What is dementia
With the development of dementia, a person’s mental abilities decrease, existing knowledge and skills are gradually lost, and the ability to learn is lost.
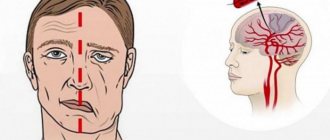
Thinking, orientation, understanding, counting, learning, language and judgment are impaired. There are many reasons why dementia develops. Dementia can be triggered by endocrine and vascular pathologies, depression, certain infections, traumatic brain injuries, brain tumors, alcoholism and drug addiction. Additional risk factors for developing dementia include:
- heredity. Moreover, the risk increases if the pathology in close relatives developed before the age of 65 years;
- obesity;
- lack of active intellectual activity.
Prevention and treatment of dementia
It is believed that approximately 10 neurons are required to store one bit (unit) of information. If we take into account all the neurons of the brain (approximately 1011), then the nervous system can store 1019 bits of information, of which no more than 5–10% are actually used by humans. Post-mortem morphological studies indicate that with age, the death of brain neurons occurs (for example, by the age of 70–80 it reaches 32–48%). This causes a decrease in brain weight (by an average of 90 g) and a decrease in the activity of neurotransmitter systems, as a result of which, with age, first of all, cognitive functions deteriorate: • decrease in reaction speed (bradyphrenia); • it becomes difficult to concentrate for a long time (fatigue); • working memory decreases (learning difficulties); • it is more difficult to change the program of action (intellectual “rigidity”). In accordance with the nature and severity of cognitive impairment, the following main syndromes are distinguished: • physiological involutive changes in cognitive abilities (“aging-associated cognitive impairment”, English: aging-associated cognitive decline, 1994); • mild cognitive impairment, 1997; • dementia [4]. Natural involutive changes in cognitive functions (or sometimes the term “successful aging” is used) are normally expressed very little in quantitative terms. Below are the criteria for the diagnosis of “aging-related cognitive impairment”: • cognitive impairment as reported by the patient or his relatives; • gradual development of disorders and their presence for at least 6 months, without episodes of sharp deterioration during this time; • impairment in one of the following areas: memory, attention, thinking, speech, visual-spatial orientation; • results of neuropsychological tests are at least one standard deviation below the norm developed for this age category. The most important factors contributing to the progression of age-related cognitive dysfunction are: • arterial hypertension; • hyperlipidemia; • diabetes; • vitamin deficiency; • hyperhomocysteinemia; • deficiency of testosterone and estrogen; • cardiac and respiratory failure; • long-term use of drugs with anticholinergic activity; • low intellectual activity; • hereditary predisposition (APOE-4). The term “moderate cognitive impairment” refers to impairments of one or more cognitive functions that go beyond the age norm, but do not reach the severity of dementia. The syndrome of moderate cognitive impairment in most cases is a pathological condition, as a result of which changes at this stage are not limited to age-related involutive processes. In most cases, it is associated with an incipient brain disease (repeats the etiology of dementia). According to a number of researchers, mild cognitive impairment syndrome is observed in 15–20% of people over 65 years of age. Long-term observations indicate that within 5 years, dementia develops in 60–80% of patients with this pathology. Only in 20–40% of cases, mild cognitive impairment is stable or slowly progressive (i.e., does not develop into dementia) [5]. Currently, there are three main clinical variants of the disease [R. Peterson, 2001]: • amnestic variant (memory impairments for current events dominate) – is a harbinger of Alzheimer's disease; • with multiple cognitive impairment (the presence of combined damage to several cognitive functions) - the outcome may be Alzheimer's disease or, less commonly, vascular dementia; • with impairment of one cognitive function while memory is intact (for example, the predominance of visual-spatial impairments means an increased risk of developing dementia with Lewy bodies). Modified diagnostic criteria for mild cognitive impairment syndrome [S. Guateir et. al., 2004]: • cognitive impairment according to the patient and/or his immediate family; • deterioration of cognitive abilities compared to baseline; • objective evidence of cognitive impairment obtained using neuropsychological tests (a decrease in the results of neuropsychological tests by at least 1.5 standard deviations from the average age norm); • absence of disturbances in the patient’s usual forms of daily activity (the possibility of difficulties in complex activities is allowed); • absence of dementia (Mini Mental State Examination score less than 24 points). The prognosis for the presence of mild cognitive impairment syndrome is quite serious. Thus, the risk of death is 1.7 times higher and the risk of Alzheimer’s disease is 3.1 times higher. Unfavorable prognostic signs for mild cognitive impairment are: – old age; – low results of neuropsychological tests; – family history of dementia; – hippocampal atrophy on brain MRI; – rapid increase in cerebral atrophy with repeated CT or MRI studies; – carriage of the APOE-4 allele. Dementia is the most severe clinical variant of cognitive dysfunction in old age. Dementia is understood as a diffuse impairment of mental functions as a result of organic brain damage, manifested by primary disorders of thinking and memory and secondary emotional and behavioral disorders. Yu. Melikhov wrote: “Time draws the most evil cartoons.” Dementia occurs in 10% of people over 65 years of age, and in people over 80 years of age it reaches 15–20%. There are currently 24.3 million people with dementia worldwide. Moreover, by 2040 the number of patients with dementia will reach 81.1 million. More than 100 nosological forms that can lead to dementia are described in the literature. The main causes of dementia: – Alzheimer’s disease (25–45%); – dementia with Lewy bodies (10–25%); – mixed dementia (10–25%); – vascular dementia (10–15%). To diagnose dementia, ICD-10 diagnostic criteria are widely used: • memory impairment (impaired ability to remember new material, difficulty in reproducing previously learned information); • impairment of other cognitive functions (impaired ability to judge, think - plan, organize - and process information); • clinical significance of the detected disorders; • impairment of cognitive functions is determined against the background of preserved consciousness; • emotional and motivational disorders; • duration of symptoms is at least 6 months. Severity of dementia: Mild – professional activities and social activities are clearly limited; – the ability to live independently, maintain personal hygiene is preserved, mental abilities are not affected. Medium – difficulties living independently; – some control is required. Severe – activities of daily living are impaired; – constant maintenance and care are required; – failure to maintain minimal personal hygiene; – motor abilities weaken. Thus, Gerald Ford wrote about former US President Ronald Reagan, who suffered from severe dementia: “It was sad. I stayed with him for half an hour. I tried to remind him of various episodes of our friendship, but, unfortunately, nothing came of it...” In 1998, Reisberg et al. proposed the concept (theory) of retrogenesis, according to which a patient with dementia goes through a kind of “reverse development.” Table 1 provides a comparison of skills that emerge as children develop and that are consistently impaired as dementia progresses (Table 1). This theory is very revealing in the analysis of the works of artists who suffered from dementia. The most famous is the German artist Carolus Horn (1921–1992). In the mid-1980s. the master works in the style of “naive art,” which coincides with the onset of his illness. His paintings looked like they were drawn by a child (Fig. 1 and 2). A progressive decline in memory in old age is primarily observed in Alzheimer's disease and proceeds, unlike other dementias, in accordance with Ribot's law: “First, events of the immediate past are forgotten, then, as the disease progresses, amnesia spreads to more distant events.” The modern classification of Alzheimer's disease is based on its age principle. In accordance with this, we distinguish: • early Alzheimer's disease, i.e. before 65 years of age, onset (presenile dementia of the Alzheimer's type), corresponds to classic Alzheimer's disease (“pure”); • late Alzheimer's disease, i.e. after 65 years, onset (senile dementia of the Alzheimer's type). Alzheimer's disease is heterogeneous in its origin: - in some cases, the disease is hereditary in nature (the presence of mutations in chromosome 21 - the amyloid b-precursor protein gene - and, possibly, in chromosomes 14 (presenilin-1) and 1 (presenilin-2) - risk get sick before the age of 60, chromosome 19 (APOE-4 gene) – risk of getting sick after 60 years); – in others it is sporadic. Risk factors for developing Alzheimer's disease are: – age; – hereditary burden; – the presence of apolipoprotein e-4 (promotes the formation of senile plaques); – Down syndrome in relatives; - female; – low level of education. The key neuromorphological phenomena of the disease are senile plaques (consisting of b-amyloid) and neurofibrillary tangles (Fig. 3). Criteria for the diagnosis of “probable Alzheimer's disease” [G. McKahn et al., 1984]. Mandatory signs: – presence of dementia; – the presence of impairments in at least two cognitive areas or the presence of progressive impairments in one cognitive area; – progressive deterioration of memory and other cognitive functions; – absence of disturbances of consciousness; – manifestation of dementia in the age range from 40 to 90 years; – absence of systemic dysmetabolic disorders or other brain diseases that would explain impairments in memory and other cognitive functions. Additional diagnostic features: – presence of progressive aphasia, apraxia or agnosia; – difficulties in daily life or changes in behavior; – family history of Alzheimer’s disease; – no changes in routine examination of cerebrospinal fluid; – no changes or nonspecific changes (for example, an increase in slow wave activity) in electroencephalography; – signs of increasing cerebral atrophy during repeated CT or MRI studies of the brain. The initial symptoms of Alzheimer's disease are usually nonspecific and include decreased initiative, limited interests, increased dependence on others, and apathy. The first signs of Alzheimer's disease: – difficulties in learning and assimilating new information; – difficulties in performing complex everyday tasks; – difficulties in orientation in space; – weakening and/or deterioration of thought processes; – speech (dysphasic) disorders; – changes in mood or behavior. Clinical features of advanced stages of Alzheimer's disease: – severe mnestic disorders; – apraxia; – agnosia; – speech disorders (aphasia) and disorders of other cognitive functions. The course of Alzheimer's disease can be complicated by the occurrence of various mental disorders. Psychopathological disorders: – affective disorders (usually depressive); – hallucinations and delusions; – anxiety and fears; - state of confusion. Behavioral disorders: – spontaneity; – aggressiveness; – excitability; – disturbance of the sleep-wake rhythm. Thus, a violation of the circadian rhythm is accompanied by disorientation, restless behavior, fussiness, “getting ready for the road,” knitting knots from bed linen, taking things out of closets, etc., i.e. manifestations of behavioral disorders. The term “vascular dementia” is commonly understood as several clinical-pathomorphological and clinical-pathogenetic syndromes, common to which is the relationship between cerebrovascular disorders and cognitive impairment. Risk factors for vascular dementia: – arterial hypertension; - diabetes; – damage to the main arteries of the brain; – hyperlipidemia; – cardiac disorders. Pathophysiological classification of vascular dementia [Chui, 1993]: – multi-infarct dementia – 10%; – dementia as a result of infarctions in functional (strategic) areas (hippocampus, thalamus, angular gyrus, caudate nucleus) (the term “focal form of vascular dementia” is sometimes used) – 5–10%; – diseases of small vessels with dementia (subcortical dementia, lacunar status, senile dementia of the Binswanger type) – 67%; – hypoperfusion (ischemic and hypoxic); – hemorrhagic dementia (as a result of chronic subdural hematoma, subarachnoid hemorrhage, cerebral hematomas); – other mechanisms (often a combination of the listed mechanisms, unknown factors) – 5–10%. However, according to neuroimaging research methods, most patients simultaneously have two or more pathogenetic types of vascular dementia” [I.V. Damulin, 2008]. Criteria for the clinical diagnosis of “probable vascular dementia” [G. Roman et al., 1993]: – presence of dementia; – the presence of clinical, anamnestic or neuroimaging signs of cerebrovascular disease: previous strokes or subclinical episodes of local cerebral ischemia; – the presence of a temporary and cause-and-effect relationship between brain damage of vascular etiology and cognitive impairment. The main symptoms of vascular dementia: – sudden onset; – stepwise progression with plateau periods (depending on the state of cerebral hemodynamics); – presence of focal neurological symptoms; – emotional lability (weakness, violent crying). However, recently much attention has been paid to mixed dementia. For example, a stroke can be considered as a direct cause of dementia in only 50% of patients with post-stroke dementia. In other cases, the nature of the cognitive defect is of a primary degenerative (usually Alzheimer’s) nature of dementia or a combination of vascular and Alzheimer’s changes (mixed dementia) [6]. Diagnostic criteria for mixed dementia [K. Rockwood et al., 2000]: - in addition to the presence of Alzheimer's disease, symptoms such as sudden onset, step-like progression, focal neurological signs and patchy cognitive deficits, consistent with the onset of vascular disease, or - typical Alzheimer's disease with ischemic changes visible on MRI. Such a frequent combination is explained by the presence of common risk factors. Table 2 presents the main risk factors for cardiovascular diseases that can trigger the development of Alzheimer's disease. Most often, dementia with Lewy bodies begins with parkinsonism, which within 1 year (no more) is joined by cognitive impairment (attention most often suffers), quickly reaching the level of dementia and visual hallucinations (maximum severity at night). The main morphological signs of dementia with Lewy bodies are Lewy bodies (consisting of partially destroyed neuronal proteins) - the highest concentration is observed in the cortex of the temporal and frontal lobes, as well as in the basal ganglia - and altered, enlarged neurons (Fig. 4). Parkinsonism in dementia with Lewy bodies: – does not have a clear asymmetry; – bradykinesia; – walking disorders; – postural disturbances (falls). Hallucinations in dementia with Lewy bodies (most often visual) can be either spontaneous (an important diagnostic criterion) or drug-induced (develop during treatment with antiparkinsonian drugs, primarily dopamine agonists). Dementia with Lewy bodies is characterized by fluctuations and severity of motor and cognitive impairment (in 80–90% of cases). Periods of decompensation can last from several days to several months and end with spontaneous improvement (if the disease does not lead to the death of the patient). Criteria for the diagnosis of dementia with Lewy bodies: – obligate sign – progressive impairment of cognitive functions, sufficient in severity to interfere with normal social and professional functions (dementia); – pronounced memory impairment is not necessarily present in the initial stages, but is obvious in the advanced stages; – characterized by the presence of a “frontal-subcortical” component of dementia, for example, impairment of attention, visuospatial abilities, etc. At least two of the following signs are necessary for the diagnosis of probable dementia with Lewy bodies and one – for the diagnosis of possible dementia with Lewy bodies: – fluctuations severity of cognitive impairment, attention, anxiety; – repeated visual hallucinations (detailed, detailed, well-defined); - Parkinsonic motor disorders (not related to the use of antipsychotics). Additional diagnostic criteria: - repeated falls; - transient losses of consciousness; - increased sensitivity to antipsychotics; - illusions; - hallucinations of other modalities (not visual). Diagnosis of cognitive disorders is based on subjective complaints of the patient, a survey of his relatives, assessing neurological status, the results of neuropsychological testing and data of CT/MRI research. The following tests are recommended as a screening study of cognitive disorders: “5 words” [D. DUBOIS, 2002], Schulta test and watch test test [S. Lovenstone et S. Gauthier, 2001], and for a more complete assessment of the degree of impaired cognitive functions and forming a syndromic diagnosis - a brief scale for assessing the mental status (English - me - mectal stat Examination (MMSE), M. Folstein et al., 1975) and Battery for frontal dysfunction (English Frontal Assessment Batter - Fab, B. Dubois et al., 1999). As an example, the results of the test of drawing watches with dementia are presented (Fig. 5). In addition to neuropsychological tests, clinical scales are used to diagnose cognitive disorders: the clinical rating scale of dementia (sininical dementia rating, J. Morris, 1993) and the total scope of violations (English. Global Deterioration Scale, B. Reisberg et al., 1982). The vascular genesis of dementia is confirmed using the ischemic scale of Khachinsky. Table 3 and in figures 6–7 presents CT/MRI - signs of Alzheimer's disease and vascular dementia and dementia with Levy Taurus. The most promising diagnostic method of dementia is positron -emission tomography (PET), which allows to obtain functional images that reflect the processes of the brain of the brain at the molecular level, including glucose metabolism and oxygen utilization, estimate of blood flow and perfusion, assessment of concentration and affinity of specific receptors. At the end of 2003, the Swedish researchers managed to make a reliable diagnosis in the early stages of Alzheimer's disease for the first time in the world for the first time in the world (Fig. 8). The therapy of cognitive disorders in old age should be aimed, firstly, to the prevention of the increase in cognitive disorders, and secondly, to reduce the severity of existing disorders. Prevention is especially important at the initial stage when effective measures can prevent or delay the development of dementia. It is necessary to reduce the risk of brain ischemia (adequate therapy of arterial hypertension, heart pathology and diabetes should be carried out) [7]. Kivipelto et al. (2006) proposed a scale of risk of developing dementia, depending on the severity of risk factors (Table 4). Treatment of dementia drugs with proven effectiveness (level A): - antagonists of NMDA receptors; - Inhibitors of cholinsterase. Drugs with alleged effectiveness (level B or C): - holinomimetics; - drugs with a neurotrophic effect; - Ginkgo Biloba [2]. As you know, the main neurochemical mechanism for the development of dementia (especially Alzheimer's disease) is a pronounced degeneration of cholinergic neurons and, accordingly, a significant decrease in acetylcholine levels in the brain. At the same time, the severity of cholinergic disorders correlates with the degree of dementia, the death of neurons, as well as the number of senile plaques and neurofibrillar balls. The data of the latest experimental studies have shown that it is the deficiency of central holinergic systems that can lead to the deposition in the brain of the pathological protein of the B - amyloid in the form of senile plaques. Increasing the concentration of acetylcholine in the brain, in turn, contributes to the growth of neurons and an increase in the number of synapses, i.e. It has a pronounced neuroplastic effect. As a result of this, cholinergic pharmacotherapy today can be considered as the prevention and treatment of dementia (primarily diseases of Alzheimer, vascular dementia, etc.). Currently, for these purposes, Cereton (Kholina Alfoscerate) is widely used - central holinomimetics. Kholina Alfoscerate is the predecessor of acetylcholine and phosphatidylcholine. The drug contains 40.5% metabolically protected choline. Metabolic protection helps the release of choline in the brain. When choline enters the body, alphascerate is broken down under the influence of enzymes on choline and glycerophosphate. Kholin is involved in the biosintase of acetylcholine, glycerophosphate is the predecessor of phosphatidylcholine membranes of neurons. In order to objectively assess the dynamics of the functional state of the brain in the treatment of Holin alfoscerate, patients suffering from Alzheimer's disease, S.E. Zhigulskaya from Soyav. (2001) conducted a quantitative study of EEG. As the results of the study showed, cholinergic stimulation can help restore the pattern of the organization of bioelectric activity of the brain, which is an additional evidence of the effectiveness of alphasal alphascrate in the treatment of dementia. In another study [T.N. Batysheva with co -author, 2009] The use of Cereton at a dose of 4 ml (1 g of alphas of alfosecrates) every day intramuscularly over 15 days contributed to improving the condition of patients with moderate cognitive disorders, which was confirmed by the results of neuropsychological research using the test of a mini -study of mental status (MMSE) . At the same time, the increase in the test indicators was an average of 1.5 points (p <0.05). O.S. Levin with Soavt. (2009) conducted an open 10 -day study of Cereton's therapeutic effect of piracetam in case of violation of cognitive functions. So, when using Cereton, it is significantly more often than when using piracetam, an improvement in the state of cognitive functions was noted (40 and 25%, respectively) (p <0.05). In order to assess the effectiveness of Cereton in case of violation of cognitive functions in patients who have undergone a stroke, we conducted our own study [S.P. Markin Sub., 2009]. It was attended by 19 patients aged 47–59 years old who suffered ONMK (2-3 weeks after an acute period). The assessment of cognitive functions was carried out in dynamics using the “5 words” test, the test of “drawing watches”, MMSE and the batteries of lobular dysfunction (BTLD). All patients received Cereton at a dose of 4 ml intravenously daily for 15 days. As the results of studies have shown, the use of Cereton in the early recovery period after a stroke helps to improve cognitive functions, which was confirmed by the positive results of the implementation of neuropsychological tests (Table 5). Figure 9 as an example presented the result of the test of “drawing a watch” by the patient D. before and after treatment with Cereton. How to evaluate the effectiveness of therapy? - cognitive indicators (dynamic study using neuropsychological scales every 6 months (according to MMSE, the average reduction in the estimate of 2.75 points in Alzheimer's disease, 1.75 points - with vascular dementia per year); - affective and behavioral indicators (stabilization of affective status and a decrease in the assessment on a neuropsychiatric scale); - functional indicators (improvement and stabilization of functional status - everyday activity); - neuroimaging indicators. Rehabilitation of cognitive impairment in patients with dementia: - training aimed at improving memory; - programs based on listening music, regular dancing classes; - programs aimed at increasing the active activity of sick houses (in particular, cooking); - art therapy (Fig. 10). Thus, the main goal of treating elderly patients with cognitive disorders is to improve the “quality of life”. To be a healthy elderly person means ignoring your illness ”(I. Shevelev).
Literature 1. Artemyev D.V., Zakharov V.V., Levin O.S. Aging and neurodegenerative disorders: cognitive and motor impairment in old age. Methodological recommendations - M., 2005 - 48 p. 2. Damulin I.V. Therapeutic possibilities for Alzheimer's disease and vascular dementia //Russian Medical Journal - M., 2001 - No. 7-8 - P. 310-313 3. Damulin I.V. New neuroprotective and therapeutic strategy for dementia: NMDA receptor antagonist akatinol memantine // Russian Medical Journal - M., 2001 - No. 25 - P. 1178–1182 4. Zakharov V.V. Age-related cognitive impairment. Methodological recommendations - M., 2004 - 12 p. 5. Zakharov V.V., Yakhno N.N. Syndrome of moderate cognitive impairment in old age: diagnosis and treatment //Russian Medical Journal - M., 2004 - No. 10 - P. 573–576 6. Levin O.S. Discirculatory encephalopathy: modern ideas about the mechanisms of development and treatment - M., 2006 - 24 p. 7. Markin S.P. Modern approach to the prevention of cerebral strokes. Methodological recommendations - Voronezh, 2004 - 43 p. 8. Markin S.P. Impaired cognitive functions in medical practice. Methodological manual - Voronezh, 2008 - 42 p.
First signs of dementia
- Both long-term and short-term memory are impaired. It becomes difficult for a person to remember events that happened recently or remember new information.
- A person loses the skills of orientation in space and time. It is not uncommon for patients to become lost even in areas familiar to them.
- Indifference to once-loved activities appears, and the desire to learn new things disappears. This happens because the brain is no longer able to receive and process information.
- Reducing the criticality of one's own perception. Usually this symptom appears when planning the next period of life.
- In the future, both the progression of these symptoms and the appearance of others, more powerful in their effects, are noted. One of the clear hallmarks of dementia is that a person lives in his past.
At the earliest manifestations of the disease, it is important to promptly consult a therapist or general practitioner. If necessary, he will refer the patient to a specialist (neurologist, psychiatrist or geriatrician).
Active life
There are no strict indications for professional sports, especially if your health condition does not allow you to perform intense cardiological and strength training. An active life means spending more time outdoors, regular walks, Nordic walking, jogging, quad biking, etc. Exercises are selected taking into account the physical fitness and activity of the person.
Living off the beaten track will help you avoid dementia and maintain a healthy brain. Air pollution is further reflected as heavy metals accumulate and come into contact with harmful compounds. Cases of “silent” strokes are often recorded, when the patient is unaware of a change in tissue that has already occurred.
In the early stages of dementia, the following factors are important:
For a person with dementia, it is important to create a quiet, homely, familiar atmosphere. Moreover, the circle of people with whom he communicates must be constant. This will eliminate feelings of anxiety, nervousness, confusion and excitement. It’s a good idea to create a daily routine and stick to it strictly.
Lyudmila Zhilevich: “Unfamiliar faces, new situations that a person is no longer able to remember, can provoke an acceleration of the development of the disease, and also negatively affect his condition.”
The first symptoms of dementia are not a reason to give up exercise. This could be walking in your favorite places, simple work in the garden, physical therapy exercises (at least 150 minutes of anaerobic exercise weekly).
Life should be full of various events and types of intellectual activity. You can read, solve crosswords and scanwords, play chess or checkers, discuss past cultural or political events.
It is important for the patient to have a hobby, but it should not only be a source of positive emotions and bring pleasure, but also stimulate cognitive and mental abilities.
A sick person's diet should contain foods that lower cholesterol levels. For example, barley, legumes, blueberries. Instead of butter, it is better to give preference to vegetable oil. The menu can include fermented milk products, lean meats and poultry, lean fish, seafood, and sauerkraut. To improve the taste of dishes, the use of seasonings (sage, cinnamon, turmeric, saffron) is allowed. But it is better to reduce salt consumption to a minimum. You should definitely drink the daily amount of clean water (at the rate of 30 ml per 1 kg of weight). It is better to cook by steaming, you can bake or boil.
If you follow all the doctor’s recommendations, you can slow down the progression of the disease, which means significantly improving the patient’s quality of life and delaying severe manifestations of dementia. At the same time, people who have a hereditary predisposition to developing the disease should pay special attention to prevention: lead a healthy lifestyle, do exercises daily for mental exercise, and control blood cholesterol levels.
An important point is to create comfortable conditions so that a person suffering from dementia remains independent for as long as possible. The best therapy is to spend more time with elderly relatives, surround them with love, care, and help them feel useful and needed, the specialist added.
The onset of dementia - how to recognize?
For now, this disease is considered irreversible and incurable. That is why it is so important to notice its first signs, warning signs. Don't think that memory loss is a normal age-related phenomenon. This is a problem that needs to be addressed. The first signs of dementia in women have their own characteristics - innate female emotionality will help to track them.
Irritability, strange laughter, or, conversely, tearfulness are noticeably manifested. Outbursts of aggression are possible, the mood changes too sharply and noticeably. Ordinary depression, to which women are also more susceptible than men, lasts longer and is more severe. And suddenly you notice next to you another, new personality of a previously well-known person. And these are not just changes - this is a breakdown in development.
A person suffering from dementia becomes suspicious and suspicious to the point of morbidity, incredibly, illogically stubborn, denies his disorder and does not want to accept help. Countless reproaches are poured down on loved ones - you are inattentive, callous, do not care, you are up to no good. It is very important that loved ones, especially the husband, immediately react to this as an illness, and not as a reason for scandals and showdowns. Watch out! Your beloved mother or grandmother needs help. You will have to insist on consulting a doctor. Early diagnosis is needed.
Useful exercises for brain training
Special exercises can help to stimulate the brain cognitively. They can be performed independently or together with your loved ones. The main condition is their regularity.
Here are some examples of effective activities:
Place in front of you a piece of paper with a list of words written in different colors. You should start with the first word. But you need to name the color in which the text is written. After you reach the end, the words must be repeated in reverse order. It can be difficult at first, since different hemispheres of the brain are responsible for the perception of text and color.
Benefit: helps to establish new connections between the hemispheres of the brain, and also trains concentration and attention switching.
When performing this exercise, you should focus on the number “19” in the center of the square. Then you need to look for “1” and then all the other numbers in ascending order. You can draw the table yourself, and arrange the numbers in the cells in any order. This activity increases the speed of perception and processing of information and promotes the development of peripheral vision.
In older people, thinking, memory and speech are directly dependent on hand movements. In this regard, activities such as knitting, embroidery, or other activities that involve fine motor skills are helpful in maintaining mental clarity.
Fold the fingers of your right hand so that they show the “peace” sign, and show “ok” with the fingers of your left hand. Then, take turns changing your finger shapes so that your left hand shows “peace” and your right hand shows “ok”. Repeat several times. Then try doing this exercise with your right and left hands at the same time. Such gymnastics trains attention and the ability to quickly switch from one task to another.
Take two blank sheets of paper and two pens. The task is to draw geometric shapes with both hands at the same time. Instead of shapes, you can write letters or words with the same set of letters. Synchronous writing trains the brain to cope with several tasks simultaneously, involving both hemispheres in the work.
A Sober Look at Dementia
Unfortunately, modern medicine does not yet know how to treat this disease, to which both residents of backward countries and those who belong to the “golden billion” are equally susceptible. But it seems we are getting closer to discovering its true causes and treatments. For now, all you can do for yourself and your loved ones is to closely monitor your mental health, emotional and behavioral reactions. You can also establish a healthy, fulfilling lifestyle, which will also push back the threat of dementia.
Dementia, like cancer, is one of the so-called “diseases of civilization.”
Humanity has learned to extend lifespan, but has not fully mastered the skills of extending health and vigor.
Today, every three seconds on our planet, someone develops dementia. The main thing you must remember is that timely detection of dementia and timely treatment will prolong the time when the patient is able to care for himself, maintain the ability to self-care, as well as partial mental and mental health.
Types of dementia and causes of its development
Depending on the causes of dementia, there are several types of this syndrome:
- Dementia due to diseases of the nervous system (also called atrophic). It develops due to damage to brain cells in Parkinson's disease, Alzheimer's disease, Pick's disease and other pathologies. This type also includes dementia with Lewy bodies - pathological formations of a protein nature inside nerve cells.
- Vascular dementia. Its cause can be pathologies of cerebral vessels - from arterial hypertension to stroke.
- Mixed. This type includes dementia that occurs due to a combination of several diseases or risk factors.
Also, the causes of dementia include poisoning with potent drugs and metal salts, metabolic disorders (including diabetes), infectious brain lesions, injuries and tumors, and severe alcohol addiction. These reasons are listed in the medical manual “Dementia” (edited by Academician N.N. Yakhin).
All pathologies and factors have one thing in common: they destroy brain cells. Moreover, the lesion can be focal, because the diseases affect different lobes of the main organ of the nervous system - frontal, temporal, parietal, etc. Depending on the cause and nature of the lesion, the complex of symptoms may also differ when comparing the clinical picture of several patients.
What to do in this situation?
Of course, as I already said, the leading factor from a medical point of view that we can offer for such patients is prevention. And preventing dementia is much more effective than treating it.
In order to prevent dementia, in addition to timely diagnosis, it is very important to monitor the lifestyle, monitor the diet of such patients and monitor basic vital signs: cholesterol, blood pressure, pulse.
It is very important to rule out injuries, treat infections in a timely manner, and not let them get worse. Any rise in blood pressure or sugar or glucose may be a harbinger of just such a dementia process, that is, try to exclude such phenomena.
And of course, psychological prevention is very important. For such patients, a comfortable family environment is important. If this does not work, you should contact a family therapist or psychotherapist in order to restore a prosperous psychological atmosphere in the family where the elderly person lives.
The daily routine is very important, sufficient, long, deep sleep is extremely important, which is also sometimes impossible without the participation of psychiatrists.
It's good to train your brain. There are a lot of cognitive trainings, but the most effective training, from my point of view, is solving crossword puzzles.
In addition, participation in some events, holidays, family celebrations, communication as much as possible, that is, to exclude that isolation where the brain rests, where life does not make any demands on the brain, and accordingly it begins to wither.