” and “supportive-preventive” treatment has not yet found widespread use (Maslovsky S.Yu., 2006).
Domestic psychiatrists V.M. Banshchikov, R.G. Golodets, S.G. Back in the late 50s, for maintenance therapy of schizophrenia with aminazine, Zhislin was recommended to take this drug for six months to a year or more after stopping an acute episode of the disease.
In the late 90s, many foreign psychiatrists advised continuing therapy with psychotropic drugs for at least a year after the first attack of schizophrenia and up to 5 years in the chronic course of the disease (Johnson D., 1990). For frequent relapses of schizophrenia, lifelong use of an antipsychotic is recommended.
It is important to motivate the patient to continue taking the drug he needs. In this case, one should keep in mind his social and labor status.
If medication is suddenly stopped, symptoms of psychosis will usually relapse within the next few weeks.
To control the drug intake, you can administer it intramuscularly or monitor the patient for 30 minutes after taking its oral forms.
It is noted that from 45 to 60% of patients take psychotropic drugs, violating the instructions of their doctors. With most chronic diseases, in particular cardiac diseases, for example, hypertension, almost the same picture is observed, especially in men.
Self-cessation of psychotropic drug therapy by patients with schizophrenia usually leads to relapse of the disease, which is observed in 75% of patients, with relapse most often occurring within the first two months after stopping therapy.
Discontinuation of medications in 50% of cases causes a relapse in the first 6 months after stopping an exacerbation of the disease; in 80% of cases, a relapse is observed during the first year. Even with compliance with the drug therapy regimen, the relapse rate is 10-15% in the first 6 months and not higher than 25% in the first year after the exacerbation is stopped. According to some data, if therapy is discontinued, a relapse of schizophrenia develops in almost all patients (10% of patients every month) (Davis D., 2006).
Unfortunately, more than 35% of patients with schizophrenia begin to violate the treatment regimen during the first 4-6 weeks of treatment; within two years, 75% of patients only partially maintain the required treatment regimen (Bloch Y. et al.).
It is generally accepted that compliance with the therapy regimen depends on the degree of criticality of patients to their condition, the convenience of dosing and administration of the drug, the severity of side effects of therapy and the nature of the relationship between the patient and his doctor.
In the stabilization phase of remission, it is recommended to continue the treatment regimen chosen to relieve the acute episode, using the same antipsychotic in the same dose, for at least 6 months (Merlo M. et al., 2002). After the formation of high-quality remission of schizophrenia during the stabilization of the process, a gradual and extremely careful reduction in the dose of the antipsychotic is possible. According to some authors, there are currently no reliable methods for identifying the minimum effective dose required for maintenance treatment of a patient with schizophrenia.
With each subsequent relapse of the disease, the doses of maintenance therapy are usually higher than after the relief of the first psychotic episode.
The first signs of exacerbation of the process require an increase in the dosage of the drug that the patient took previously.
Recently, there have been works in the literature in which, instead of continuous maintenance pharmacotherapy, it is recommended that a patient with schizophrenia be treated with intermittent courses (“interval therapy”) of atypical antipsychotics. In the case of stable remission after selecting optimal doses of the drug, intermittent courses of therapy seem to be more preferable.