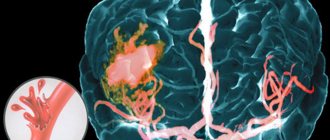
Based on modern ideas about the mechanisms of development of ischemic stroke, neurologists at the Yusupov Hospital identify 2 main directions of pathogenetic therapy: improving the perfusion of brain tissue (the passage of blood through them) and neuroprotection (a set of measures aimed at improving the biochemical and restorative properties of the nerve cell).
Complex therapy of ischemic cerebral stroke
It is known that in the absence of adequate therapy, approximately 2 million neurons die within ten minutes of ischemia. Each stage of the ischemic cascade is a potential target for therapeutic intervention. The earlier neuroprotective treatment is started, the greater the chances of success, the less the degree of damage to the brain substance.
Doctors at the Yusupov Hospital begin complex therapy for ischemic stroke immediately after the patient is admitted to the neurology department and an accurate diagnosis is established. Neurologists draw up treatment regimens for patients with cerebral infarction individually, taking into account which vessel has impaired blood flow, the size of the ischemic focus, and how damaged the nerve cells around the area of cerebral infarction are. Due to the fact that the clinic conducts research on modern drugs for the treatment of acute cerebrovascular accidents, patients at the Yusupov Hospital have the opportunity to receive the most modern drugs.
Drug treatment of acute ischemic stroke includes basic and specific therapy. Basic therapy consists of:
- measures to support respiratory and circulatory functions;
- correction of metabolic disorders and the volume of circulating fluid;
- blood pressure control.
The main goal of intensive care is to prevent oxygen deprivation of brain tissue and the associated increase in brain damage. To ensure adequate water-electrolyte balance and blood flow, doctors at the Yusupov Hospital provide infusion therapy to patients with ischemic stroke. The purpose of infusion therapy is:
- achieving blood thinning;
- maintaining adequate cerebral perfusion pressure (a physiological indicator characterizing the level of blood supply) not lower than 70 mm Hg. Art. to eliminate ischemia and oxygen starvation of neurons;
- correction of electrolyte disturbances, primarily high or low sodium levels in the blood.
Doctors at the Yusupov Hospital achieve a normal level of cerebral perfusion pressure in patients with ischemic stroke by increasing systemic arterial pressure and decreasing intracranial pressure. To increase blood pressure, crystalloid solutions and sympathomimetics are administered intravenously.
In case of ischemic stroke, doctors at the Yusupov Hospital maintain the patient’s circulating blood volume at the proper level and prevent the development of hypovolemia, which increases the risk of low blood pressure and reduces central perfusion pressure. These changes in the equilibrium of the internal environment of the body lead to vasodilation and increased intracranial pressure.
To maintain the overall water-electrolyte balance and ensure sufficient blood flow in the cerebral vessels, patients with ischemic stroke in the neurology clinic are administered 30-35 ml/kg/day of fluid. Patients who, upon admission to the Yusupov Hospital, have low blood pressure, elevated hematocrit, dry mucous membranes and no decompensated heart failure, are prescribed infusion therapy in a volume of 1000-1500 ml of Ringer's solution or 0.9% sodium chloride solution. Patients with developed cerebral edema are maintained in a negative water balance.
Antiplatelet therapy for ischemic stroke: problems and prospects
This situation can be illustrated using the American Heart Association Stroke Guidelines (2011), according to which clopidogrel is no less effective than ASA and ASA in combination with modified-release dipyridamole in secondary stroke prevention. At the same time, this combination therapy differs only slightly in its beneficial effect from ASA monotherapy, but has such a significant side effect for the patient as headache. In terms of safety, clopidogrel, in turn, is slightly superior to ASA or ASA + dipyridamole in terms of the incidence of hemorrhages. Finally, a number of patients are advised to take clopidogrel or clopidogrel in combination with ASA (for example, after stenting surgery). If we take into account the cost of treatment, then the undisputed leader here is ASA. Let's consider some of the nuances of antiplatelet therapy for ischemic stroke. Variability of response to antiplatelet therapy. Increasingly, the term “resistance to antiplatelet therapy” is used to describe a situation where antiplatelet therapy prescribed to a patient to prevent cardiovascular complications is ineffective. Resistance, or poor response to treatment, is defined clinically when a patient taking ASA or clopidogrel at a therapeutic dose develops an ischemic event, or based on laboratory data. It is the results of laboratory tests that are given special attention, since they allow us to assess the possible response to treatment with a specific drug in a specific patient. However, available antiplatelet sensitivity tests have a number of significant limitations that must be taken into account when interpreting their results. Resistance to antiplatelet agents can develop due to several reasons, the main of which are shown in Table 1. Laboratory signs of resistance to ASA are detected in 5–60% of patients. This variation is due to the use of different methods to assess platelet function. In vitro, response to ASA is assessed by testing thromboxane A2 or platelet functions that are mediated by thromboxane, such as by measuring the light transmittance of a platelet suspension exposed to thromboxane A2, ADP, or collagen. This test is the “gold standard” for determining platelet aggregation properties. When assessing sensitivity to ASA, the optimal stimulator of aggregation is the precursor of thromboxane A2 - arachidonic acid, and when using other aggregation agonists, test results should be interpreted with caution, because they can activate aggregation through other mechanisms that are less dependent on COX-1. In addition, this test has poor reproducibility, and results vary by patient age, race, sex, and hematocrit. Sensitivity to clopidogrel is also influenced by a number of factors, and the prevalence of resistance to this drug ranges from 4 to 30%. As with ASA, this indicator is largely dependent on the laboratory method of assessing platelet function. Similarly, the gold standard for determining sensitivity to clopidogrel is to measure the light transmittance of a platelet suspension assessed before and after clopidogrel administration. In addition, less common methods such as thromboelastography, platelet receptor P2Y12 function testing, and vasodilator-stimulated phosphoprotein (VASP) assessment by flow cytometry may be used to assess platelet function. Laboratory diagnosis of antiplatelet resistance is difficult for a number of reasons, the leading of which is the lack of a comprehensive, reliable and validated method for assessing platelet function. The results obtained using different methods cannot be compared, since the different physiological mechanisms of thrombus formation are taken into account to varying degrees. There is no test that can take into account hydrodynamic factors, intercellular interactions, the effect of biological mediators and a huge number of other reasons that influence aggregation. Thus, the currently existing laboratory methods for assessing platelet aggregation represent a model that is very far from the processes occurring in vivo. In addition, the response to therapy may vary over time for each patient. In this case, one should take into account concomitant conditions such as inflammation or stress, which can lead to an increase in platelet formation and enhance extraplatelet synthesis of thromboxane. Therefore, a single assessment of resistance may have insufficient prognostic and diagnostic value. Finally, there is a view that response to therapy follows a normal distribution, and patients with resistance and excess sensitivity to antiplatelet agents correspond only to the extreme ends of this function. So, due to significant limitations of currently available laboratory methods for assessing platelet function, they cannot be recommended for routine use when choosing antiplatelet drugs for stroke prevention. The activity of clopidogrel depends on genetic factors and concomitant therapy. The point of application of clopidogrel, prasugrel and ticagrelor is the ADP receptor P2Y12, which inactivates the GPIIb/IIIa fibrinogen receptor involved in platelet aggregation. However, only about 15% of clopidogrel when taken orally undergoes bioactivation to form the active drug using isoenzymes of the cytochrome P450 (CYP) system - CYP 2C19 and CYP 3A4. The polymorphism of the CYP 2C19 gene is represented by 3 alleles, 2 of which do not provide normal metabolism of clopidogrel. In accordance with this, if there are 2 “non-functioning” alleles, metabolism is considered “impaired” (occurs in 12-20% of people), and if there is 1 “non-functioning” allele, it is considered “partially impaired”. A number of studies have been conducted to determine the effect of genetic polymorphism on the clinical effect of clopidogrel treatment. In general, it was found that “disturbed” metabolism is of clinical significance, which is manifested by an increased risk of vascular complications. As a means of overcoming insensitivity to clopidogrel in such patients, it was proposed to increase its dose (600 mg/day as a loading dose on day 1, then 150 mg/day for 6 days and 75 mg/day thereafter ), however, there are clinical differences between this treatment regimen and the usual regimen of clopidogrel (600 mg/day – loading dose and 75 mg/day – subsequently), as well as ASA in high (300–325 mg/day) and low (75–100 mg/day) doses were not identified. There was no effect of the described polymorphism on the effectiveness of prasugrel and ticagrelor. In summary, it should be assumed that routine genetic testing for platelet function while taking clopidogrel for stroke prevention is inappropriate, and if this is ineffective, it is optimal to replace it with ASA (as monotherapy or in combination with dipyridamole). Another problem associated with the activity of clopidogrel is that some proton pump inhibitors, like clopidogrel, are metabolized by the CYP 2C19 isoenzyme, as a result of which the effectiveness of the latter may be reduced. Particular concerns have been raised with omeprazole; pantoprazole and esomeprazole do not affect the metabolism of clopidogrel. However, clinical studies have shown that the use of proton pump inhibitors does not increase the incidence of recurrent stroke. New antiplatelet drugs: are they suitable for stroke prevention? The development of recurrent stroke, despite antiplatelet therapy, stimulates the search for new, more effective drugs with a more favorable pharmacokinetic and pharmacodynamic profile. Such drugs are prasugrel and ticagrelor. Prasugrel is a thienopyridine derivative that, like clopidogrel, inhibits platelet aggregation by irreversibly binding to the P2Y12 receptor. Its activity does not depend on genetic polymorphism, and it has a more powerful, rapid and lasting effect compared to clopidogrel. This was confirmed clinically - in a study of patients with acute coronary syndrome who underwent percutaneous angioplasty, prasugrel was more effective in preventing myocardial infarction than clopidogrel, but the safety results were not in favor of prasugrel, which was associated with a higher incidence of hemorrhagic complications , especially in patients who have had a stroke or TIA. Prasugrel has not been approved for secondary prevention of stroke. Ticagrelor is a reversible P2Y12 receptor inhibitor that inhibits platelet aggregation more strongly and rapidly than clopidogrel. In a study of patients with acute coronary syndrome, the incidence of ischemic stroke did not differ between the clopidogrel and ticagrelor groups, but the incidence of fatal intracerebral hemorrhage was higher with the latter drug. In summary, the results from the prasugrel and ticagrelor studies support the conclusions from the MATCH and CHARISMA studies that more aggressive antiplatelet therapy may not provide additional benefit in secondary stroke prevention along with an increase in bleeding complications. Conclusion. Selection of optimal antiplatelet therapy. Antiplatelet therapy is a key approach to the pharmacological prevention of atherothrombotic ischemic stroke. The effectiveness of the three main antiplatelet drugs is comparable, and any of them can be used as initial therapy, but therapy should be adjusted based on drug tolerability, comorbidities, cost of treatment, and patient preferences. Taking into account the above factors, ASA remains one of the most popular antiplatelet drugs, which is characterized by the most studied safety and tolerability profile. The existing dosage form of ASA (75 and 150 mg) in combination with a non-absorbable antacid - magnesium hydroxide (the drug Cardiomagnyl) - avoids the adverse effect on the gastric mucosa, which is especially important during long-term antiplatelet therapy; At the same time, the absorption of ASA and its further effect do not change. Dual antiplatelet therapy (with the exception of ASA and modified-release dipyridamole) is not preferred in most patients with stroke. Perhaps in the future, a personalized approach to preventive therapy and identification of patients with possible resistance to treatment will become possible, which will allow for optimal selection of strategies for primary and secondary prevention of stroke.
Literature 1. Domashenko M.A., Tanashyan M.M. Antiplatelet drugs in the treatment and prevention of cerebrovascular diseases // RMZh.. - 2008. - T. 16, No. 9 (339). – S. 1982–1987. 2. Domashenko M.A., Tanashyan M.M. Clopidogrel in the treatment and prevention of cerebrovascular diseases // Farmateka. – 2009. – No. 7 (181). – pp. 26–31. 3. Stroke: diagnosis, treatment, prevention / Ed. BEHIND. Suslina, M.A. Piradova. – M.: MEDpress–inform, 2008. – 288 p. 4. Cardioneurology / Ed. BEHIND. Suslina, A.V. Fonyakina. – M.: IMA-PRESS, 2011. – 264 p. 5. Suslina Z.A., Tanashyan M.M., Domashenko M.A. Antithrombotic therapy of ischemic cerebrovascular accidents from the perspective of evidence-based medicine, 2nd ed. – M.: Medical Information Agency LLC, 2009. – 224 p. 6. Suslina Z.A., Tanashyan M.M., Umarova R.M. Clopidogrel for ischemic cerebrovascular diseases // Treatment of nervous diseases. – 2003. – No. 4. – P. 14–18. 7. Tanashyan M.M., Domashenko M.A. Antiplatelet agents in the secondary prevention of ischemic stroke in patients with multifocal atherosclerosis // Breast Cancer. – 2010. – T. 18, No. 26 (339). – pp. 1549–1551. 8. Angiolillo DJ, Suryadevara S, Capranzano P et al. Antiplatelet drug response variability and the role of platelet function testing: a practical guide for interventional cardiologists // Catheter. Cardiovasc. Interv. 2009. Vol. 73(1). P. 1–14. 9. Bornstein NM, Karepov VG, Aronovich BD et al. Failure of aspirin treatment after stroke // Stroke. 1994. Vol. 25(2). P. 275–277. 10. Dawson J, Quinn T, Rafferty M et al. Aspirin resistance and compliance with therapy // Cardiovasc. Ther. 2011. Vol. 29(5). P. 301–307. 11. De Berardis G., Lucisano G., D'Ettorre A. et al. Association of aspirin use with major bleeding in patients with and without diabetes // JAMA. 2012. Vol. 307(21). P. 2286–2294. 12. Furie KL, Kasner SE et al. American Heart Association Stroke Council, Council on Cardiovascular Nursing, Council on Clinical Cardiology, and Interdisciplinary Council on Quality of Care and Outcomes Research. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American heart association/American stroke association // Stroke. 2011. Vol. 42(1). P. 227–276. 13. Goldstein LB, Bushnell CD et al. American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Epidemiology and Prevention; Council for High Blood Pressure Research,; Council on Peripheral Vascular Disease, and Interdisciplinary Council on Quality of Care and Outcomes Research. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association // Stroke. 2011. Vol. 42(2). P. 517–584. 14. Halawani SH, Williams DJ, Adefurin A. et al. Aspirin failure in patients presenting with acute cerebrovascular ischaemia // Thromb. Haemost. 2011. Vol. 106(2). P. 240–247. 15. Kastrati A. New anti-platelet agents: The end of resistance? // Thrombosis Research. 2012. Vol. 130. S.53–S.55. 16. Krasopoulos G., Brister SJ, Beattie WS, Buchanan MR Aspirin “resistance” and risk of cardiovascular morbidity: systematic review and meta-analysis // BMJ. 2008. Vol. 336(7637). P. 195–198. 17. Kuliczkowski W., Witkowski A., Polonski L. et al. Interindividual variability in the response to oral antiplatelet drugs: a position paper of the Working Group on antiplatelet drug resistance appointed by the Section of Cardiovascular Interventions of the Polish Cardiac Society, endorsed by the Working Group on Thrombosis of the European Society of Cardiology // Eur . Heart J. 2009. Vol. 30(4). P. 426–435. 18. Moonis M., Padma Srivastava MV (eds). Controversies in Stroke Care. – Byword Books Private Limited, 2012. – 342 p. 19. Seok JI, Joo IS, Yoon JH et al. Can aspirin resistance be clinically predicted in stroke patients? // Clin. Neurol. Neurosurg. 2008. Vol. 110(2). P. 110–116. 20. Thiagarajan P., Jankowski JA Aspirin and NSAIDs; benefits and harms for the gut // Best Practice. Res. Clin. Gastroenterol. 2012. Vol. 26(2). P. 197–206. 21. Wallentin L., Becker RC PLATO Investigators. Ticagrelor versus clopidogrel in patients with acute coronary syndromes // N. Engl. J. Med. 2009. Vol. 361(11). P. 1045–1057. 22. Weber R., Weimar C., Diener H.–C. Antiplatelet agents in stroke prevention: acute and long–term treatment strategies // Hamostaseologie. 2009. Vol. 29(4). P. 326–333. 23. Wiviott SD, Braunwald E. TRITON–TIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes // N. Engl. J. Med. 2007. Vol. 357(20). P. 2001–2015. 24. Yeung J., Holinstat M. Newer agents in antiplatelet therapy: a review // J. Blood Med. 2012. Vol. 3. P. 33–42.
Treatment of ischemic cerebral stroke with neuroprotectors
Currently, there are many drugs that have a neuroprotective effect. Doctors at the Yusupov Hospital use only neuroprotectors, the effectiveness of which has been proven by scientific research, to treat ischemic stroke. One of these drugs, which has the most versatile mechanisms of action in relation to oxidative stress (damage to brain cells as a result of oxidation) and a wide evidence base for ischemic stroke, is EMHPS (ethyl-methyl-hydroxypyridine succinate).
In this case, based on clinical experience in the use of EMGPS, the following scheme for its administration is used:
- at the prehospital stage, 400 mg is administered intravenously as a bolus once;
- in the acute period of ischemic stroke (up to 14 days), 5 mg/kg/day is administered intravenously, but more than 800 mg/day;
- during the recovery period (within 14 days), 400–800 mg of the drug 2-3 times a day is administered intramuscularly or intravenously.
One of the mechanisms of the damaging effect of ischemia is cholinergic insufficiency. With pathology of cerebral vessels, the number and size of cholinergic neurons in brain structures decreases. Neurologists at the Yusupov Hospital use the following regimen for the use of choline alfoscerate for acute ischemic stroke: for the first 3-7 days, 1000 mg is administered intravenously 2 times a day, and from the second week they switch to taking 400 mg of the drug per day 2 times a day (course of treatment - 2 month).
The combination of ethyl-methyl-hydroxypyridine succinate and choline alfoscerate in the context of ischemic stroke allows doctors at the Yusupov Hospital to fully influence the fundamental mechanisms of the development of clinical symptoms associated with ischemia and cholinergic insufficiency.
Drugs with proven effectiveness in ischemic stroke include the cerebroprotector Citicoline. Doctors at the Yusupov Hospital use it for both primary and secondary neuroprotection. Primary protection of brain cells begins from the first minutes of ischemia and continues during the first three days of stroke, especially active during the first twelve hours. Secondary neuroprotection reduces the severity of long-term consequences of ischemia. Neurologists begin it 3-6 hours after the onset of a stroke and carry it out for at least seven days.
Drugs after ischemic cerebral stroke
In order to prevent recurrent acute cerebrovascular accident. Doctors at the Yusupov Hospital prescribe antihypertensive drugs to patients who have suffered an ischemic stroke. During your stay at the neurology clinic, cardiologists individually select the most effective drug and its dose. In some cases, it is recommended to take combination antihypertensive drugs.
If there is a depressive state, antidepressants are prescribed. They not only eliminate the patient’s feeling of fear, but also eliminate the negative symptoms that develop as a result of cerebrovascular accidents. If the patient has no contraindications, he is prescribed antiplatelet agents. These include:
- acetylsalicylic acid and its derivatives (Trombo-AS, Aspirin Cardio, Acecardol, Cardiomagnyl, Aspicor, CardiASK);
- ADP receptor blockers (Clopidogrel, Ticlopidine);
- phosphodiesterase inhibitors (Triflusal, Dipyridamole);
- glycoprotein receptor blockers (Lamifiban, Eptifibatide, Tirofiban, Abciximab);
- inhibitors of arachidonic acid metabolism (Indobufen, Picotamide);
- medicines based on the Ginkgo Biloba plant (Bilobil, Ginos, Ginkyo).
Some plants also have an antiplatelet effect: horse chestnut, blueberries, green tea, ginger, garlic. Vitamin E also falls into this category.
In order to receive treatment and rehabilitation after an ischemic stroke with modern drugs, call us by phone. You will make an appointment with a neurologist, who, after the examination, will select an individual treatment regimen. The collective decision on the choice of treatment method for the most severe patients with ischemic stroke is made by doctors of the highest category, candidates and doctors of medical sciences on an expert council.
Drugs for recovery after chemotherapy
As we have already mentioned, chemotherapy drugs attack not only tumor cells, but also healthy cells. After a course of treatment, different organs may be affected to varying degrees. This is a necessary evil that must be tolerated in order to destroy cancer cells.
For faster and more complete recovery after chemotherapy, each patient receives an individual treatment program. First of all, efforts are aimed at restoring blood composition, normalizing the functioning of the liver, kidneys, heart, and combating depression and other psycho-emotional problems.
The choice of drugs for rehabilitation treatment after chemotherapy is quite large. It is important not to forget about such “boring” measures as proper lifestyle, nutrition, adequate sleep and rest, and physical activity. Dietary supplements can also be useful, but if you decide to take them, you should first consult with your doctor.
Book a consultation 24 hours a day
+7+7+78