Vestibular rehabilitation therapy
Fortunately, most of us go about our daily lives oblivious to the complexity of our body's systems that keep us upright and balanced.
But this only happens until, for some reason, our coordination and balance are disrupted, reminding us how vital simple everyday tasks are. Vestibular Rehabilitation Therapy (VRT) consists of a set of exercises that encourage the brain and spinal cord to restore imbalances that occur due to diseases or abnormalities of the vestibular system or damage to the central nervous system.
This guide will help you understand:
- anatomy of the vestibular system
- why do we need ART?
- What disorders does ART usually treat?
Organ of balance
To understand how to treat the vestibular apparatus, it is necessary to become familiar with its structure and functions. It is located in the inner ear and is part of a complex mechanism that provides balance to the body and allows us to navigate space. When tilting/turning the head, the receptors of this organ are irritated. As a result, the muscles that help straighten the body contract. Every day our body is exposed to a huge number of irritants, so it gets used to them. However, for some people they cause problems with the vestibular system that require treatment.
Anatomy
The anatomy and physiology underlying the human body's sense of balance is complex. Many systems are involved, including the brain, spinal cord, eyes, ears, and receptors in the skin, joints, and muscles. Impairment in any of these areas due to injury or illness can negatively impact your sense of balance.
The inner ear, also called the labyrinth, consists of the semicircular canals along with the saccule and the uterus. Collectively, this inner ear system is called the vestibular system or vestibular apparatus.
The inner ear also contains the cochlea, which is the main structure involved in hearing perception.
The three semicircular canals respond to rotational movements of the head. The canals are located at 90 degrees to each other and are filled with a fluid called endolymph. Hair cells are located at the base of each semicircular canal and project into the endolymph. The movement of the head causes movement of the endolymph in the channels, which in turn causes the hair follicles to move accordingly and emit impulses about balance that travel to the brain. Hair cells in the sac and utricle respond to linear acceleration of the head, such as when riding in an elevator or moving forward.
Sensory information from the inner ear is transmitted to the brain through the vestibular portion of the eighth cranial nerve, which is also called the vestibulocochlear nerve. The cochlear part of the nerve transmits hearing information. Certain areas of the brain, particularly the cerebellum and brain stem, as well as parts of the cerebral cortex, process sensory information coming from the inner ear. When both the right and left inner ears send the same information to the brain, the body is balanced. When the body or head moves, the sensory information from the ears is not identical, so the brain perceives the movement and the body adjusts accordingly.
The ears work closely with the eyes to maintain balance. The basis of this is
vestibulo-ocular reflex (VOR). This is an automatic function of the eyes that stabilizes images on the retina in response to head movements. This reflex causes the eyes to move in the opposite direction to the movement of the head so that the eyes remain stationary on the observed target. Thus, precise information from the vestibular system influences the sense of balance.
If one inner ear is affected by disease or injury, then sensory information sent to the brain will falsely indicate movement from that vestibular system. In this case, the eyes will adjust accordingly and move opposite to the perceived movement despite the fact that the head is actually stationary. The result is involuntary back and forth eye movements. This eye movement is called nystagmus and, if present, makes any healthcare professional suspect a vestibular problem.
There are two other reflexes, the vestibulocervical reflex and the vestibulospinal reflex, which also help the body maintain a sense of balance.
The vestibulocervical reflex works in conjunction with incoming vestibular information and the neck muscles to stabilize the head. And the job of the vestibulospinal reflex is to create compensatory movements of the body in response to vestibular input in order to maintain balance and avoid falling.
Disturbance along any part of the anatomical pathway described above can affect the perception of balance or equilibrium. A problem with the part of the inner ear or sensory information transmitted to the brain through the vestibulocochlear nerve is called peripheral vestibular disorder.
If a problem affecting balance is due to damage to a structure within the brain itself, which then affects the reception and integration of balance information, it is called a central vestibular disorder.
Common disorders treated with ART
The most common peripheral vestibular disorders treated with ART are benign paroxysmal positional vertigo (BPPV) and any injury or disease that results in decreased function of the inner ear. This decreased function may be associated with disorders such as Meniere's disease, vestibular neuritis or labyrinthitis, or acoustic neuroma. The term unilateral or bilateral vestibular hypofunction can be used to describe decreased function of the vestibular system in one (unilateral) or both (bilateral) ears due to disease or injury.
Clinically, any peripheral dysfunction in the vestibular system that affects balance can potentially be treated with ART, however the effectiveness of treatment will depend on the exact cause of the vestibular problems.
Central vestibular disorders such as multiple sclerosis or stroke may also respond to ART, although in general peripheral vestibular disorders tend to respond better.
Benign paroxysmal positional vertigo (BPPV)
BPPV is a common clinical balance disorder characterized by recurrent attacks of dizziness that are brief in nature (usually 10-60 seconds) and most often triggered by certain head positions. Benign, in medical terms, means that it is not life-threatening. Paroxysmal means that it occurs with rapid and sudden onset or worsening of symptoms.
BPPV is the most common cause of recurrent dizziness. BPPV is thought to be caused by calcium carbonate crystals (called otoconia, otoliths, or “ear stones”) in the semicircular canals of the inner ear. Under normal circumstances, these crystals are located within the sac of the ear, but in BPPV, these crystals are thought to dislodge and migrate into the semicircular canals of the ear. This misalignment is thought to have a number of possible causes, such as ear or head trauma, ear infection or surgery, or natural degeneration of the inner ear structures. Often, however, the direct cause cannot be identified.
Otoconia settle in one place of the canal when the head is motionless. The most common canal to be affected is the posterior semicircular canal. A sudden change in head position, often caused by actions such as rolling over in bed, getting out of bed, tilting the head, or looking up, causes crystals to shift. This shift, in turn, sends false balance signals to the brain and causes dizziness.
Dizziness due to BPPV can be severe and accompanied by nausea. The attacks may occur for seemingly no reason and then disappear for several weeks or months before returning again. BPPV usually affects only one ear, and although it can occur at any age, it is often seen in patients over 60 years of age and is more common in women. Nystagmus is usually present.
Meniere's disease
Meniere's disease is a chronic, incurable vestibular disorder characterized by symptoms of episodic severe dizziness, fluctuating hearing loss, ear fullness and/or ringing in the ear (tinnitus), and nystagmus.
This disease gets its name from the French physician Prosper HaMeniere, who in the late 1800s theorized the cause of these symptoms, which he noted in many of his patients.
The exact cause of Meniere's disease has not yet been determined, but it is thought to be due to an abnormal amount of endolymphatic fluid accumulating in the inner ear and/or an abnormal accumulation of potassium in the inner ear.
The early stages of acute attacks of Meniere's disease vary in length from 20 minutes to 24 hours. The attacks may occur regularly over the course of a week or may occur weeks or months later. Other symptoms may coincide with an attack, such as restlessness, diarrhea, shaking, blurred vision, nausea and vomiting, cold sweats, and a rapid pulse or racing heart. After attacks, patients often experience extreme fatigue that requires many hours of rest to recover. For some patients, the time between attacks may be symptom-free, but other patients report persistent associated symptoms even between attacks.
Vestibular neuronitis
Vestibular neuronitis is an inflammation of the inner ear or its associated nerve (the vestibular portion of the vestibulocochlear nerve) that causes dizziness. Hearing may also be affected if the inflammation also affects the cochlear nerve.
Dizziness caused by vestibular neuronitis has a sudden onset and can be mild or extremely severe. Nausea, vomiting, unsteadiness, decreased concentration, nystagmus, and blurred vision may also occur. Most often, infections that cause inflammation of the inner ear or vestibulocochlear nerve are viral rather than bacterial. Proper diagnosis as to whether it is viral or bacterial is important to ensure the most effective and appropriate treatment.
Acoustic Neuroma
An acoustic neuroma is a benign tumor on the vestibulocochlear nerve. Early symptoms include hearing loss in the affected ear, ringing in the ear (tinnitus), dizziness, and a feeling of fullness in the ear. The tumor grows slowly, so symptoms appear gradually and can be easily missed in the early stages. As the tumor grows, it can press on other nerves in the area, and symptoms such as a headache or pain and numbness in the face may occur. Dizziness or other balance problems may occur as the tumor grows.
Vestibular symptoms
Peripheral or central vestibular disorders can lead to a number of different symptoms. VRT can potentially relieve or resolve any symptoms associated with a vestibular disorder.
Common symptoms include:
- dizziness
- blurred vision
- fatigue
- anxiety
- headache
- nausea and/or vomiting
- cold sweat
- ringing/tinnitus
- hearing loss
- twitching orbital stagmus
- ear pressure
- panic attacks
- leaning to the side
- fear of falling
- increased risk of falls
- imbalance
- unsteady walk
- anxiety
- depression
What diseases cause vestibular disorders?
Vestibular disorders have the following causes:
1. People aged 60 years and older often experience benign positional vertigo, which occurs against the background of traumatic brain injury, otitis media, and ischemia. However, there are cases where the exact reasons were not established.
This vestibular disorder is characterized by the following symptoms and external signs: a person changes his body position in bed (lays down, stands up, turns around), and he experiences a short-term attack of dizziness. In most patients, the exacerbation phase (attacks of dizziness occur quite often) is replaced by a spontaneous long-term remission.
To confirm the diagnosis, special so-called positional tests are used - the person changes the position of the head, and doctors record when nystagmus and dizziness occur.
The appearance of this disease is facilitated by the formation of otoliths in the posterior semicircular canal. The force of gravity acts on the otoliths, and they shift, irritating the vestibular receptors of the dome, which leads to dizziness. This condition can last for a very long time without the manifestation of any other disorders.
Treatment of this vestibular disorder with traditional medications often does not produce the desired effect. In cases where the body is particularly resistant to certain medications, surgical intervention is indicated. Severe outbreaks of positional vertigo have another cause - the loop of the anterior inferior cerebellar artery compresses the vestibular nerve, which leads to decreased hearing sensitivity, tinnitus and hyperacusis. Taking carbamazepine (finlepsin) usually helps to relieve the manifestations of this disease, and in cases of ineffectiveness of the drug, a procedure such as microvascular decompression of the nerve is used. Drinking alcohol leads to changes in endolymph density, and this can also cause dizziness.
2. Another fairly well-known cause of dizziness is vestibular neuritis. It is caused by damage to the vestibular nerve or peripheral vestibular apparatus. People of all ages are susceptible to the disease. It is often preceded by infectious diseases affecting the upper respiratory tract. In this case, the following symptoms of the disease and its external signs are distinguished: sudden rotational movements of the head cause an attack of dizziness, vomiting, and a feeling of nausea. The presence of horizontal rotatory nystagmus is observed. An important fact is that in the case of this disease, the nystagmus has only a unilateral direction, while in the case of a bilateral one, we are talking about a different diagnosis. Vestibular neuritis is characterized by the absence of other neurological symptoms (for example, decreased hearing sensitivity). Attacks of severe dizziness, accompanied by repeated vomiting, last in the patient for 3-4 days, but complete remission occurs only after a few weeks. In cases where the patient’s condition does not improve within a month, he is sent to magnetic resonance or computed tomography for additional research. Mild cases of the disease do not require hospitalization; outpatient treatment is quite possible. At the initial stage, short-term treatment with corticosteroids is often prescribed - they reduce vestibular symptoms. The positive effect and improvement in the patient’s condition provide grounds for discontinuing medications and prescribing special exercises to strengthen the vestibular apparatus.
3. The root cause of vestibular disorders in older people with a history of vascular diseases is often vertebrobasilar insufficiency. It can be caused by pathologies such as ischemia of the labyrinth or vestibular nerve or trunk. This vestibular disorder is characterized by the acute development of an attack of dizziness, the presence of disturbances in the functioning of the vestibular system, vomiting, and a feeling of nausea. In some cases of ischemia of adjacent sections of the trunk, other external signs are observed - a person may suddenly fall, he is disoriented, his vision is impaired, his limbs become flaccid and numb.
The occurrence of vertebrobasilar insufficiency can also be caused by some other reasons: atherosclerosis of the arteries, sometimes cardiogenic embolism, increased blood viscosity, vasculitis. To accurately diagnose this disease, it is necessary to take into account the symptoms of various concomitant diseases in the medical history, namely arterial hypertension (high blood pressure), diabetes mellitus, hyperlipidemia. The entire course of treatment for vertebrobasilar insufficiency is primarily aimed at correcting or eliminating risk factors, and includes taking antiplatelet and vasoactive drugs.
4. Blockage of the internal auditory artery is one of the most persistent types of vertigo. The most common external sign of this disease is hearing loss. Cerebellar ataxia and nystagmus, coupled with an acute attack of dizziness, may indicate hemorrhage or cerebellar infarction. And in these cases, emergency intervention is required, since we are talking about human life and death. The initial stage of cerebellar stroke is very similar to vestibular neuritis. And they differ in nystagmus, which in this disorder is bilateral or vertical. The patient is also unable to stand without assistance.
5. Slowly increasing imbalance and moderate dizziness indicate chronic bilateral vestibulopathy. The cause of the disease can be intoxication of the body with certain types of medications. Timely discontinuation of the medication helps restore vestibular function. If this is not done in time, the process becomes irreversible. Various types of solvents, chemicals, and loop diuretins can also sometimes cause a vestibular disorder called chronic vestibulopathy.
6. Here are the known symptoms of Meniere's Disease: dizziness that occurs occasionally, congestion and tinnitus, accompanied by a decrease in hearing sensitivity. An acute attack of dizziness reaches its maximum in a few minutes and regresses in the following hours. At the very beginning of the disease, the process of hearing loss can be stopped. But each subsequent attack leads to the fact that hearing sensitivity becomes lower and lower. In this case, constant tinnitus appears, which intensifies before the onset of an attack and during it. Some patients may fall suddenly without losing consciousness. The reason for this is a sharp increase in pressure in the inner ear and, as a result, irritation of the vestibular receptors. In the process of diagnosing this vestibular disorder, the main condition is the exclusion of other diseases, for example, SLE, neurosyphilis or hypothyroidism.
7. Injuries to the skull and head can often become a source of post-traumatic vertigo. This occurs due to concussion of the labyrinth, the formation of a perilymphatic fistula, or a violation of the integrity of the temporal bone.
8. There are a number of other ear diseases that can cause vestibular disorders. These include: common wax plugs in the ears, Eustachian tube dysfunction, otosclerosis. Otitis media in acute form can also cause dizziness, especially if it is complicated by purulent processes in the labyrinth.
9. One of the rather rare and infrequent causes of dizziness is a tumor of the cerebellopontine angle. A gradual and slow process of hearing loss, as well as constant tinnitus, indicate a disease such as acoustic neuroma.
10. Let us note another cause of vestibular disorders - basilar migraine. Girls in the prepubertal period are most susceptible to migraine dizziness and pain. They last no more than an hour and are relieved by taking anti-migraine medications.
11. Short-term attacks of dizziness can also occur with epilepsy. But along with them, other symptoms of an epileptic seizure are usually observed: motor, autonomic or sensory, and a disturbance of consciousness is necessarily present.
12. Craniovertebral anomaly - we are talking about it when attacks of dizziness are combined with nystagmus and impaired speech and swallowing functions. Symptoms such as vomiting, nausea, dizziness with rotational movements of the head can signal the initial stage of multiple sclerosis.
Diagnosis of the cause of dizziness
A detailed history of your medical condition is the most important information your doctor needs to diagnose the cause of your vestibular disorder and then administer appropriate ART.
The doctor will ask you to describe your vestibular symptoms in detail. Any symptoms you experience above or others should be mentioned. Your doctor will want to know when the first episode of your symptoms occurred, how long they lasted, and whether they were related to any other events, such as a car accident, head injury, illness, or infection.
He will also want to know how often symptoms have recurred since the first episode and the general pattern of symptom frequency. Find out exactly what causes your symptoms, such as moving your head in a certain direction or getting out of bed. For dizziness, your doctor will ask about the nature of what you're feeling and whether you experience episodes of true dizziness where you have a spinning sensation.
The doctor will also want to know if there is anything that reduces or increases your symptoms, and if you are taking any medications, or if you have a family history of any inner ear disorders or central nervous system disorders.
He may ask you to rate the intensity of some of your symptoms on an objective scale. Finally, they will ask about all the daily activities that are related to your vestibular problem, such as walking, driving, working, and even household activities such as dressing, bathing, showering, and housekeeping.
He will also want to know if you have any falls.
The doctor will examine your eye movements by asking you to follow certain objects with your eyes or by asking you to move your head while keeping your attention on a specific target.
An examination of the joints and neck muscles is also carried out to determine the cervicogenic nature of dizziness.
Finally, your doctor may ask you to fill out a questionnaire to determine the intensity of your vestibular symptoms.
Depending on what the doctor finds during the initial examination, they may send you for a series of other tests to further determine the cause of your vestibular symptoms.
Vestibular rehabilitation
As stated above, ART can be used to treat various disorders that cause dizziness or balance problems. Almost any disorder that occurs due to vestibular dysfunction and does not receive sufficient compensation can be treated with ART. The effectiveness of ART depends on correct diagnosis of the cause of the imbalance, the skill/training of the therapist in developing and administering the treatment, and adherence to the prescribed exercise program.
As explained earlier, the purpose of ART exercises is to encourage the brain and spinal cord to compensate for any balance deficits that arise due to diseases or abnormalities of the inner ear or central nervous system. In other words, patients teach their vestibular system to do one of several things; adapt to the stimuli presented, substitute other sensory pathways, or become accustomed to changing vestibular signals sent to their brain so that they can manage their vestibular disorder and maintain normal functioning despite possible ongoing symptoms.
In some cases, ART can eliminate vestibular symptoms. Unfortunately, however, this is not always the case, so minimizing symptoms or the frequency of recurrence of symptoms is considered a successful outcome of ART.
Research in the field of ART shows that, in general, ART exercises are effective in reducing many symptoms of vestibular disorder and that these improvements can often persist for several months after therapy. However, the effectiveness of therapy often depends heavily on what exactly is causing the vestibular symptoms in the first place and the use of individualized exercises rather than a standard exercise protocol.
ART, however, is not always effective for all vestibular problems. There are even some vestibular problems where exercise is not considered appropriate, so proper diagnosis of the cause of the symptoms is important.
ART exercises
If your physiotherapist feels that ART is right for you after completing your assessment, they will prescribe a range of individual exercises for you to do regularly. These exercises will focus on your specific vestibular problem and associated symptoms.
Additionally, the exercises you are prescribed will focus on any day-to-day problems you are facing as a result of your symptoms. Some exercises will be done with your physical therapist on a stability platform, and others will be retrained so that you can do them on your own as part of a home exercise program.
Medications to treat your symptoms may be an addition to ART and should be discussed with your doctor.
Complaints of dizziness are among the most common in practical medicine. In this case, the patient may have in mind a wide variety of sensations - a feeling of rotation, falling, movement of his body or surrounding objects, a state of lightheadedness, general weakness and a premonition of loss of consciousness, as well as instability when walking and gait disturbance [1-3]. For most diseases accompanied by dizziness, there are typical complaints, symptoms and their combinations.
There are systemic and non-systemic dizziness. Systemic vertigo is also called vestibular or true vertigo, or vertigo. This type of dizziness is manifested by the illusion of rotation of one’s own body or surrounding objects in a certain direction in space, accompanied by vegetative symptoms (nausea, vomiting, increased sweating), a feeling of fear, imbalance and nystagmus. This dizziness can be caused by damage to the vestibular system at both the peripheral and central levels [1–4].
Non-systemic dizziness is observed much more often than systemic vestibular dizziness. It is not always associated with damage to the vestibular system, it is not characterized by hearing loss, and, as a rule, nausea and vomiting are not observed [1-3].
The causes of recurrent systemic vertigo can be a variety of diseases: Meniere's disease, benign positional paroxysmal vertigo, vestibular neuronitis, perilymphatic fistula, labyrinthitis, peripheral vestibular syndrome of toxic origin, trauma to the labyrinth or vestibular-cochlear nerve, tumor of the cerebellopontine angle or vestibular-cochlear nerve.
Patients with complaints of dizziness are often diagnosed with vertebral artery syndrome due to osteochondrosis of the cervical spine.
There is a group of patients with recurrent severe rotational vertigo, accompanied by tinnitus, vomiting, and falling, whose attacks are short-lived, occur for no apparent reason or when the position of the head changes, but are repeated many times over a certain period of time. Outside of attacks of dizziness, as a rule, no deviations in vestibular function are detected, and hearing loss is rare. Some authors have suggested that such cases be associated with neurovascular compression of the vestibulocochlear nerve.
T. Brandt et al. [5] described several observations of patients with short-term paroxysms of dizziness and called them peripheral vestibular paroxysms. According to their data, carbamazepine was effective in all cases. There are no objective data on the frequency of this form of dizziness, since this syndrome is interpreted either too broadly or too narrowly. Difficulties in making this diagnosis are due to the lack of description of this pathological condition in the domestic literature. We present our observation.
Patient S., 60 years old, individual entrepreneur, upon admission complained of attacks of rotational dizziness directed clockwise, accompanied by noise in the right ear, vomiting, falling to the left without loss of consciousness. When examined outside an attack: there is no spontaneous nystagmus, the reflexes of oral automatism are animated, the nasolabial folds are symmetrical, the tongue is in the midline, swallowing and phonation are not changed. No facial sensitivity disorders or impaired sense of smell were noted. Tendon-periosteal reflexes are equal, strength in the limbs is sufficient, no pathological reflexes were detected. She is stable in the Romberg position and performs coordination tests without intention. Gait is not impaired. Hearing SR 6 m in both ears. Blood pressure 110/80 mm Hg. Art., pulse 76 per minute, rhythmic.
History of the disease: in August 2010, acutely, for no apparent reason, noise appeared in the right ear; within a few minutes, severe clockwise rotational vertigo developed; a fall to the right side was noted without loss of consciousness. The attack regressed within a few hours. Similar attacks were repeated subsequently 2-3 times a year, lasting up to 1-2 days. Audiometry performed during this period did not reveal any hearing loss. An examination by an otorhinolaryngologist revealed no pathology. In the neurological department at the place of residence, a clinical diagnosis was established: discirculatory encephalopathy stage II with vestibulo-atactic syndrome. In the interictal period she took betaserc and sermion. Since July 2012, for no apparent reason, attacks have become more frequent up to 2-3 times a day, their character has changed: the attack was accompanied by congestion and noise in the right ear, rotational dizziness to the right, unpleasant sensations in the epigastrium, sticky sweat, nausea and vomiting for 2 weeks . The changes detected on MRI of the brain were regarded as signs of foci of gliosis and normal pressure mixed hydrocephalus. She was hospitalized at the Republican Scientific and Practical Center of Neurology and Neurosurgery to clarify the diagnosis and correct treatment.
In order to clarify the diagnosis, an examination was carried out.
An otoneurological examination revealed a decrease in vestibular excitability on the right during caloric tests, which made it possible to interpret the pathological process as peripheral vestibular syndrome on the right.
Pure tone threshold audiometry did not reveal any hearing impairment. Due to the absence of hearing impairments, a hearing test in an extended frequency range, electrocochleography, and a dehydration test were not performed on the patient.
Videonystagmography was performed using a VF5b device (Interacoustics, Denmark), and spontaneous nystagmus to the left with a frequency of 0.7 Hz was detected. A provocative hyperventilation test, as well as a Valsalva maneuver, caused an increase in the frequency of nystagmus to 0.9 Hz and a feeling of dizziness with nausea. The right sinocarotid test induced an increase in nystagmus frequency to 1.1 Hz. The de Klein test on the right caused the appearance of U-shaped wave nystagmus with a frequency of 0.9 Hz without an autonomic reaction. Optokinetic nystagmus to the right is weakened, the vestibulo-ocular reflex is evoked, and the reaction of suppressing it with the gaze is preserved.
A study of acoustic brainstem evoked potentials revealed bilateral deterioration of conduction from the level of the superior olives to the inferior colliculi. Dynamic MRI of the brain using a DISCOVERY MR750W 3.0T device (GE, USA) did not reveal any pathological space-occupying formations in the cranial cavity. The median structures are not changed. In the cerebral hemispheres there are hyperintense foci on T2 mode. The basal cisterns, cerebral ventricles, and cortical sulci are not dilated. The craniospinal junction is unremarkable. Conclusion: multifocal changes in the brain of vascular origin.
The EEG revealed moderately pronounced diffuse changes in the form of disorganization of the cortical rhythm with increased slow-wave activity in the fronto-central leads without clear lateralization. A duplex scan with color and spectral Dopplerography of the brachiocephalic arteries and veins was performed. Echographic signs of stenosing atherosclerotic lesions of the brachiocephalic arteries were revealed: stenosis at the mouth of the right external carotid artery up to 30-40%, at the mouth of the right subclavian artery 30% in diameter, in the bifurcation area of the left common carotid artery 30% in diameter, without hemodynamic disturbances.
X-ray of the cervical spine with functional tests revealed: kyphosis C3-C7, spondyloarthrosis C2-C3, disc chondrosis C2-C4, C4-C7 stage IV, uncovertebral arthrosis C4-C7, spondylosis C3. Lordosis was straightened during extension, block of segments C4-C7, hypomobility of segments C2-C4.
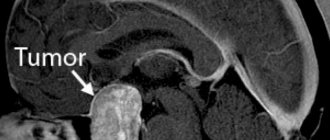
The results of the examination made it possible to confirm the presence of chronic cerebral circulatory failure as part of the clinical diagnosis: dyscirculatory encephalopathy. To clarify the causes of paroxysmal dizziness, a repeat MRI was performed with localization of the area of interest (internal auditory canals) using the FIESTA-C isotope pulse sequence, which made it possible to study the vestibulocochlear nerves in detail. An intimate apposition of the loop of the anterioinferior cerebellar artery to the trunk of the vestibular-cochlear nerve on the right was revealed at a distance of 10 mm from the proximal end and 11 mm from the distal end of the nerve, which allows us to most likely assume a neurovascular conflict (see figure).
Figure 1. MRI of the brain of patient C. The apposition of the loop of the anterior inferior cerebellar artery to the trunk of the vestibulocochlear nerve on the right at a distance of 10 mm from the proximal end and 11 mm from the distal end of the nerve (arrow). MRI using the FIESTA-C isotropic pulse sequence.
Based on the clinical, vestibulometric and neuroimaging examinations with a detailed study of the vestibular-cochlear nerves, the patient was diagnosed with periodic vestibular paroxysm of a mixed nature (peripheral right-sided and cerebellar), caused by a neurovascular conflict (attachment of the anterioinferior cerebellar loop to the vestibular-cochlear nerve on the right) against the background of discirculatory encephalopathy of the first degree.
The patient was prescribed carbamazepine at a dose of 200 mg/day to prevent attacks; no attacks of dizziness were registered during the observation period. To speed up vestibular compensation, nootropic drugs and vestibular gymnastics are also prescribed.
Discussion
The true incidence of vestibular paroxysmia in the population is unknown due to the small number of observations. This syndrome combines clinical signs of various conditions (rotational dizziness with unilateral hearing loss during an attack lasting from several minutes to several days, instability when walking, concomitant autonomic symptoms). All this may cause difficulty in interpreting this disease. Often this pathological condition is regarded as Meniere's disease, benign positional vertigo, postural phobic vertigo, vertebral artery syndrome with cochleovestibular paroxysms, vertebrobasilar insufficiency. Vestibular paroxysm is distinguished when the peripheral part of the vestibular system is damaged and when its central part is damaged [4-6].
To date, diagnostic criteria for vestibular paroxysmia are used [5], which are characterized by the presence of short attacks of dizziness in combination with a number of other signs. Among them:
- the occurrence of an attack of dizziness during hyperventilation, as well as in certain positions of the head (turning to the side, tilting back) and the cessation of the attack when the position of the head changes;
- the presence of objective cochlear disorders that increase during each attack: unilateral hearing loss or noise in the ear, confirmed by audiometry, in the study of auditory evoked potentials, and their decrease in the interictal period;
— violation of static and dynamic balance during an attack;
- absence of brainstem symptoms, central vestibular and oculomotor disorders;
- reduction in the frequency and severity of attacks when taking carbamazepine.
It is believed that vestibular paroxysmia with damage to the peripheral part of the vestibular system, like trigeminal neuralgia, glossopharyngeal neuralgia, myokymia of the superior oblique muscle of the eye, can be caused by compression of the nerve by the vessel [6]. The cause of the attack can be either direct compression of the nerve, or pathological paroxysmal impulse transmission between adjacent axons with foci of demyelination. There is another version of the occurrence of vestibular paroxysm - hyperactivity in the nuclei of the vestibular-cochlear nerve, provoked and maintained by chronic compression of the brain. Some authors do not exclude compression of the vestibulocochlear nerve by malformations or aneurysm of the vessels of the posterior cranial fossa [7, 8]. Sometimes attacks of vestibular paroxysm are caused by tension on the nerve by an arachnoid cyst with prolonged blockade of the nerve or its irritation by the membranes of the cyst [9].
Vestibular paroxysmia with damage to the central part of the vestibular apparatus can be caused by transient cerebellar ischemia, occlusion of the vertebral artery when turning the head, or vestibular epilepsy [10-12].
In the described case, Meniere's disease was evidenced by the absence of a significant decrease in hearing acuity according to the results of audiometry with a disease duration of about 2 years and the presence of attacks of moderate frequency dizziness, as well as the occurrence of attacks when turning the head. Benign positional vertigo is excluded due to the absence of positional nystagmus during the Holpike test. Preservation of asymmetric vestibular excitability (reduced on the left with caloric stimulation) and hearing on both sides testified against neuroma of the vestibulocochlear nerve. Significant vertebrobasilar insufficiency was excluded based on the absence of spontaneous nystagmus and oculomotor disturbances. In addition, the patient did not show any violation of statics and coordination at the time of observation. Central causes of recurrent vertigo, such as vertebral artery occlusion, were excluded by duplex scanning of the brachiocephalic arteries and veins with functional tests. According to the EEG results, paroxysmal forms of activity of typical localization were not recorded, which made it possible to exclude vestibular epilepsy. The evidence against vestibular migraine was the appearance of attacks of dizziness after 50 years in the absence of a history of migraine, and the absence of brainstem and visual disturbances during an attack.
The traditional examination did not allow us to explain the cause of recurrent dizziness. This directed us to search for other causes of unilateral peripheral cochleovestibular syndrome.
In our case, there was precisely compression of the vestibular-cochlear nerve by the anterior inferior cerebellar artery, which was altered due to atherosclerosis, which occurred with clinical features (duration of attacks up to 1-2 days, no hearing loss on the affected side). We have not received data for the second theory of the occurrence of vestibular paroxysms - hyperactivity of the vestibular nuclei. A number of neurophysiological data were also taken into account (atherosclerotic lesions of the brachiocephalic arteries, osteochondrosis of the cervical spine, bilateral deterioration of conduction from the level of the superior olives to the inferior colliculus, multifocal changes in the brain of vascular origin), which determine the background of the underlying disease.
Treatment should be aimed at eliminating the underlying cause, however, the adherence of the loop of the anterioinferior cerebellar artery to the trunk of the vestibulocochlear nerve is not always removable. Methods of decompression and selective neurectomy of the vestibular nerve are used [13, 14], which are not always used after long-term ineffective conservative treatment. Therefore, pathogenetic and symptomatic treatment is of great importance in the treatment of vestibular paroxysmia. The mechanism of the vertigolytic effect of carbamazepine is still unclear, however, according to the literature, long-term use of this drug is effective.
Our approach to treatment (exercises on the stabiloplatform)
Stabilometry is a modern method that allows you to assess the state of a person’s balance in various diseases.
The patient is examined on a special platform that records minimal vibrations of the human body with subsequent computer processing. At the end of the study, a conclusion and recommendations for rehabilitation in the form of training are issued.
With the help of video games, a person, by moving fulcrum points, “guides” the actions of the character on the screen, thereby training his vestibular apparatus. Repeated repetition of such training increases the effectiveness of the therapy.
Treatment on a stabiloplatform with biofeedback is prescribed as part of complex therapy for diseases and pathological conditions such as:
- imbalance, loss of coordination;
- frequent dizziness and headaches;
- diseases of the vestibular apparatus;
- panic attacks accompanied by dizziness
- polyneuropathy;
- vascular diseases, conditions of impaired blood supply to the brain, incl. post-stroke
- various spinal injuries (vertebral displacement, curvature)
- flat feet
Treatment of neck diseases
Some patients who experience dizziness or balance problems also have orthopedic neck problems that cause or worsen their symptoms. In these cases, your physiotherapist at Healthy Sports can also provide hands-on treatment in combination with the other ART exercises described above.
Strategies for self-administration
Secondary damage due to vestibular problems can occur due to frequent falls. As part of your ART, your doctor will talk about simple strategies that can minimize the risk of secondary injuries. For example, you may be advised to use walking aids if you are tired or in a particularly busy environment, such as a grocery store.
Conclusion
ART can be extremely helpful in reducing or eliminating any vestibular symptoms and imbalances you may experience due to diseases or abnormalities of the inner ear or central nervous system. These exercises will lead to the best results if they are prescribed by one of our doctors at the Healthy Sports Medical and Health Complex.
You can undergo an examination at the Healthy Sports Medical and Health Complex, make an appointment by phone: 58-88-28
Dramamine® – a drug for the correction of vestibular disorders
Drug treatment of vestibular apparatus disorders is aimed at stabilizing the balance system and reducing its sensitivity to external influences.
The drug Dramina® blocks the function of transmitting signals to the central nervous system that cause dizziness, nausea and other unpleasant manifestations of motion sickness. The basis of the treatment of vestibular disorders is the removal of excessive irritation of the perceptive structures of the inner ear. Dramamine® is a drug for the relief of symptoms of vestibular disorders, more information about which you can find here.