Today, there are more than 50 million people with epilepsy in the world. This disease is caused by non-infectious brain damage and is chronic. It causes seizures of varying levels of complexity, in which a certain clinical picture is observed: convulsions, fainting, salivation, etc. A single case of such symptoms is not a reason to visit a specialist; every person has experienced a similar condition at least once in their life. If the seizures are constant and prolonged, this becomes a good reason to visit a doctor. In order to find out about the presence of a disease and the extent of brain damage, it is necessary to undergo a lot of diagnostic measures that make it possible to establish the type of disease, as well as its effect on the body. One such method is MRI of epilepsy.
What does an MRI of the brain show in epilepsy?
Magnetic resonance therapy for epilepsy shows the affected areas of the brain and is performed in almost all cases of the disease. This is an excellent way to determine the extent to which the disease has spread to healthy cells and the speed of its development. In terms of its information content and harmlessness, MRI is in many ways superior to even computed tomography. In addition, this technique has an obvious advantage: it does not contain X-ray radiation, and it does not affect the human body in any way. MRI of the brain for epilepsy is performed at any age, since this procedure does not provide for severe clinical consequences, it can be used by patients with a disease of any complexity and degree of development.
It is the deep conviction of international antiepileptic organizations that the process of undergoing MRI or CT scanning is mandatory and should be carried out at the request of a doctor.
Many modern clinics with the latest equipment provide the opportunity to diagnose this disease, so the procedure is mandatory. For a successful examination you need:
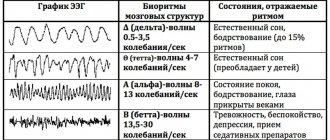
- Referral for research with a competent formulation of a possible diagnosis and the need for diagnostics. The referral must indicate possible suspicions of pathology and any of its manifestations. Based on previous examinations, including EEG, the neurologist can assume the possible location and nature of the pathological process.
- Modern MRI scanner with optimal power and amplitude. Such devices conduct research even with minimal sections.
- Radiation therapy specialist with in-depth knowledge of neurology, with a good understanding of the specifics of the nervous system. The doctor must know when to use additional data collection methods that are not provided for in the medical protocol.
Whether an MRI shows epilepsy depends largely on physicians and consultants, as well as MR imaging specialists, who are often unable to meaningfully analyze the collected data to establish a treatment modality and confirm a final diagnosis. However, according to statistics from the Ministry of Health, the number of cryptogenic epilepsies is significantly decreasing, which has a positive effect on further treatment.
Thus, for successful MRI diagnosis of epilepsy it is necessary:
- a prompt referral for an MRI examination, drawn up by an epileptologist. In most cases, based on the clinical picture and EEG results, a neurologist-epileptologist can make an assumption about the nature and localization of the pathological process and should reflect this in the direction.
- A modern MRI scanner with sufficient magnetic induction power - at least 1.5 Tesla and the ability to conduct research with a minimum slice thickness of 1-2 ml.
- A qualified MRI physician who is well aware of the specific functioning of the nervous system and uses, if necessary, additional data collection methods that go beyond the usual protocol.
Global trends in the development of epileptology indicate a constant decrease in the number of cryptogenic (with an unknown cause) epilepsies and an increase in the number of symptomatic ones, that is, developing secondary to the background of structural and morphological changes in the brain.
Is it possible to detect epilepsy using MRI?
Epilepsy as a disease has been known for more than 7 thousand years, but instrumental diagnostics began only in 1929. Magnetic resonance imaging in this case is a reliable instrumental method for diagnosing such a pathology, therefore complex procedures are practiced all over the world to determine the spread and development of the disease down to the last small detail. It makes it possible not only to identify the disease, but also to identify the causes that provoked it. A significant advantage of the method is high sensitivity, specificity, and absence of radiation. The Association of Radiologists has developed special protocols for identifying the disease. Thanks to this, it is possible to establish the causes of the pathology, of which there are many:
- defects and anomalies of the brain of various types;
- sclerotic changes;
- oncology and benign tumors;
- changes as a result of impacts and trauma experienced;
- infectious lesions;
- vascular pathologies;
- degenerative changes;
- metabolic disorders.
In other words, diagnostics using modern equipment allows us to examine the pathology from the inside and determine the sources and factors that provoked its development. This method undoubtedly influences the level of treatment, since the final conclusions regarding the patient’s diagnosis are based on MRI or CT readings.
Ultra-precise MR examination for epilepsy using the MIBS-II protocol
Back to news list
25 Nov. 2021 11/25/2020
MIBS introduces a new study into clinical practice - high-resolution MR scanning of the brain using the MIBS-II epiprotocol. It will allow the epileptologist to detect foci of epilepsy in the patient that were previously invisible with other types of instrumental imaging.
“By reducing the slice thickness by almost 2 times, we obtained images of higher quality and more information content. This increases the opportunity to find “hidden” zones of structural changes in the cerebral cortex responsible for the development of seizures. This is reaching a new level in the diagnosis of epilepsy, corresponding to the most advanced European standards,” says MIBS radiologist Daria Rudenko .
In accordance with the recommendations of the ILAE (International League Against Epilepsy, International League Against Epilepsy), magnetic resonance imaging of the brain is a mandatory component of the examination of all patients with epilepsy, with the exception of some of its forms. However, routine MRI can only exclude fairly large pathologies - vascular malformations, tumors, consequences of traumatic brain injuries and infectious and inflammatory processes. To visualize smaller structural changes, specialized epileptological MRI protocols are used - with minimal slice thickness, using additional signal amplification and image processing modes.
From the previous epiprotocol, MIBS-I, which also remains in service at the diagnostic center, the new version of MR scanning, performed on a modern three-tesla magnetic resonance imaging scanner MAGNETOM Skyra, differs in thinner sections. The slice thickness is only 0.6 mm compared to 1 mm in MIBS-1 and 5 mm in standard magnetic resonance imaging.
As Daria Rudenko explains, in approximately 15% of cases, the doctor encounters MR-negative cases of epilepsy, when a clinical specialist assumes the presence of structural focal epilepsy, but cannot detect lesions on magnetic tomography images. A more sensitive study using the MIBS-II protocol will make it possible to detect such pathologies. “It can be assumed that MIBS-II will also be useful in multifocal (multifocal) pathologies, in cases where previously used protocols detected only one focus,” adds Daria Rudenko.
In addition, the new technology has another significant advantage that may be important for neurosurgeons. Imaging is done in 3D, the images are 1mm cubic voxels, and the results can be loaded into surgical navigation systems for surgery. That is, simultaneously with an accurate diagnosis, the patient undergoes preoperative preparation. Therefore, this protocol will be important in the treatment of patients with drug-resistant epilepsy (not sensitive to drug therapy) who are candidates for surgery. Drug-resistant epilepsy is quite common, accounting for about 30% of cases of this disease.
MRI scanning of the brain according to the MIBS-II epiprotocol is performed under anesthesia not only for children, but also for adults, since the high sensitivity of the method requires complete immobility of the patient for quite a long time - the study takes 1 hour 45 minutes. You can undergo the study at the Center for Comprehensive Diagnostics of MIBS, located at the address: St. Petersburg, st. 6th Sovetskaya, 24-26.
Back to news list
Who prescribes MRI for epilepsy?
Any disease requires the attention of a specialist, and epilepsy is no exception. Especially considering the fact that the most important human organ is affected. After a detailed history, the therapist refers the patient to an appointment with a neurologist, who records the client for an EEG if his suspicions suggest the possibility of damage to tissue cells. This conclusion is required by the radiologist in order to:
- clarify the areas where epileptic activity was detected;
- if necessary, introduce a number of additional programs during the procedure;
- compare the indicators obtained from EEG and MRI, and determine structural changes in tissues.
The use of tomography has several goals pursued by a neurologist. To clarify suspicions and collected data, only those whose history has identified and described a seizure are sent for MRI, since the program allows for a detailed study of possible structural disorders of the areas that are most active during attacks. In addition, the procedure is recommended for patients with an already confirmed diagnosis who cannot get rid of attacks with the help of medications. Drug-resistant epilepsy is not one of the most common pathologies, but its development has certain risks, since drug treatment does not produce results, and the person may not meet the requirements for surgical interventions. MRI is important to clarify the need for surgical intervention for a specific diagnosis.
What will an MRI show for epilepsy?
“... Then suddenly something seemed to open up before him: an extraordinary inner light illuminated his soul. This moment lasted perhaps half a second; but he, however, clearly and consciously remembered the beginning, the very first sound of his terrible scream, which burst out of his chest of its own accord and which he could not have stopped by any force. Then his consciousness faded away instantly, and complete darkness set in...” - F.M. Dostoevsky.
Today we will talk about a disease that, according to a number of doctors, Prince Myshkin from Dostoevsky’s novel “The Idiot” suffered from. How is it identified today? What contribution does magnetic resonance imaging make to the diagnostic process? Radiologist Zarema Bardudinovna Tseeva told us about this and much more.
- Zarema Bardudinovna, let’s first explain to our readers what kind of disease this is - epilepsy?
This is a chronic disease of the brain, the leading manifestation of which is spontaneous epileptic seizures. It occurs in approximately 1% of people.
- At what age does epilepsy appear?
In any. More often, the disease is congenital in nature, due to which attacks occur already in childhood (5-10 years), as well as in adolescence (12-18 years). However, epilepsy can also be acquired, that is, it can arise as a result of a number of brain pathologies.
- How common is the diagnosis of “epilepsy” in our country?
In Russia there is no exact data on this disease, but according to statistics, the incidence is relatively high and, importantly, tends to increase. Thus, over the past 5 years the number of patients has increased by almost 40%. The average incidence in the country is 95 cases per 100,000 population.
- What are the causes of epilepsy and who is at risk?
These are various types of pathological changes in the brain: congenital developmental anomalies, genetic changes, damage in the pre- and perinatal period, traumatic brain injuries, circulatory pathology, consequences of infectious diseases (meningitis, encephalitis), neoplasms.
Factors that provoke the development of an epilepsy attack may be psycho-emotional stress, stress, climate change, overwork, insufficient or excessive sleep, and bright light.
The risk group for children includes those who have suffered hypoxia during childbirth, infectious diseases involving nervous tissue, repeated cases of seizures at high body temperature, and brain injuries. Hereditary burden on the part of either parent matters.
- How does epilepsy manifest and is it treated?
The leading manifestation in both adults and children is spontaneous epileptic seizures. Preceding symptoms are a possible “aura”: dizziness, auditory or visual hallucinations. Loss of consciousness, convulsions, and “foam” from the mouth are noted.
Epilepsy is certainly treatable. In 70% of cases, treatment is medicinal, in 15% surgical interventions are used. The remaining cases are more difficult to treat, however, their relief is also possible.
With this disease, in some cases, stable remission is possible; in others, anti-relapse treatment is carried out.
- No one will argue with the fact that any treatment begins with diagnosis. How is epilepsy diagnosed?
It is carried out on the basis of an eyewitness account of the attack, the results of a full examination, assessment of the neurological status, data from electroencephalography and magnetic resonance imaging. If MRI is not possible, computed tomography can be performed, but its diagnostic capabilities in terms of epilepsy are significantly inferior to MRI.
- Zarema Bardudinovna, what role does MRI play in diagnosing epilepsy?
The most direct one. Magnetic resonance imaging is one of the most informative neuroimaging methods. It allows you to identify the causes that cause the development of epileptic seizures, and can also help in determining the localization of the pathological focus when the issue of surgical treatment is being decided.
- What is MRI in the Epilepsy program? How does this diagnosis differ from conventional magnetic resonance imaging of the brain?
This study, which is a high-resolution MRI, is usually performed after a traditional procedure to clarify points characteristic of epilepsy and not clearly identified during standard tomography. It is also performed in case of resistance to anticonvulsant therapy and for its correction, before surgery for epilepsy. The data obtained using this type of study is compared with the EEG to obtain a more complete and accurate picture of the pathological process.
- What is an MRI of the brain according to the epileptological scanning program?
This is the same as the MRI in the Epilepsy program.
- How is magnetic resonance imaging performed in patients with epilepsy and does it require preparation?
The patient is questioned in detail, including to clarify the issue of contraindications. The procedure itself is generally identical to a standard MRI examination. No special preparation is required.
- What determines the prognosis of the disease? Is this diagnosis always a death sentence?
For prediction, the cause of the disease and the possibility of eliminating it, as well as age, are important. Epilepsy is not a death sentence. There are cases of permanent relief from attacks. In any case, the patient’s condition can be corrected with medication or surgery.
-Which specialist should see a patient with epilepsy?
There are several doctors who treat epilepsy. First and foremost, he is a neurologist, as well as a specialist – a neurologist-epileptologist. If there is a need for surgery - a neurosurgeon. If mental disorders occur, use a psychiatrist.
For reference:
Tseeva Zarema Bardudinovna
Graduate of Kuban State Medical University in 2008, Faculty of General Medicine.
In 2009 she completed her internship in the specialty “Therapy”, and in 2010 - in the specialty “Radiology”.
From 2010 to the present, he has been working as a radiologist at MRT Expert Sochi LLC.
CT or MRI - which is better?
Quite a lot depends on the choice of equipment, so random visits to such diagnostic centers are unacceptable. For more detailed diagnostics, the MRI unit is equipped with programs that were created to obtain additional information about the condition of the affected tissues. The absolute coverage of such tissues by the information field of the tomograph greatly simplifies the process of determining therapy and the level of risks for individual cases.
MRI according to the “Epilepsy 3 Tesla” program allows you to create optimal conditions for a patient who can succumb to an epileptic seizure at any moment, and collect the necessary information on the specifics and development of the disease in great detail. The use of modernized equipment in medical institutions has led to first-class diagnostic quality, but thereby increased its duration. However, this method is most in demand in cases where it is difficult to give a final conclusion or determine the damaged areas due to the presence of a tumor or vascular compactions. And whether epilepsy is visible on an MRI of the brain is a rhetorical question.
A CT scan is performed to obtain a detailed cross-sectional picture of the brain. Specialized equipment ensures the safety of the procedure and efficiency, and also guarantees the quality of the results obtained. This is a painless examination option, the only contraindication for which is pregnancy. Both tomography options have their advantages, but the need to use one or another device is determined by the attending physician.
Based on the characteristics, it should be noted that these options are suitable for many patients and do not carry great risks. Precautions and contraindications are always determined before the start of treatment and require general tests and a complete medical history. A detailed study of the pathology allows us to exclude possible complications and additional difficulties during therapy. The patient must provide complete information about the disease, personal intolerance to drugs and allergies, and indicate complications of illness or surgery.
MRI for episyndrome
Hardware scanning with great accuracy determines such an anomaly as hippocampal sclerosis, which is the root cause of chronic epileptic seizures. Also, when examining using an enhancing contrast agent, areas of formation of benign tumors are clearly visible. They are also the cause of the anomaly.
MRI of the brain for epilepsy is most effective for recognizing intrauterine disorders in the brain area, starting from the second trimester of pregnancy. For adult patients, when symptoms appear, diagnosis is prescribed in the post-traumatic period, since scars in the tissues of the organ often lead to the appearance of a secondary syndrome.
An alternative to nuclear resonance screening can be computed tomography, as it perfectly visualizes soft tissues. However, unlike MRI diagnostics, during computer scanning the human body is subjected to additional stress from X-ray radiation.
High-resolution MRI for episyndrome is performed using high-power machines. Thanks to the increased power, the duration of the procedure is significantly reduced, and the clarity of the resulting images increases significantly. Additional contrast enhancement is also not required, since the resolution provides maximum contrast images that can not only be zoomed in, but also composed into a three-dimensional image. This allows you to study the problem from different angles and in any projection.
MRI for episyndrome recognizes the following causes of the pathological process:
- post-stroke necrosis of gray matter cells as a result of cessation of their blood supply;
- the appearance of obstacles in the vascular channels that interfere with normal blood flow (cholesterol plaques and calcium deposits);
- cystic formations and tumors of benign etiology, which, as they grow, displace and compress adjacent tissues and vessels, this interferes with the normal nutrition of nerve fibers, which leads to the appearance of a secondary syndrome;
- cancerous formations growing into neighboring structures, migration of metastases;
- aneurysms of large vascular canals, in which stretching and swelling of the walls of blood vessels occurs, pressing on nearby nerve endings;
- multiple sclerosis, detected in any zone of the gray matter.
How is an MRI performed for epilepsy?
The main obstacle for many is the fact that during the tomography the patient must remain motionless for up to 50 minutes, which is extremely difficult for people with increased irritability or constant anxiety. The procedure itself is carried out according to the same standards as for any other disease that requires a similar diagnosis. Epilepsy is chronic, and it is quite difficult to predict the onset of the next attack. The main object of the search is focal cortical dysplasia, which is a specific sign of true epilepsy, and not symptomatic.
After anamnesis and mandatory tests with established results, the doctor sends you for diagnostics. The patient takes off all metal jewelry, belts, costume jewelry, precious metals and other paraphernalia and sits on the tomograph couch. After this, it enters the center of the ring magnet, and the diagnostic process itself starts. This manipulation does not cause any sensations or discomfort; any complications or inconveniences can arise exclusively in the technical part of the equipment.
The specialist performing the procedure is in another room behind glass and communicates with the patient via a microphone. There should be no foreign objects in the inspection area that could disrupt the operation of the unit. The patient should listen carefully to the doctor and follow his instructions, while remaining as still as possible. A long, but non-traumatic process extracts all the necessary information about the state of the cells and the extent of the spread of the disease.
How is a high-resolution MRI of the brain performed?
High-resolution MRI of the brain is performed in the same way as all diagnostic studies using magnetic resonance imaging.
The patient lies down on the table and listens to the doctor's instructions. He is informed that he needs to lie still, and at the request of the specialist he will have to hold his breath.
If a study with a contrast agent is to be performed, an intravenous injection of contrast is given.
Next, the table with the patient slides under the tomograph scanner. Sensors collect the necessary information, process it and transmit it to the monitor screen. The doctor may magnify the image to better see the areas of the brain that are of greatest interest to the doctor.
The duration of the diagnosis is approximately 40 minutes. If it is necessary to use a contrast agent, the period increases to 60 minutes.
MRI with contrast for epilepsy
It is known that epilepsy is a disease that has several factors that provoke characteristic seizures. This greatly expands the range of searches for affected tissue areas, which is why different research methods are used. Protocols for diagnosing chronic brain lesions involve the use of a contrast agent, which makes it possible to determine the extent of changes and the functioning of the naked brain during the study.
The procedure itself consists of administering a substance intravenously; it quickly spreads through the vessels and veins, ultimately reaching the brain. The contrast itself contains an acceptable amount of iodine and other compounds that, when released into the blood and under the influence of rays, display their own color. This is how the easily recognizable mesh of the venous system appears. On the computer image, clear contours of all channels and the circulatory system of the head are visible, the smallest changes in the structure of blood vessels are determined, and specialists see where inhibition or fluid accumulation occurs. This is another effective way to determine epilepsy by MRI, caused by vascular pathologies or degenerative changes.
MRI for EPILEPSY
In the diagnosis of epilepsy, electroencephalography (EEG) plays a leading role, and currently the most informative diagnostic method is video EEG monitoring. This method quite accurately detects disturbances in the activity of the cerebral cortex, but does not show the possible causes of the disease.Conventionally, the causes of epilepsy and epileptiform syndromes can be divided into “volumetric” and “non-volumetric”. Bulk causes include tumors, vascular aneurysms, and malformations. In such cases, surgical treatment can eliminate the cause of the seizures. “Non-volume” causes include the consequences of strokes, traumatic brain injuries, and developmental defects. Sometimes the cause of seizures can be a demyelinating process.
And if EEG diagnostics registers epileptic activity of the brain, then the next diagnostic step is to identify or exclude structural pathology of the brain, which can provoke seizures. And here the main diagnostic tool is magnetic resonance imaging (MRI).
MRI is currently the “gold” standard for diagnosing the morphological substrate of epilepsy. When a structural pathology of the brain is identified, the clinician (neurologist or epileptologist) decides on the choice of treatment method (conservative or surgical).
Considering the fact that the main task of MRI in the diagnostic process of epilepsy is to identify structural pathology, the maximum quality of the obtained images is necessary. One of the most important factors on which image quality depends is the magnitude of the magnetic field induction of the MRI scanner, which is measured in Tesla (T). Today, an induction of 3.0 T is the maximum possible for use in clinical practice. This makes it possible to obtain MR scans (slices) of the brain with high spatial resolution (less than 1.0 mm thick), necessary for identifying small epileptogenic lesions. The second advantage of the image obtained on an ultra-high-field MR tomograph is its high contrast resolution, which ensures clear differentiation of intact gray and white matter of the brain and pathological foci.
High-resolution MRI makes it possible to identify structural abnormalities in the anatomical structures of the brain responsible for the formation of pathological epileptic activity. Such changes usually go undetected during standard MRI scans of the brain. An example is changes in the structure of the hippocampus, such as hippocampal sclerosis, which are not detected by conventional MRI.
*Hippocampus (from ancient Greek ἱππόκαμπος - seahorse) is part of the limbic system of the brain (olfactory brain). Participates in the mechanisms of emotion formation, memory consolidation (that is, the transition of short-term memory to long-term memory), generates the theta rhythm when maintaining attention. Plays a key role in the formation of epileptic activity.
However, the magnitude of the magnetic field induction of an MRI scanner is not the only condition for obtaining high-quality diagnostic data. Another such condition is the use of a special research protocol designed to identify the substrate of epilepsy in accordance with international standards. An MRI protocol is a set of specific programs called pulse sequences, each aimed at better visualizing a specific pathology.
According to a recent international study, standard MRI does not detect up to 57% of focal epileptogenic zones, and hippocampal sclerosis remains undetected in 87% of cases.
In addition to standard “anatomical” MRI, MR spectroscopy is now widely used, a method that allows non-invasive assessment of the concentration of major neuronal metabolites in a given area. When examining patients with epilepsy, it provides additional information about the location of the pathological focus and its nature.
Another important condition for a high-quality diagnosis of epilepsy is the interpretation of the results of an MRI study by a radiologist specializing in the study of this pathology. The results of the above international research study showed that high-resolution MRI detects focal changes in 91% of cases ONLY when the data is assessed by a specialized radiologist. For comparison: with standard MRI, the result is achieved only in 39%.
Our clinic has the ability to conduct MRI studies of the brain using a specially developed “Epilepsy” program, taking into account all the nuances of modern radiation diagnostics of this disease. Our specialist radiologists have been dealing with this problem for a long time together with leading epileptologists and neurosurgeons in Moscow and have extensive experience in interpreting the results obtained.
Contraindications
There is no need to take any special measures before the diagnosis itself. The patient can continue medication treatment, adhere to the diet and all the doctor’s requirements. Usually the patient leads a full life, without restrictions and precautions. The main recommendation of doctors is a calm environment at work or at home. An isolated case is a patient who experiences a short interval between seizures. Such people are often kept under the supervision of specialists to establish the intervals between attacks, then acceptable options for examination are prescribed.
Despite all the harmlessness, the procedure still has a number of limitations. This is the presence of any metal implants in the body, implants of the inner and middle ear, as well as pacemakers. In addition, it is not recommended to undergo examination for people whose weight exceeds 130 kg. The first months of pregnancy in women are also contraindications. The procedure is contraindicated for people suffering from claustrophobia. Patients in this category undergo pre-treatment or a similar procedure using adapted devices.
High-precision MRI of the brain to exclude organic causes of epilepsy (episyndrome)
Description of medical service:
The service includes
- specially designed targeted orientation of tomographic slices at the level of the head, body and tail of the hippocampus;
- thin-section scanning of the brain in IR mode to exclude congenital cortical malformations and anomalies that may be an organic cause of epilepsy in children and adults.
The scanning protocol was developed taking into account the recommendations of the world's authoritative radiological communities (European Congress of Radiology - ECR, American College of Radiology - ACR). This is a multi-projection scan with a set of pulse sequences T1, T2, DWI, FLAIR, Hemo.
Brain scanning in episyndrome mode allows with high accuracy:
- identify a complex of organic disorders associated with epilepsy,
- obtain information about the state of the white and gray cerebral matter, the presence or absence of focal changes of various etiology and pathogenesis, cerebrospinal fluid circulation disorders, anomalies in the development of the cerebrum and structures of the posterior cranial fossa, extracerebral and meningeal tumors, hematomas and ischemia,
- give an overview of the condition of the pituitary gland and paranasal sinuses.
Types and costs
| Service | Cost, rub. | Action in the center on Musa Jalil |
| High-precision MRI of the brain to exclude organic causes of epilepsy (episyndrome) | 4500 rub. | 3950 rub. |
The prices indicated on the website are not a public offer (according to Article 435-437 of the Civil Code of the Russian Federation). You can find out the exact cost of studies and additional services from the administrators of our MRI centers by calling the numbers listed on the website or using the feedback form.
Preliminary preparation before the procedure:
not required.
Scan time:
about 40 minutes; when examining with a contrast agent, the scanning time increases to 60 minutes.
Time to prepare a medical report:
from 30 minutes or more (depending on the category of complexity of a particular case) after the scanning procedure.
Indications for the study:
epilepsy of unknown origin in children and adults.
Contraindications to medical services:
It is known that the MRI technique does not involve the use of ionizing radiation, and this is its important advantage. However, it is necessary to strictly observe certain precautions when performing MRI, due to the fact that the method is strictly contraindicated for a certain group of people, namely:
- patients with pacemakers and implanted cardiac defibrillators (non-removable);
- patients with foreign metal fragments in the eye area;
- patients with cochlear implants (non-removable);
- patients with implanted neurostimulators (non-removable);
- patients with aneurysmal ferromagnetic clips (non-removable);
- patients with shrapnel and bullet wounds and the presence of metal fragments in the body;
- patients with portable insulin pumps (non-removable).
The above conditions form a group of absolute contraindications to MRI and require immediate refusal to conduct the study.
We take patient safety very seriously. When registering for a study, call center operators must check the presence of implants or other metal elements. In addition, before the procedure, our employees will provide you with an informed consent questionnaire to identify any contraindications.
MRI for epilepsy in children
Unfortunately, one of the causes of the disease is a congenital pathology of fetal development. Patients of neurologists and epileptologists often include children of all ages. MRI for epilepsy in children is performed in order to exclude the most dangerous causes that require surgical intervention:
- tumor;
- consequences of injury;
- congenital developmental anomalies;
- cortical dysplasia;
- manifestations of genetic diseases.
It is worth remembering that this examination requires standing still (in the case of examining children) for about 20–30 minutes, so this often becomes a problem. Children are afraid of noise, the absence of adults nearby and unfamiliar sensations. In order for the process itself to proceed quickly and efficiently, a qualified specialist is required who can identify the problem and is well acquainted with the changes in epilepsy. To diagnose all possible changes in brain tissue, the examination must be carried out on a high-field (not
Why do a high-resolution MRI of the brain?
The main reason why an examination is prescribed is the need to identify or exclude the presence of pathological changes in the brain.
A magnetic resonance imaging scanner allows you to obtain a three-dimensional image of any part of the brain. The 3D image shows tumors, cortical pathologies, the results of traumatic injuries, and inflammatory processes. High-resolution MRI of the brain is performed not only to identify the causes of epilepsy. The examination also helps diagnose other pathologies, for example, identify the focus of the disease during a stroke, and detect congenital anomalies.
Deciphering MRI for epilepsy
MRI images of the brain are interpreted exclusively by a qualified radiologist. Often this is a specialist who personally performed the diagnosis and works closely with the patient’s attending physician. Correctly interpreting and explaining images requires professional medical training and significant practical experience. At the clinic, the patient can receive tomography results a few hours after completion of the procedure or the next day.
Basic information is transmitted electronically to the attending physician. Specialists conduct a thorough examination of the scanograms, after which they report the results. The images are used to prescribe additional diagnostic measures if the disease causes controversial statements. None of the doctors with a narrow specialization in other areas has the right to interpret the results in any order. Any findings by doctors who are not radiation specialists or the patient's attending physician cannot be considered as a final diagnosis.
Why is specialized MRI performed for epilepsy?
There are two main motives for undergoing a specialized MRI according to the epiprotocol.
First, MRI data of the brain will be the final confirmation of the absence/presence of epilepsy, which will be reflected in future treatment tactics or will become the basis for monitoring the situation over time.
The second motive is the exact localization (determining the location) of the area of the brain “responsible” for the presence of epilepsy. It is this area, usually tiny, that is subject to radical treatment. Today, treatment of epilepsy can be carried out either by traditional neurosurgical intervention or by non-surgical means.
Prices for MRI for epilepsy in Moscow
The results of an MRI examination do not constitute a doctor's opinion. This is one of the diagnostic methods, which is largely educational in nature for the doctor, who uses several similar conclusions to determine the diagnosis and prescribe drug or surgical therapy. Therefore, the images and the information obtained appear in the protocols as the main and legal indications for starting and conducting treatment for the patient. This method of examination by specialists is one of the most popular for many diseases. A narrow range of contraindications allows the use of an objective examination of the whole body under any circumstances and in different patients.
The cost of diagnostics in each clinic is determined differently. This depends on the focus and status of the medical institution in which the person is being examined. In addition, the price is also affected by the specifics of the therapy. A patient who is an inpatient in a hospital receives the service free of charge. The cost varies depending on many factors that are often beyond the control of the organization itself. The emergence of modified equipment with the latest developments often affects the pricing of other units already in operation. But even with such price fluctuations, we can say that this is an affordable survey method. 55% of patients use MRI and CT services. Thus, these methods are recognized as one of the most effective, painless and informative methods in examining pathologies of various types and nature.
Price for MRI for episyndrome
The cost of diagnostics depends on numerous factors, which include: the workload of the clinic, the qualifications of the staff, the modernity and power of the equipment, as well as the presence of additional procedures (for example, the use of contrast).
The center's discount programs also affect the final amount. To find out the price of an MRI for episyndrome, as well as to get more detailed advice, you can call our operators. They will tell you the addresses of clinics, the exact cost of the procedure, help you choose the most convenient time to make an appointment, and much more.
All contacts are on our portal.