Myasthenia gravis is a chronic autoimmune disease that is characterized by abnormalities in neuromuscular transmission. As a rule, the activity of the facial muscles, eyes, and chewing muscles is disrupted. The disease is characterized by muscle weakness, pathological fatigue, and the presence of crises. The number of people suffering from this disease is constantly increasing. There is 1 patient with myasthenia gravis per 50,000 population.
Factors contributing to the development of pathology are:
- stress and emotional mental instability of a person;
- excessive physical activity;
- frequent ARVI;
- use of anticholinesterase drugs in high doses;
- load on the organs of vision.
If there is a predisposition to the development of myasthenia gravis and the presence of factors contributing to this, the disease develops very rapidly.
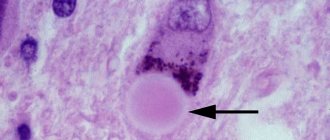
The main role in the causes of ocular myasthenia is attributed to diseases of the thymus gland. With the development of tumors in this organ, specific antibodies are often found in the patient’s bloodstream. They have the ability to destroy the thymus itself, as well as cells of striated skeletal muscles.
Antibodies, acting on muscle tissue, destroy the cell membrane. This disrupts the binding of receptors to acetylcholine, and makes it difficult to transmit nerve impulses to muscle fibers. Therefore, weakness and depression of the skeletal muscles occurs.
Symptoms of myasthenia gravis
The main symptom of myasthenia gravis is increased fatigue with prolonged muscle strain. At first, the muscles simply get tired, and then they completely cease to be controlled and “refuse” to work. After a long rest, the muscles regain functionality. Immediately after waking up, a person feels a surge of strength, but as a result of active muscle activity, they weaken again. In its manifestations, myasthenia gravis is similar to paralysis, however, unlike it, muscles tend to recover after rest.
During myasthenic crisis, rapid breathing, increased work of the heart muscle, and increased salivation are also observed. If the patient's respiratory muscles are affected, then the onset of a myasthenic crisis poses a threat to his life.
Myasthenia gravis is a progressive disease, so the patient’s condition worsens over time. In some cases, he may even become disabled.
Discussion
When thinking through the tactics of anesthesia, we proceeded from the need to comply with the following basic requirements: 1) minimizing the use of drugs that contribute to impaired respiratory function (muscle relaxants, opioids, anxiolytics), potentiating the effect of muscle relaxants (halogen-containing anesthetics, a number of antibiotics) or affecting NMP (magnesium preparations, fluorine-containing corticosteroids, etc.); 2) prevention of conditions that disrupt neuromuscular transmission (hypokalemia, hypocalcemia, acidosis, hypothermia, etc.); 3) reversal of NMB with minimal risk of developing cholinergic crisis; 4) early return to drug prevention of myasthenic crisis.
To solve the first problem, the option of combining general and epidural anesthesia was chosen. Many authors recommend not using muscle relaxants [7]. However, we assumed that such extensive abdominal surgery would not be possible without the use of muscle relaxants due to the impossibility of surgery, and our assumptions were confirmed. There is a recommendation for the use of volatile anesthetics to reduce the need for relaxants [2]. We chose the alternative option of using TVVA under the control of neuromonitoring, which, under conditions of accelerometry, makes NMB more predictable and controllable. Anxiolytics and opioids were excluded from the premedication and postoperative pain management regimen.
To solve the second problem, the acid-base state and plasma electrolytes were monitored intraoperatively with timely correction of shifts. A set of measures was used to prevent induced hypothermia. Interestingly, corticosteroids and AChE inhibitors, which are first-line drugs for the treatment of myasthenia gravis, can themselves induce myopathy [2, 6].
To solve the third problem, we had 2 options: use rocuronium followed by its neutralization with sugam-madex, or use cisatracurium followed by reversion with AChE inhibitors. With the advent of sugammadex in the anesthesiologist's arsenal, the use of the rocuronium-sugammadex combination in patients with myasthenia gravis is quite logical and can be considered preferable. In this case, a large number of previous abdominal operations significantly increased the risk of re-intervention (for bleeding, early acute adhesive intestinal obstruction, anastomotic leak, etc.). As is known, re-use of rocuronium is not recommended in the next 24 hours after using sugammadex. Data on the possibility of using rocuronium just a few hours after the use of sugam-madex [10] were obtained on volunteers and require clinical confirmation. It was these circumstances that kept us from using rocuronium and sugammadex. To reverse the effect of cisatracurium, we chose galantamine, an AChE inhibitor with a milder and longer-lasting effect compared to neostigmine [11]. The need to use anticholinesterase drugs is indicated in most recommendations. However, the lack of clear dosing regimens (bolus or infusion) always increases the risk of muscarinic effects up to myasthenic cholinergic crisis [1, 6]. In this case, the use of Nivalin after two anesthesias and in the early postoperative period was not accompanied by pronounced classic side effects of AChE inhibitors.
Maintenance and reversal of NMB during the first anesthesia was carried out under accelerometry control. At the stage of recovery of urinary tract, assisted ventilation in the BIPAP mode was used. This allowed the patient to be safely extubated in the operating room 40 minutes after the end of the operation. During the second anesthesia, accelerometry was not used, which may be one of the main reasons for the somewhat delayed recovery of muscle activity. This once again confirms the feasibility of using LUT monitoring for patients with myasthenia gravis.
After the use of muscle relaxants, weakness and fatigue are usually observed only in the muscle groups affected by the disease, while the respiratory and limb muscles recover quite quickly [12]. Our observation confirms this phenomenon: the patient experienced less difficulty breathing, squeezed his hand tightly, but was not immediately able to independently remove the secretion from the oropharynx. In this regard, it is necessary to carefully sanitize the oral cavity using vacuum suction, especially during decurarization.
This clinical observation demonstrates the features of perioperative management of patients with concomitant severe myasthenia. It is important to understand that the severity of the condition of such patients is determined not only by the severity of myasthenic symptoms, but also by the side effects of therapy. When surgically treating patients with concomitant myasthenia, it is necessary to individualize the risks of using all pharmacological agents, the likelihood of a decrease in the reparative properties of tissues and the occurrence of infectious complications. The consequences of general anesthesia are minimized with a rational choice of pharmacological agents, including drugs for reversing NMB, as well as the use of neuromuscular monitoring. Concomitant myasthenia gravis in itself should not be a reason for refusing the necessary surgical treatment.
Forms of myasthenia
Ocular myasthenia . The first sign of this form is drooping of the eyelid. The symptom appears due to disruption of the orbicularis oculi muscle. At first, the patient can open his eyes freely, only slight weakness is felt. Subsequently, constant blinking causes weakness of the muscle fibers innervating the eyeball.
Bulbar myasthenia . In this form of the disease, muscle fibers that are controlled by the bulbar group of nerves are affected. The person has problems chewing and swallowing food. Speech gradually changes - it becomes quiet, hoarse, with a nasal tint. Due to the progressive depletion of the muscle, speech may disappear altogether.
Generalized myasthenia gravis . This is the most common form. The work of the eye muscles is the first to be disrupted. As the disease progresses, other muscle groups also suffer. If there is a deviation in the functioning of the muscles of the face and neck, deep wrinkles appear in the forehead area, the smile line becomes distorted, and drooling increases. The next muscles to be affected are the muscles of the arms and legs. The patient feels well only in the morning. As a result of the progressive course of the disease, the muscle fibers atrophy, and the person stops walking.
Myasthenic crisis
As mentioned above, myasthenia gravis is a progressive disease. As the disease progresses, the patient's condition worsens, symptoms increase and become more severe, and muscle dysfunction becomes more pronounced. People who have suffered from myasthenia for a long time often experience myasthenic crisis. This is a sudden attack, as a result of which a sharp weakness of the pharyngeal and respiratory muscles appears, the functioning of the heart muscle is disrupted, and saliva flows heavily. Myasthenic crisis is a threat to life, so the condition of the myasthenic patient must be carefully monitored and timely assistance provided.
Myasthenia gravis
Signs
The disease usually begins with eye symptoms.
The sufferer develops ptosis and double vision. Moreover, in the morning there is less ptosis than in the evening. Gradually, it becomes difficult for a person to climb stairs, get out of a chair, or raise his arms up. During a long conversation, the patient’s speech is impaired, the voice becomes nasal, weakness of the tongue develops, and it becomes difficult to pronounce some letters, for example, “r”, “w”, “s”. However, after rest, these symptoms disappear. Swallowing problems may appear later. With generalized myasthenia gravis, breathing problems may develop. Sometimes a myasthenic crisis occurs - this worsens all the symptoms of the disease, including breathing problems.
Description
Myasthenia gravis was first described in 1672 by Thomas Willis. However, the cause of the disease is still unknown. It is assumed that the disease develops after acute respiratory viral infection or severe stress.
However, what happens with this disease is known. With myasthenia gravis, the body begins to produce antibodies against its own acetylcholine receptors on the postsynaptic membrane of neuromuscular synapses. But it is still unknown where exactly these antibodies are formed and what provokes their appearance.
The acetylcholine receptor is a structure in the cell that receives external information transmitted to the cell. These receptors are located in groups on the cell. Information is transmitted using acetylcholine. It attaches to the receptor, under its action the receptor changes its configuration and thereby transmits some information to the cell. In particular, acetylcholine is involved in the transmission of nerve excitation in motor nerves. When antibodies attack receptors, their number decreases, so neuromuscular transmission worsens.
Myasthenia gravis can affect adults and children of any age, but it is more often registered in women 20-40 years old. But it rarely happens in children.
According to the nature of the course of the disease, they are distinguished:
- myasthenic episodes, when episodes of weakness are short-term, and the intervals between them can reach several years;
- myasthenic condition, which develops quickly, over several months, but then does not progress for many years, remaining at the same level;
- a progressive form of myasthenia, which develops slowly, in some cases its progression may even stop;
- a malignant form of myasthenia, which develops very quickly, involves many muscles, often affecting the respiratory muscles.
Often with myasthenia gravis in adolescents, children and young adults, thymic hyperplasia is detected. And approximately 10% of older patients are diagnosed with malignant thymoma (tumor of the thymus gland).
A woman suffering from myasthenia gravis should become pregnant only after consulting a doctor, since the child may inherit antibodies to acetylcholine receptors that the mother’s body has produced. Although a woman's condition rarely worsens after pregnancy, it usually improves.
First aid
First aid is necessary for myasthenic crisis, as breathing is impaired. The patient must be urgently hospitalized and connected to a ventilator.
Diagnostics
It is believed that myasthenia gravis is a rare disease: 1 person per 10,000 population. However, some experts doubt that the disease is so rare, since they consider confirmed cases of the disease, and diagnosing myasthenia gravis is very difficult, since its manifestations appear and disappear. And to make a correct diagnosis, you need to carefully examine the patient.
To make a diagnosis of myasthenia gravis, the following is usually done:
- clinical examination;
- needle electromyography;
- proserine test (after administration of proserine, the symptoms of a person suffering from myasthenia decrease sharply);
- blood test for antibodies to acetylcholine receptors;
- blood test for thyroid hormones;
- computed tomography of the thymus gland.
Myasthenia gravis is differentiated from meningitis, polymyositis, ocular myopathy, and cerebrovascular accident.
After a diagnosis of myasthenia gravis is made, the patient must be carefully examined, since this disease may have concomitant autoimmune diseases - thyrotoxicosis, polymyositis, rheumatoid arthritis, systemic lupus erythematosus.
Treatment
The main task in the treatment of myasthenia gravis is the correction of neuromuscular transmission. For this it is important to increase the amount of acetylcholine. Typically, anticholinesterase drugs are used, which inhibit the enzyme that hydrolyzes (decomposes) acetylcholine. The dose of the medicine is selected individually.
If necessary, for example, in case of a malignant tumor of the thymus gland, a thymectomy is performed, that is, its removal. However, X-ray therapy (a type of radiation therapy in which X-rays are used to irradiate an organ or limited area of the body) or corticosteroids can often be used.
Previously, with myasthenia gravis, death with myasthenia was 30-40% of cases, but now the mortality rate is about 1%. But despite this, the disease requires long-term serious treatment.
Prevention
With myasthenia gravis, excessive physical activity and prolonged exposure to the sun are contraindicated. In addition, there are many drugs that cannot be used for myasthenia gravis. These are magnesium preparations, antipsychotics and tranquilizers, diuretics, except for spironolactone, antibiotics of the fluoroquinolone and aminoglycoside groups and some others. Therefore, before starting to take any medicine, a person suffering from myasthenia gravis should consult a doctor.
© Dr. Peter
FAQ: Can myasthenia gravis be cured?
Myasthenia gravis is a chronic disease. With its treatment, you can achieve only lasting improvement, sometimes with the disappearance of all symptoms. This is called remission. It can last for several months or even years. It may even last until the end of life, but this does not mean that the disease has passed, since when taking certain medications or under stress there is a very high probability of its exacerbation.
FAQ: Can you get myasthenia gravis?
No, this is not an infectious disease, and it is not transmitted from a sick person to a healthy one.
FAQ: Why do myasthenic crises occur?
With proper treatment and compliance with all doctor’s recommendations, myasthenic crises are extremely rare. They usually occur when taking illegal drugs or improper treatment.
Diagnosis of myasthenia gravis
The diagnosis of ocular myasthenia gravis is made on the basis of a complete clinical and laboratory examination, which includes the following methods:
- Study of patient complaints.
- External examination of the affected areas.
- Cooling test: Ice is placed on the patient's eyelids and the functioning of the eye muscles is observed. This test is considered positive if the function of the eyelids is restored for a short period of time.
- Test with proserine. The patient is injected with a 0.05% solution of this drug subcutaneously in an amount of 2-3 ml. The test is positive if 30 minutes after administration the function of the eyelid muscles is restored. The effect of proserin lasts about 3 hours, then ptosis returns.
- Electromyography, a study based on the study of muscle function during rhythmic stimulation.
- Blood test for the presence of characteristic antibodies: to titin and acetylcholine receptors.
- CT scan of the anterior mediastinum, which examines the condition of the thymus gland. This type of study is used because of the possible connection between the development of myasthenia gravis and the presence of tumor formations in this organ
Read also
Aphasia
Aphasias are speech defects that appear with minor brain damage, most often affecting the left hemisphere in right-handed people, and consisting of various forms of speech changes.
Location and size… Read more
Polyneuropathy
Diabetic polyneuropathy is a pressing problem for patients with diabetes. Diabetic polyneuropathy is a serious complication of diabetes mellitus. The incidence of polyneuropathy is 26-50%...
More details
Consequences of traumatic injuries to the skull, spine, brain and spinal cord
Traumatic brain injuries, or traumatic brain injuries, are damage to the brain that impair brain function. Brain injuries are divided into two large groups - closed...
More details
Chiari malformation
What is Chiari Malformation? Chiari malformation (formerly Arnold-Chiari malformation) is a congenital defect of brain development that involves the dislocation of the cerebellar tonsils into the spinal canal through the large…
More details
Clubfoot
Clubfoot should not be understood as just one foot disorder. This is a group of deformities of the foot and ankle joint with their pathological setting. Clubfoot is a deformity in which...
More details
Treatment of myasthenia gravis at different stages
How to treat ocular myasthenia? This question remains open to this day, since the exact causes of this disease have not been fully elucidated. We can say with certainty that a complete cure for this pathology cannot be achieved. Patients are offered lifelong maintenance therapy to put the disease into remission.
The drug Calamine has received a huge number of positive reviews in the treatment of ocular myasthenia. It belongs to the group of anticholinesterase drugs. Use this remedy 1 tablet three times a day.
Also, when treating the disease in the early stages, the following medications can be prescribed:
- antioxidants;
- potassium preparations;
- B vitamins.
If the patient's condition worsens, it is recommended to prescribe hormonal drugs in large doses. This method is called “pulse therapy”. Prednisolone is prescribed in a total dose of up to 2000 mg. The drug has a fairly strong effect on the cardiovascular system, kidneys, and endocrine glands, so constant monitoring by a therapist is required. Cancellation of prednisolone occurs with a gradual reduction in dose.
Also, when the ocular form becomes generalized, it may be necessary to take cytostatics - Cyclosporine, Azathioprine.
Immunoglobulin plays a special role in the treatment of ocular myasthenia. It is able to slow down the development of autoimmune processes and reduce the effect of antibodies on muscle tissue. This drug is administered dropwise into a vein, 5-10 g per day, course dose is 30 g.
Severe forms of myasthenia gravis require plasmapheresis, which helps cleanse the blood of pathological antibodies. This procedure is carried out for 5-7 days.
If the cause-and-effect relationship between the development of the disease and the presence of a thymic tumor is reliably known, surgical treatment is performed - thymectomy.
Treatment
Taking into account the pathogenetic mechanism of the development of myasthenia gravis, the proven and simplest method of treating patients with myasthenia gravis is the use of ACEP. Currently, drugs such as tenzilon, proserin, and kalimine are widely used in clinical practice for myasthenia gravis. They differ mainly in the duration of action: tensilone for several minutes, proserin for 2–3 hours, kalimine for 4–5 hours.
Ubretide, as a rule, is not used due to the formation of a cumulative effect and the development of a cholinergic crisis. Tensilon is used for diagnostic purposes only. Prozerin is used when quick action is needed. Kalimin is often preferred.
Dosing principle: the next dose is taken 30 minutes before the end of the previous dose. When transferring patients to parenteral administration of drugs, it is necessary to take into account that 1 tablet of kalimine (60 mg) is equivalent to 1 ml of a 0.05% solution of proserin.
In some situations (mensis, infections, remission) sensitivity to ACEP increases. In this case, the dose of drugs should be reduced.
Patients should be taught to adjust the dose individually depending on the course of the disease.
Relative contraindications to the use of ACEP:
- bronchial asthma;
- severe atherosclerosis;
— IHD, angina pectoris;
- epilepsy.
Prozerin acts in 20–40 minutes, duration of action is 2–4 hours. Release forms: tablets of 15 mg, ampoules of 0.05% solution of 1 ml. It is undesirable to use it for basic therapy, since it is a short-acting drug and has high toxicity.
Kalimin begins to act after 60 minutes and retains its effect for 4–6 hours. Release forms: tablets 60 mg, ampoules of 0.5% solution 1 ml. The drug is taken at intervals of 5–5.5 hours.
When using ACEP, potassium preparations are additionally prescribed, since the latter prolong the effect of ACEP. A diet rich in potassium (baked potatoes, dried apricots, bananas, etc.) is recommended. Potassium-sparing drugs are used (veroshpiron 25 mg, 1 tablet 2 times a day, potassium chloride - 3.0 g per day in solutions, powders, tablets) to prevent an overdose of ACEP.
Forecast
Even in the last century, myasthenia gravis was considered a rather serious disease, as a result of which about 40% of patients died. At present, with the use of modern approaches to the treatment of this disease, mortality is only 1% of all patients.
Myasthenia gravis is considered a localized form of the disease. However, if the patient does not receive appropriate treatment, then, according to statistics, over the next two years, 50% of patients will develop a generalized form.
With timely and correct treatment, the number of patients who experience stable remission of the disease is about 80%. In this case, the patient must still remain under the constant supervision of doctors and follow all their recommendations, since ocular myasthenia is considered a chronic and not completely curable disease.
Treatment of myasthenia gravis
Specific medications (of which there are many) should be avoided or used with caution (especially certain antibiotics) that may worsen myasthenia gravis or interfere with medications used in its treatment.
Thymectomy (removal of the thymus gland) may increase the chances of improvement or remission. It is recommended for patients with thymoma. Without thymoma, thymectomy is an option and may be effective in cases where anti-AChR autoantibodies are elevated.
Acetylcholinesterase inhibitors (AChEIs), such as pyridostigmine and neostigmine, are the first line of treatment for myasthenia gravis, regardless of its subtype.
For more severe disease or if AChEIs do not work, immunosuppressive therapy is recommended: oral corticosteroids (prednisolone, prednisone, methylprednisolone) and other immunosuppressive drugs (azathioprine, cyclosporine, mycophenolate mofetil, rituximab, cyclophosphamide, methotrexate, tacrolimus).
In case of myasthenia gravis crisis (severe exacerbations), intravenous immunoglobulins, plasmapheresis and plasma exchange are used.
Soliris (eculizumab), an anti-C5 monoclonal antibody from Alexion Pharmaceuticals, improves symptoms of refractory myasthenia gravis and is approved for the treatment of generalized myasthenia gravis with AChR autoantibodies.
Prevention of relapse
When the main treatment is over and remission has already been achieved, it is important to take care of relapse prevention. The patient will have to adhere to certain rules: give up bad habits, lose weight if obesity occurs, adjust the diet, enriching it with foods containing vitamins and microelements. Traditional medicine is also used for preventive purposes. Forecast and consequences
Myasthenia gravis is an insidious disease that until recently was considered almost incurable and even fatal. However, today the situation is not so sad. Thanks to modern medications, the disease can be successfully cured and stable remission achieved. The patient's further life differs little from the life of completely healthy people.
This disease does not require hospitalization (except for surgical treatment). The therapy is carried out on an outpatient basis, but nevertheless, the specialist will carry out constant monitoring and carefully monitor the dynamics. Myasthenia gravis is a disease that cannot be neglected. High-quality treatment and strict adherence to the specialist’s instructions are the key to success. Almost 90% of patients who started therapy in a timely manner successfully cope with the disease and continue to lead their usual lifestyle, the quality of which, as a rule, does not suffer. If the disease is not treated, the consequences can be dire.