What is a basal skull fracture?
A basal skull fracture is a very severe traumatic brain injury (TBI) in which one or more of the bones that make up the base of the skull: the occipital, sphenoid, temporal or ethmoid, breaks. The cause of such damage is usually a significant impact: it could be an accident, a fall backward from a height, a direct blow from something heavy to the head or face in the lower jaw area.
Fracture of the bones of the base of the skull accounts for 4% of the number of diagnosed traumatic brain injuries. A combination of fractures of the base and vault of the skull is also possible, which occurs in 50-60% of patients with this injury.
Survival rate for skull fracture
Of decisive importance is how quickly and competently first aid is provided for a fracture and hospitalization with subsequent medical measures is carried out. TBI is often accompanied by heavy bleeding, which can lead to death in the first hours after injury or cause a prolonged coma, the prognosis of which is extremely unfavorable. In this case, there is a high probability of lifelong disability, when basic life functions are impaired and intelligence is seriously affected.
For fractures without displacement, single cracks that do not require surgical intervention, the prognosis is relatively favorable.
The mortality rate for fractures of the bones of the base of the skull ranges from 24 to 52%, depending on the severity and complexity of the injury and its subsequent complications.
Skull fracture: diagnostic methods
Diagnostics is carried out comprehensively and includes the following activities:
- Medical examination and collection of patient complaints. During the examination, the doctor assesses the general condition of the victim, the reaction of the pupils, and measures the pulse and blood pressure. The position of the tongue and the symmetry of the patient’s jaws are also assessed. Neurological reactions are being studied;
- An x-ray of the skull is performed in two projections;
- A computed tomography (CT) or magnetic resonance imaging (MRI) scan is performed.
In extremely severe cases, when it is impossible to conduct a full diagnosis, treatment of the patient is prescribed based on the existing external signs of pathology.
Signs and symptoms of a skull fracture
Symptoms depend on the severity, location of the fracture, and the extent of damage to brain structures. Loss of consciousness can take any form, from short-term fainting at the time of injury to long-term coma. The more severe the damage, the more severe the damage, but with intracranial hematoma there may be a period of lucidity preceding loss of consciousness, which should not be mistaken for the absence or mildness of injury.
Common signs of a fracture include:
- Expanding headaches due to developing cerebral edema;
- Vomiting, aspiration of vomit, or spontaneous leakage of stomach contents into the lungs;
- Symmetrical bilateral hemorrhages around the eyes in the form of “spectacles”;
- Different diameters and lack of pupillary response;
- Respiratory and circulatory disorders in case of compression of the brain stem;
- Leakage of cerebrospinal fluid (cerebrospinal fluid), mixed with blood, from the nose and (or) ears;
- Cardiac disorders: arrhythmia, tachycardia, bradycardia, high or low blood pressure;
- Excitement or immobility;
- Confusion;
- Involuntary urination.
Fractures of the temporal bone pyramid can be longitudinal, transverse, or diagonal. With longitudinal fractures, the middle and inner ear and the facial nerve canal are affected. Symptoms: bleeding from the ear and leakage of cerebrospinal fluid due to a ruptured eardrum, hemorrhage in the area of the temporal muscle and behind the ear, partial hearing loss. Bleeding increases when you turn your head, so this is strictly prohibited.
A transverse fracture of the temporal bone is characterized by complete loss of hearing, disturbances in the functioning of the vestibular apparatus, paralysis of the facial nerve, and loss of taste.
- Clinical signs of anterior fossa fracture: nosebleeds, nasal liquorrhea (cerebrospinal fluid discharge through the nose), hemorrhages around the orbits and under the conjunctiva. Bruises appear 2-3 days after the injury, which fundamentally distinguishes them from ordinary bruises that appear as a result of direct blows to the face. Sometimes so-called subcutaneous emphysema occurs: when the cells of the ethmoid bone are damaged, air penetrates into the subcutaneous tissue, causing blisters to form on the skin.
- Clinical signs of a middle cranial fossa fracture: unilateral ear bleeding; a sharp decrease in hearing or complete deafness; release of cerebrospinal fluid due to a ruptured eardrum, dysfunction of the facial nerve, bruising in the area of the temporal muscle and behind the ear; partial loss of taste. Middle fossa fractures account for 70% of skull base injuries.
- Clinical signs of a fracture of the posterior cranial fossa: simultaneous damage to the auditory, facial and abducens nerves; bruising behind the ears on one or both sides; when the caudal nerves are pinched or ruptured, the tongue, palate, and larynx are paralyzed and the functioning of vital organs is disrupted.
- Fractures of the base of the skull are also characterized by damage to the olfactory or optic nerve. With such fractures, the meninges are ruptured, as a result of which a communication channel is formed between the brain matter and the external environment through the nasal and oral cavities, middle ear or orbit. Splinter fractures are especially dangerous in this regard: bone fragments can injure arteries and veins. Communication with the external environment leaves the brain open to infections and microbes and can lead to the development of encephalitis, meningitis or brain abscess.
Characteristics of different types of skull fractures
There are two types of mechanisms for causing a fracture of the base of the skull: direct and indirect. In a direct fracture, the bone breaks at the site of the impact. If the blow is of great force, the bone (or its fragments) is pressed inward and can damage the lining of the brain.
An indirect fracture occurs due to the impact of other bones when the impact force is transferred from another part of the body (pelvis, legs, spine). For example, when falling, the legs initially receive the blow, then along the spine the force of the blow passes to the base of the skull.
Depending on the nature of the injury, its location and the severity of the injury, three main types are distinguished:
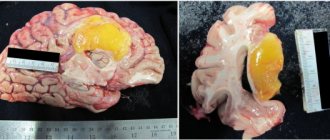
- Comminuted fracture. The most difficult, since bone fragments can damage the meninges and blood vessels;
- depressed fracture. Also dangerous because damaged bones are pressed into the skull, which can lead to brain damage or crushing;
- linear fracture. It looks like a thin line in the photo. With this type of injury, there is no displacement of the bones, but damage to blood vessels and the development of hematomas are possible.
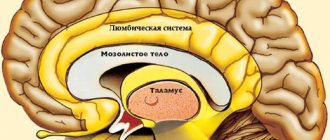
Depending on the location of the injury, fractures of the anterior, middle and posterior cranial fossa are distinguished. The most common of them (up to 50%) occur in the middle part of the cranial fossa. They can be oblique, transverse or longitudinal.
For fractures of the temporal bone pyramid, the most common are longitudinal cracks that appear as a result of a blow to the occipital region. They lead to damage to the middle or inner ear, facial nerve. As a rule, they are accompanied by hearing loss, problems with coordination of movement; possible paralysis of the facial nerve and loss of taste on 2/3 of the tongue.
A fracture of the anterior part of the cranial fossa is often accompanied by bleeding from the nose, as well as bruising around the eyes (lower and upper eyelids), which appear 2-3 days after the injury, and not immediately, as with direct blows. In some cases, the formation of subcutaneous emphysema (swelling) is possible, especially with cracks passing through the air sinuses.
Fractures of the posterior cranial fossa are usually longitudinal and extend from the squamosal fossa to the foramen magnum or jugular foramen. They are characterized by bruising of the mastoid process and damage to the auditory, abducens or facial nerves.
Fracture in the area of the foramen magnum. There is damage to the caudal group of nerves, bulbar symptoms appear, and possible disruption of the functions of the main vital organs.
First aid for a skull fracture
If you suspect a fracture, you should immediately call an ambulance. If the victim’s condition is satisfactory and he is conscious, then he should be placed on his back (without a pillow), his head and upper body immobilized and secured, and an antiseptic bandage applied to the wound. If hospitalization is delayed, dry ice can be applied to the head. If there are no breathing problems, you can give the victim diphenhydramine or analgin.
In an unconscious state, the victim should be laid on his back in a half-turn position and his head should be turned slightly to the side to avoid aspiration in case of vomiting, loosen tight clothes, remove existing glasses, dentures, and jewelry. To secure the body, place a cushion of clothing or a blanket under one side of the body.
In case of acute respiratory distress, artificial respiration is performed through a mask. Cardiovascular drugs (sulfocamphocaine, cordiamine), glucose solution, Lasix are administered. In case of heavy bleeding and a sharp drop in pressure, Lasix is replaced with intravenous administration of polyglucin or gelatinol. During motor excitation, a solution of suprastin is injected intramuscularly.
Painkillers should be used with caution as they may complicate bleeding. The use of narcotic painkillers is contraindicated; they aggravate respiratory disorders.
First aid to the victim
The life of the victim depends on how timely and correctly first aid was provided:
- Before the ambulance arrives, the victim must be placed in a safe position. If the person is conscious, he should be placed on his back,
- If the victim is not available for productive contact , he must be given a stable lateral position so that in case of vomiting, choking or tongue retraction does not occur. It is important that the person lies on a hard surface. Do not place pillows, soft cushions, etc. under your head under any circumstances.
- Next, you need to check the victim’s airway . If necessary, the oral cavity must be cleared of blood clots, mucus, foreign bodies (for example, dentures), etc. Otherwise, aspiration (swallowing) may occur.
- The next step is the application of an aseptic dressing. This must be done very carefully so as not to cause displacement of bone fragments. The safest option is to cover the wound with a clean napkin,
- Before the ambulance arrives, the victim should not be given painkillers. You can gently apply an ice bag wrapped in a towel to your head.
Classification of skull base fractures
Fractures vary:
- According to the damaged bones of the same name;
- Along the cranial fossae of the inner surface of the skull: anterior, middle and posterior;
- In relation to the external environment;
- By the presence or absence of bone displacement.
The occipital and sphenoid bones are part of the brain section of the skull. The temporal bones form the cranial vault and house the hearing organs: the pyramid of the temporal bone contains the tympanic cavity and the inner ear. The anterior fossa is formed by the frontal bone, the plate of the ethmoid bone, and is separated from the middle fossa by the edges of the sphenoid bone. The middle fossa is formed by the sphenoid and temporal bones. The posterior fossa is formed by the occipital bone, the posterior part of the sphenoid bone.
Non-displaced fractures are classified as open TBIs and have a favorable prognosis. If the fracture is accompanied by blood loss or leakage of cerebrospinal fluid, it is considered an open penetrating type TBI.
Treatment of a skull fracture
For an accurate and detailed diagnosis of injury, magnetic resonance imaging (MRI) or computed tomography (CT) is used. Depending on the severity and complexity of the damage, treatment can be conservative or surgical.
Conservative treatment
Conservative methods are indicated for mild to moderate injuries, when liquorrhea can be eliminated non-surgically.
It is necessary to observe strict bed rest, the head should be in an elevated position - this helps to reduce the secretion of cerebrospinal fluid. Treatment includes dehydration therapy (aimed at reducing fluid content in the organs), for this purpose, lumbar punctures (taking cerebrospinal fluid from the spinal cord at the lumbar level) are performed every 2-3 days, and subarachnoid insufflations (introduction into the subarachnoid space of the spinal cord) are carried out in parallel. the same amount of oxygen. Drugs that reduce the production of cerebrospinal fluid are also used - diuretics Diacarb, Lasix.
Physical activity is limited for six months. The victim must be registered with a traumatologist and neurologist, and be observed by an otolaryngologist and an ophthalmologist.
Particular attention should be paid to the prevention of intracranial complications of a purulent nature. For this purpose, sanitation of the nasopharynx, oral cavity and middle ear is carried out using antibiotics. In the presence of purulent complications, intramuscular or intravenous injections are supplemented by the introduction of antibiotics into the epidural space (endolumbar). For this, kanamycin, chloramphenicol, monomycin, and polymyxin are used. Also, endolumbar administration of kanamycin is carried out 2 days after the cessation of liquorrhea. The best way to select a drug is by culture of the cerebrospinal fluid flora or a smear taken from the nasal mucosa.
Surgery
Surgery is necessary in the following cases:
- Detection of a comminuted fracture;
- Damage or compression of brain structures;
- Leakage of cerebrospinal fluid through the nose, which cannot be stopped by conservative methods;
- Recurrences of purulent complications.
Surgical treatment is used in the presence of bleeding, hematoma or bone fragments that may pose a direct threat to life. In this case, trephination (opening) of the skull is performed, and after the operation, the bone tissue defect is closed with the removed bone or a special plate (in most cases). This is followed by long-term rehabilitation.
On topic: 12 folk methods for home treatment
Fractures of the skull bones
In the acute stage, treatment is usually conservative. It consists of repeated lumbar punctures (or lumbar drainage), dehydration therapy, and prophylactic use of antibiotics. In a significant number of cases, it is possible to cope with liquorrhea in this way.
However, in some patients, the leakage of cerebrospinal fluid continues weeks and months after the injury and can cause repeated meningitis. In these cases, there are indications for surgical removal of liquor fistulas. Before surgery, it is necessary to accurately determine the location of the fistula. This can be done by radioisotope research with the introduction of radioactive drugs into the cerebrospinal fluid or using computed tomography and magnetic resonance imaging, especially if these studies are combined with the introduction of special contrast agents into the cerebrospinal fluid.
For nasal liquorrhea, trepanation of the frontal region is usually used. The approach to the location of the cerebrospinal fluid fistula can be carried out both extra- and intradurally. It is necessary to carefully close the dural defect by suturing or repair using aponeurosis or fascia.
The bone defect is usually closed with a piece of muscle.
If the source of the CSF rhea is an injury to the wall of the sphenoid sinus, a transnasal approach with sinus muscle tamponade and a hemostatic sponge is usually used.
With cracks in the bones of the base of the skull passing through the air cavities, in addition to the leakage of cerebrospinal fluid, air may enter the cranial cavity. This phenomenon is called pneumocephalus. The reason is the emergence of a kind of valve mechanism: with each inhalation, a certain amount of air enters the cranial cavity from the paranasal sinuses, but it cannot come back out, because when exhaling, the sheets of torn mucous membrane or dura mater stick together. As a result, a huge amount of air can accumulate in the skull above the cerebral hemispheres, causing symptoms of increased intracranial pressure and brain dislocation with rapid deterioration of the patient’s condition. Air accumulated in the skull can be removed using a puncture through a burr hole. In rare cases, it becomes necessary to surgically close the fistula in the same way as is done for liquorrhea.
With fractures of the base of the skull passing through the optic nerve canal, blindness may occur due to contusion or compression of the nerve by a hematoma. In these cases, intracranial intervention with opening of the canal and decompression of the optic nerve is justified.
Cranioplasty. The consequences of traumatic brain injury can be a variety of, often extensive, defects of the skull. They arise as a result of comminuted fractures; if it is impossible to save a bone flap due to high intracranial pressure and prolapse of the brain into the surgical wound. Bone defects can be caused by osteomyelitis if the wound becomes infected.
Patients with large bone defects react to changes in atmospheric pressure. The development of a scar-adhesive process along the edges of the bone defect can cause pain syndromes. In addition, there is always a danger of damage to areas of the brain not protected by bone. Cosmetic factors are also important, especially for frontobasal defects.
These reasons justify the indications for cranioplasty.
Defects in the convexital parts of the skull can be closed with the help of prostheses made of fast-hardening plastic - styracryl, galacost. While this polymer is in a semi-liquid state, a plate corresponding to the skull defect is formed from it. To avoid the accumulation of blood and exudate between the dura mater and the plastic plate, several holes are made in the latter. The graft is firmly fixed with sutures to the edges of the defect. Tantalum plates and mesh are also used to close bone defects.
Recently, the bone of the patient himself has been used for cranioplasty. For this purpose, a symmetrical area of the skull is exposed and a bone fragment corresponding in size to the bone defect is cut out. Using special oscillating saws, the bone flap is separated into two plates. One of them is placed in place, the other is used to close the bone defect.
A good cosmetic effect can be obtained by using specially processed cadaveric bone for cranioplasty, however, recently the use of this method has been refrained due to the risk of infection with the virus of slow infections.
The most difficult cranioplasty is for parabasal injuries, including the frontal sinuses and orbital walls. In these cases, a complex operation to reconstruct the skull is necessary. Before surgery, the extent and configuration of bone lesions should be carefully studied. Volumetric reconstruction of the skull and soft tissues of the head using computed tomography and magnetic resonance imaging can be of great help. To restore the normal configuration of the skull in these cases, the own bones of the skull and plastic materials are used.