Almost everyone has experienced a headache at some point, and most of us have had one many times. A minor headache is nothing more than an unpleasant experience that is relieved by taking regular pain medications, eating, drinking coffee, or resting. Most headaches are not the result of a serious medical condition, but if you have a very severe or unusual headache, you should consult with a specialist to rule out a life-threatening emergency condition (intracerebral hemorrhage, brain tumor, or cerebral vein thrombosis). ). Fortunately, such problems rarely occur. However, you should know how to control the vast majority of headaches that do not threaten your health.
According to WHO, almost half of adults have experienced a headache at least once in the past year. Regular headaches are among the most common disorders of the nervous system, but unfortunately the population is not perceived as a serious disorder, since they are mostly episodic, do not lead to death and are not contagious. Low rates of medical consultation in developed countries may indicate that many people suffering from headaches are unaware that effective treatment exists. It is estimated that 50% of people with headaches self-medicate.
What types of headaches are there?
A headache can affect any part of the head, and the pain may be present in one or more places.
Doctors classify headaches depending on whether the pain is caused by an underlying medical condition. In other words, headache can be primary or secondary.
Primary headaches
Primary head
pain is not a sign of any disease. Chemical activity in the brain, nerves, blood vessels, or muscles of the head and neck (or a combination of these factors) may play a role in causing primary headaches. Some people may also carry genes that make them more likely to develop such headaches.
The most common primary headaches are:
- Tension headache;
- Migraine;
- Beam (cluster) headache.
Some headaches are also considered primary, but are less common. These headaches have certain characteristics, such as: short duration or association with certain activities.
Other primary headaches:
- Primary headache when coughing;
- Headache on exercise;
- Primary headache associated with sexual activity;
- Primary stabbing headache;
- Possible primary stabbing headache;
- Hypnic (alarm clock) headache.
Secondary headaches
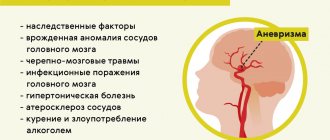
Headache caused by organic pathology is called secondary headache. Clinicians who evaluate patients with headache should be alert for signs suggestive of life-threatening illness. Possible causes of secondary headaches:
- Acute sinusitis (infection of the nose and sinuses);
- Dissection (dissection) of the arteries of the neck and brain;
- Venous thrombosis of the brain;
- Cerebral aneurysm;
- Intracerebral hemorrhage and subarachnoid hemorrhage;
- AVM (arteriovenous malformation) of the brain
- A brain tumor;
- Traumatic brain injury;
- Coronavirus disease 2021 (COVID-19);
- Encephalitis and meningitis;
- Giant cell arteritis (inflammation of the lining of the arteries);
- Glaucoma (angle-closure glaucoma);
- Arterial hypertension;
- Excessive use of painkillers.
How to quickly overcome headaches
- 1. Sleep
. Most often, this method turns out to be the most effective to relieve headaches. 1-2 hours of sleep will allow you to return to normal and stop the torment. - 2. Relaxation
. This means real targeted relaxation with consistent relaxation of all the muscles of the body, and not just sitting with your eyes closed. 15-20 minutes of complete muscle relaxation is usually enough for the pain to subside.
- 3. Push-ups
. A slightly unusual, but very effective method is to do a good push-up on the floor. In this case, your hands need to be positioned so that muscle tension falls on the areas where pain is felt. If the cause of headaches is blood stagnation in the neck or muscle spasm, then push-ups will easily relieve it. Other strength exercises, such as dumbbells, are also fine. - 4. Eye exercises
. 5-10 minutes of doing any eye exercises (usually “drawing” imaginary geometric shapes with your eyes) helps relieve pain if it is concentrated in the frontal part of the head. - 5. Lemon
. To relieve headaches, apply the inside of a lemon peel to your temples and forehead. - 6. Beets
. Fresh circles are also applied to the forehead and temples, but, unlike lemon, beets can leave marks on the skin. - 7. Cabbage leaf
. An old, proven remedy for headaches is to mash a cabbage leaf so that it releases the juice, then apply the leaf to your temples and forehead, and lubricate the inside of your wrists and the area behind the ears with the juice. - 8. Herbal teas
. A cup of hot tea made from chamomile or calendula will help relieve pain caused by minor indigestion. A cup of lemon balm tea will help relieve pain caused by nervous stress.
- 9. Milk with honey
. If the headaches are caused by a mild exacerbation of chronic gastritis, then a glass of hot milk with a dissolved teaspoon of honey will almost certainly help. - 10. Vinegar compress
. 1 teaspoon of table vinegar per 0.5 liter of cool water, soak a towel in the resulting solution and apply to the forehead and temples. - 11. Cinnamon
. Add 1 gram of cinnamon to 100 ml of hot water (not boiling water), cover, let it brew for 30 minutes, then strain and slowly drink in small sips. The remedy will help faster if you drink it on an empty stomach. - 12. Strong coffee
. This method can help if the pain is due to a situational decrease in blood pressure. Coffee should only be natural, because instant coffee does not have the desired effect. - 13. Water
. If the pain arises from dehydration, then you just need to restore the water balance in the body. To do this, drink a liter of water in small sips over 1 hour. You cannot immediately drink large volumes of liquid - in this case, 70-80% of the water will be excreted in the urine, and the therapeutic effect will not be achieved. - 14. Self-massage
. Depending on the location of the pain, you need to rub your temples in a circular motion or rub the back of your head or forehead with your palm until a feeling of intense warmth appears in the massage area. - 15. Towel
. Another old but working trick is to tightly bandage your head with a towel and wear it for about 1-3 hours.
And one more little tip
: supporters of alternative medicine claim that even the most persistent headaches go away if you lean your forehead against an aspen tree, which supposedly has the property of absorbing negative energy. It is not known whether this will help, but if there is nothing else at hand, then you can try - it definitely won’t make it worse.
Tension headache
Tension headaches affect approximately three out of four adults and are the most common of all headaches. The lifetime incidence in the general population, according to various studies, can range from 30% to 78%.
Tension headache
divided into
episodic
and
chronic
.
Tension headache symptoms . Attacks of episodic tension-type headaches (ETH) are usually bilateral, pressing or squeezing in quality, of mild to moderate intensity, lasting from a few minutes to several days. The pain is not worsened by normal physical activity and is not associated with nausea, although photophobia or phonophobia may be present.
Episodic headaches can transform into chronic headaches.
Chronic tension-type headache (CTTH) develops from frequent, episodic tension-type headaches, with daily or very frequent episodes of headache, usually bilateral, pressing or tightening in quality, mild to moderate intensity, lasting several hours to several days or continuous. The pain is not worsened by normal physical activity, but may be associated with mild nausea, photophobia, or phonophobia.
Treatment of headaches is aimed at improving the patient’s emotional state, eliminating muscle tension, and correcting psycho-emotional disorders. Main approaches include behavioral therapy, management of painful episodes, and preventative treatment.
The main provisions of behavioral therapy include: an explanation of the benign nature of tension headaches, the mechanisms of its occurrence (the role of emotional and muscle tension), the need for training in psychological and muscular relaxation, as well as the mechanisms of action of preventive drugs (antidepressants) and the benefits of non-drug methods.
For cupping
During painful episodes, simple analgesics/non-steroidal anti-inflammatory drugs (NSAIDs) are recommended.
Ibuprofen 400 mg is recommended as the first choice drug, which has the least potential to cause gastrointestinal complications. Preventive treatment
is recommended for patients with CHF and frequent EGTH and includes exclusively antidepressants. The effect of antidepressants in primary headaches is due to their own analgesic effect due to increased activity of antinociceptive (anti-pain) systems. Treatment is considered effective if the frequency of episodes of headache (the number of days with headache per month) is reduced after 3 months of therapy by 50% or more from the initial value. Treatment with the most effective antidepressant, amitriptyline. Mirtazapine and venlafaxine are recommended as second choice drugs, and other tri- and tetracyclic antidepressants are recommended as third choice.
What does a doctor do at home for a headache?
A doctor who arrives on call will listen to the patient’s complaints, conduct a visual examination, get acquainted with the medical history, and the results of previous tests if the person has a chronic disease. He also:
- carries out the necessary diagnostics: measures blood pressure, heartbeat, temperature;
- tests the ability to navigate in space;
- can conduct an EGC, collect the necessary materials for further transportation to the laboratory for analysis;
- performs a blockade - a medical procedure to relieve pain.
The doctor may also recommend further examination and treatment, prescribe medications, diet, and therapeutic massage. He can also name the causes of pain and methods for preventing attacks of pain.
If necessary, the doctor may recommend visiting other specialists.
Migraine
Migraine
- This is a common disease that leads to disability due to headaches. Many epidemiological studies have documented its high prevalence and socioeconomic and personal consequences. The incidence of migraine worldwide is 10-13.8%, and in Russia it is about 20.8%. The Global Burden of Disease Study 2010 (GBD2010) ranked migraine as the third most common disease in the world. It ranks third as the world's highest cause of disability in both men and women under 50 years of age.
Migraines are less common than tension headaches, but they are usually much more severe. They are two to three times more common in women than in men. A Harvard study of 20,084 men aged 40 to 84 found that having migraines increased the risk of heart attacks by 42% for men with migraines. Genetic predisposition may also play a role, as a family history of migraine is a common risk factor.
Migraine triggers.
Although migraines can occur without warning, they are often caused by triggers.
Main migraine triggers:
Some other possible triggers include: fatigue, sleep disturbances, physical stress, jet lag due to long-haul flights, and irregular meal times. |
Migraine symptoms.
Migraines often begin in the evening or during sleep. For some people, attacks are preceded by fatigue, depression and lethargy for several hours, or irritability and restlessness. Because migraine symptoms vary widely, at least half of all migraine sufferers think they have sinus headaches or tension headaches rather than migraines.
Most migraine attacks occur without an aura. Headache, manifested by attacks lasting 4-72 hours, unilateral localization, pulsating, moderate or severe intensity, aggravated by normal physical activity and accompanied by nausea and/or vomiting; photophobia and/or phonophobia.
About 20% of migraines begin with one or more neurological symptoms called aura. An aura is a complex of neurological symptoms that usually occurs before a headache, but may begin after the headache phase begins or continue into the headache phase.
Visual aura is the most common type of aura, occurring in more than 90% of migraine patients with aura in at least some attacks. It often presents as a spectrum of consolidation: a zigzag figure near the point of fixation that may gradually widen to the right or left and assume a laterally convex shape with a curved shimmering edge, leaving behind an absolute or variable degree of relative scotoma. The next most common sensory disturbances are pins and needles that move slowly from the site of origin and affect more or less of one side of the body, face and/or tongue. Numbness may follow, but numbness may also be the only symptom. Speech disorders are less common.
Answer the following 3 questions
Over the past 3 months, have your headaches been accompanied by the following symptoms:
| 1. Nausea or vomiting | Yes | No |
| 2. Intolerance to light and sounds | Yes | No |
| 3. Did your headache limit your ability to work, study, or do your daily activities for at least one day? | Yes | No |
If you answered “yes” to at least two questions, then there is a 93% chance that you have migraines.
Migraine treatment
Traditional migraine therapy consists of behavioral therapy, relief of an already developed attack and preventive treatment aimed at preventing attacks. Behavioral therapy, a necessary stage in effective patient management, is carried out during a conversation with the patient and includes: explaining the benign nature of migraine, dissuading the presence of an organic disease, discussing the role of attack triggers and the need to avoid them, risk factors for chronic migraine (taking a large number of painkillers, stress , psycho-emotional states), as well as justification of treatment tactics (mechanisms of action of prescribed medications).
Treatment for a migraine attack is prescribed depending on its intensity and the degree of maladjustment of the patient. For infrequent attacks of mild or moderate intensity, simple or combined analgesics are indicated; for severe nausea and vomiting - antiemetics. When pain is intense and there is significant maladjustment, triptans are prescribed.
Currently, new groups of drugs for the relief of migraine attacks have been approved around the world. This, in turn, allows doctors to treat their patients more effectively, and patients to reduce the number of days with headaches, improve quality of life, sleep, mood and performance.
Lasmiditan
is a selective serotonin 1F receptor agonist that does not have vasoconstrictor activity. The role of lasmiditan in clinical practice has not yet been determined, but it is probably best suited for patients with relative contraindications to triptans due to cardiovascular risk factors.
In October 2021, the US Food and Drug Administration (FDA) approved lasmiditan oral tablets for the treatment of acute migraine in adults. The drug is currently not registered in the Russian Federation.
CGRP antagonists
( Rimegepant and Ubrogepant)
Monoclonal antibodies directed against the CGRP receptor or ligand. They are oral options available for the acute treatment of migraine in patients with inadequate response or contraindications (eg, coronary artery disease) to triptan treatment.
Ubrogepant
received US Food and Drug Administration (FDA) approval for the treatment of acute migraine in adults in December 2021, and rimegepant received similar FDA approval in February 2021. This group of drugs is not registered in the Russian Federation.
Preventive therapy
is aimed at reducing the frequency, duration, intensity of attacks, the number of doses of painkillers and improving the quality of life of patients.
The main indications for a course of treatment: frequency of headache days > 4 per month, insufficient effectiveness of drugs for relieving migraine attacks, presence of risk factors for chronic migraine (abuse, depression), prolonged aura (>60 min). The duration of the course of treatment is from 3 to 12 months (on average 4-6 months for episodic, 8-12 months for chronic migraine), then an attempt is made to gradually withdraw the drug(s) or reduce their dosage.
CGRP antagonists
is a human monoclonal antibody that binds to and inhibits the calcitonin gene-related CGRP receptor (CGRP), and is a therapeutic target in migraine due to its putative role in mediating trigeminovascular pain transmission and the vasodilatory component of neurogenic inflammation
Large molecules in the form of monoclonal antibodies directed against the CGRP receptor or ligand are given by injection to prevent migraines. The US Food and Drug Administration (FDA) approved the CGRP antagonist monoclonal antibodies erenumab, fremanezumab, and galcanezumab in 2021 and eptinezumab in 2021 for the preventive treatment of migraine. In 2021, two drugs were registered in the Russian Federation (erenumab, fremanezumab).
Chronic migraine
In patients suffering from migraine attacks against the background of daily or almost daily headaches, it was emphasized that there is a period of change (transformation) in the nature of the headache - from episodic attacks of migraine headaches to the gradual development of daily or almost daily headaches. The period of headache transformation is not identified in the anamnesis in all patients.
According to statistics, the incidence of chronic migraine in the world is 1.4-2.2%, in the Russian Federation - about 6.8%.
The criteria for chronic migraine are:
- Headaches more than 15 days a month over the past 3 months;
- ≥ 8 days per month for > 3 months headache meets criteria for migraine headache;
- With or without analgesic abuse.
Treatment of chronic migraine
Due to the severe course of the disease and multiple comorbid disorders, optimal management of patients with CM should be carried out. Drugs are selected taking into account the comorbid background; The duration of treatment should be at least 1 year. Topiramate and botulinum therapy with botulinum toxin type A (BTA) have proven effectiveness in treating CM. Botulinum therapy - both in the world and in Russia, is used for the preventive treatment of CM - can be used if previously conducted courses of preventive treatment are ineffective, or used as a first-line drug in the presence of contraindications to taking tablets, or in combination with them. For BTA, specific treatment regimens (drug administration protocol) and doses have been developed, violation of which leads to treatment failure and adverse events.
Currently, the CGRP antagonists erenumab, fremanezumab and galcanezumab and eptinezumab are actively used in the treatment of chronic migraine.
Methods for headaches
The method of dealing with a situational illness depends on the cause. If you know for sure that the main organ is “cracking” after alcohol, there will be one approach, if you are not entirely sure of the source of poor health, then another. It is useful to know all the methods, using one or the other depending on the situation.
Hot water
This method of dealing with headaches can rightfully be considered universal. The mechanism of action is very simple: hot water causes blood vessels to dilate, and a large amount of blood flows to the meninges at once. The spasm goes away, making you feel better in just a few minutes.
Cold and hot shower
A variant of the previous method of struggle.
Helps with:
- migraine;
- with a hangover;
- during attacks of VSD;
- children with increased intracranial pressure.
If you or your child are not used to the sharp contrast, it is not necessary to replace boiling water with ice water and vice versa. It is quite enough to alternate between lukewarm and very warm water; the procedure is carried out within ten to fifteen minutes. This time should be enough to establish blood circulation.
Stimulation of the Tang Yin point
You can believe in Chinese medicine or not, but it is almost five thousand years old and the Chinese are in no hurry to abandon it. And it’s not for nothing that there are almost two billion of them!
The indicated point for combating headaches is located in the area of the “third eye” - that is, on the bridge of the nose between the two existing ones. For the desired effect, you need to massage the area for about ten minutes, if possible, using sharp objects. If you don't have acupuncture needles, a regular pencil or pen point will do. There will be a trace of lead or ink left, but it’s not difficult to wash it off.
Neck massage
In children with intracranial pressure and adults with osteochondrosis, which is typical for every second office worker, pain and vascular spasms occur because the blood flow is compressed by the cervical vertebrae.
It is not difficult to alleviate the condition:
- Place your hands on your neck.
- Slowly begin massaging the collar area.
- If it hurts, be patient, it will soon get easier.
- The procedure should last five minutes or longer.
Additionally, you can sign up for therapeutic massage courses. They allow many people to get rid of unwanted symptoms for a long time.
Essential oil
Essential oils are a great way to combat various ailments. Aromatherapy is one of the most promising areas of medicine; adherents claim that with the help of odors you can get rid of even serious diseases. Whether it’s true or not is difficult to judge, but you can overcome the pain in your head. You will need lemon, lavender or peppermint essential oil.
- Place two or three drops on a cotton swab.
- Place a few cotton wool next to you.
- Breathe in the scent of essential oils for up to twenty minutes.
Gradually you will feel relief until you are completely relieved of your discomfort.
Chocolate bar
A common cause of migraines in schoolchildren, students and workaholic office workers is a simple lack of glucose in the blood. If in people suffering from type 1 diabetes, a lack of sugar is manifested by tremors, clouding of consciousness, even coma, then healthy people do not face such terrible consequences. But a hungry brain will still demand its way. It's time to forget a little about a healthy lifestyle and diet and “feed” the starving “gray matter”.
Walk in the fresh air
What do we breathe? That's right - dust, stale air, or, at best, what the air conditioner produces. All this is far from the concept of “freshness”.
Go outside - just not on a highway or a crowded avenue, but preferably at least in a park or square. Walk for about forty minutes to an hour. Fresh air will provide an influx of oxygen and saturate the blood with the most important element.
Strong tea or coffee
Only if you are prone to hypotension. It is worth remembering that low blood pressure, unlike high blood pressure, is not a disease, but can sometimes be a symptom of vitamin deficiency, iron deficiency anemia and other ailments. However, there are completely healthy people who simply have chronically low blood pressure and get headaches because of it. They can be advised to “treat themselves” with strong tea - preferably not from tea bags, but natural tea, oolong tea is absolutely fine. Or using natural coffee.
Ear massage
Another exercise from the field of Chinese medicine - and also very effective. In the ears, according to the philosophy of acupuncture, all the areas “responsible” for the body are located, so massage improves blood circulation and enriches the blood vessels of the brain with oxygen. It really works, tested by many headache sufferers.
Beam (cluster) headache
Cluster (bundle) headache (CHB, PHB) is the most common type of trigeminal (autonomous) autonomic cephalgia. The prevalence of CGD in the population is low - 0.1–0.4%; men suffer 3–4 times more often than women. The age peak of incidence in men occurs in the second decade, women have two peaks - from 15 to 20 years and from 45 to 50 years. Most patients have an episodic form of PHB (90% of all cases) with alternating periods of pain and remissions; Less common (up to 10%) is chronic CBG, when remissions are either absent altogether or do not exceed 1 month.
Symptoms of cluster headache (PHB).
Attacks of severe, strictly unilateral pain, orbital, supraorbital, temporal, or any combination of these sites, lasting 15–180 minutes and occurring anywhere from once a day to eight times a day. Pain is associated with ipsilateral conjunctival injection, lacrimation, nasal congestion, rhinorrhea, forehead and facial sweating, miosis, ptosis and/or eyelid edema, and/or restlessness or agitation.
Treatment
of cluster headaches
. Before prescribing therapy, the patient should be explained about the benign nature, possible prognosis of the course of the disease, the need to avoid potential provoking factors during the painful period (refusal of alcohol, medications and products with vasodilating properties, adherence to a sleep-wake schedule). Therapy includes relief of attacks and prevention of painful periods
To relieve attacks, triptans and inhalation of 100% oxygen are most effective, and to a lesser extent, local anesthetics (lidocaine, capsaicin); analgesics and opioids are not used.
Preventative treatment
should begin as soon as possible after the onset of the painful period. Even with a noticeable improvement during the first 1–2 weeks of therapy, patients should not interrupt the course: the duration of treatment should exceed the usual duration of pain bundles. Corticosteroids (prednisolone) and verapamil are most effective.
When to worry about a headache?
You can manage many types of headaches on your own, and your doctor can prescribe medication to control most headaches. But some headaches require immediate medical attention.
Here are some warning signs when you should be concerned about headaches:
- Headaches that first appear after age 50;
- Significant change in the nature of the headache;
- Severe “thundering” headache;
- Headache that gets worse with coughing or movement;
- Constantly worsening headaches;
- Headaches that are accompanied by fever, neck stiffness, confusion, decreased attention and memory, or neurological symptoms such as blurred vision, slurred speech, weakness and numbness in the extremities, or seizures;
- Headaches accompanied by painful redness of the eyes;
- Headaches after a blow to the head;
Headaches that interfere with normal daily activities.
What happens after I start treatment?
Once you start a treatment program, monitor how well it works. A headache diary can help you note any patterns or changes in how you feel. Remember that it may take you and your doctor some time to find the best treatment plan, so try to be patient. Be honest with him about what works for you and what doesn't.
Even if you are being treated, you should still avoid things that you know can trigger your headaches, such as foods or smells. It is important to adopt healthy lifestyle habits that will help you feel good, such as regular exercise, adequate sleep and a healthy diet. Also, schedule scheduled follow-up appointments so your doctor can see progress and make changes to your treatment program if you need them.